 |
Q:
A 38-year-old uninsured male presented, stating his right eye had been red for a week. Examination revealed best-corrected acuity of 20/60 OD with a cyclitic membrane, 10% hypopyon and 3+ to 4+ cell and flare. With few resources to pay for meds or labs, how should I treat him?A:
Uveitis management begins with an accurate description of the inflammation and often requires additional testing to determine underlying systemic, autoimmune or infectious disease. “A dilated fundus examination is necessary to determine the primary site of inflammation,” says Jessica Steen, OD, assistant professor of Nova Southeastern University in Fort Lauderdale.
Clinical clues can help to guide your diagnosis. However, first rule out intermediate or posterior uveitis, or even panuveitis. Since this is the first episode of unilateral anterior uveitis with severe inflammation (cyclitic membrane and hypopyon), Dr. Steen suggests asking about systems associated with HLA B27 positivity, Behcet’s disease or herpes.
“My basic laboratory evaluations for this patient would be a CBC with differential, HLA B27, chest X-ray, RPR and FTA-ABS, quantiferon gold (for tuberculosis) as well as consideration of Lyme antibody titer,” says
Dr. Steen. However, our patient declined these tests because of cost, which we carefully documented.
Treatment
The mainstay of initial therapy in anterior uveitis is a strong topical steroid with an aggressive dosing strategy. While Durezol (difluprednate 0.05%, Novartis) is our first choice, a branded medication may be unfeasible for uninsured patients. Generic prednisolone acetate 1% dosed at least hourly will typically provide adequate treatment.
“Once you have control of the inflammation, determine if the patient is ready for a slow, deliberate taper,” Dr. Steen says. Tapering a steroid too quickly could increase inflammation and result in a longer treatment course, increasing the risk of side effects.
Dr. Steen suggests lagging the taper way behind the improvement—only tapering when the 3+ to 4+ cell and flare has significantly improved. Even then, taper slowly.
For patients who show limited improvement with topical steroids, a short course of Medrol Dosepak (oral methylprednisone, Pfizer), or subconjunctival corticosteroid may be necessary. Extended delivery devices, such as the recently approved Dextenza plug (sustained-release dexamethasone 0.4mg, Ocular Therapeutix), can minimize the patient’s need for topical therapy; however, it’s only approved right now for the treatment of postoperative pain and inflammation (Figure 1). Using it alone would most likely not provide the anti-inflammatory effect needed for a primary uveitis.
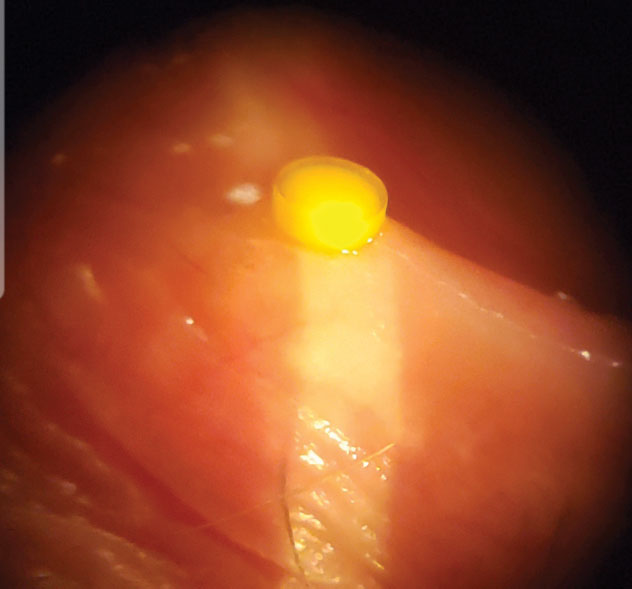 |
| Fig. 1. Dextenza could be a promising alternative or adjunct to drops in treating anterior uveitis. |
Manage Pressure and Pupils
With strong steroids dosed frequently, you might get the occasional intraocular pressure (IOP) spike. Continue your anti-inflammatory therapy as planned and add an IOP-lowering medication or combination agent. Dr. Steen’s choice is the fixed combination of dorzolamide 2% and timolol 0.5%.
Cycloplegic agents suppress ciliary body spasm, improving comfort and preventing posterior synechiae formation. For mild to moderate iritis, consider homatropine 5% every 12 hours. In advanced cases like our patient’s where synechiae have formed, have some 1% atropine and 10% phenylephrine on hand.
We provided our patient with the dilating drops and kept costs to a minimum using generic prednisolone. The hypopyon and cyclitic membrane resolved within a few weeks, and his vision improved to 20/25. Advise patients that it could take several months for complete resolution. We are hoping to run lab tests should he become insured but, meanwhile, will monitor him for any recurrences and re-treat if necessary.

