 |
A 35-year-old male presented with painless vision loss in his left eye since awakening that morning. The patient first went to an outside MD, where an anterior chamber paracentesis was performed and, then, he was referred to us.
The patient’s past medical history was significant for beta thalassemia minor, depression and hypothyroidism.
He was taking finasteride, bupropion and levothyroxine. He was a current everyday smoker. His systemic vital signs were normal.
His uncorrected visual acuity was 20/20 OD, 20/400 OS with pinhole improvement to 20/70 OS. His intraocular pressure (IOP) was 17mm Hg OD and 15mm Hg OS. Pupils were pharmacologically dilated from the earlier doctor visit and trace APD in the left eye was identified by reverse. Confrontation fields and extraocular motilities were all normal.
Anterior segment was unremarkable in both eyes; there was a temporal corneal anterior paracentesis track in the left eye.
Posterior segment of the right eye was normal; the left eye had optic nerve edema, superior macular large area of edema and infarction extending from the optic nerve to nasal border of fovea (Figures 1a and 1b).
OCT and OCT angiography (OCT-A) were obtained. They are available for your review in figures 2 and 3.
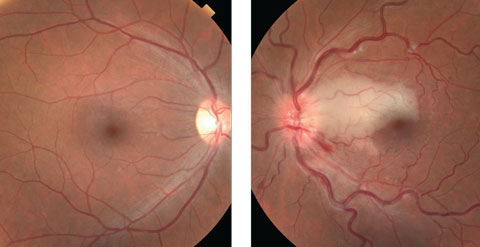 |
| Figs. 1a and 1b. Fundus photo of the right eye (at left) was normal, but the left eye (at right) shows a large optic nerve edema, superior to the macula and infarction extending from the optic nerve to the nasal border of fovea. Click to enlarge. |
Take the Retina Quiz
1. What type of vascular occlusion is most consistent with our patient’s left fundus findings?
a. Branch retinal artery occlusion
b. Central retinal artery occlusion
c. Branch retinal vein occlusion
d. Cilioretinal artery occlusion
2. Which of the following is not associated with cilioretinal artery occlusion?
a. Embolism.
b. Anterior ischemic optic neuropathy.
c. Hypotony.
d. Hypotension.
3. What are the OCT findings in the left eye?
a. Hyporeflectivity of the inner retina corresponding to intraretinal edema.
b. Hyperreflectivity of the inner retina corresponding to intraretinal edema.
c. Hyperreflectivity of the inner retina corresponding to exudates.
d. Subretinal fluid.
4. What is the most appropriate management for this patient?
a. Intravitreal antibiotics.
b. Immediate photodynamic therapy.
c. Observation.
d. Workup to identify underlying cause.
e. C and D.
Diagnosis
Our patient was an otherwise young, healthy individual before the onset of his left eye visual symptoms. History, clinical evaluation and imaging confirmed a diagnosis of cilioretinal artery occlusion (CLRAO) with impending central retinal vein occlusion (CRVO).
The retina is normally supplied by branches of the ophthalmic artery. In about 32% of eyes, a cilioretinal artery is present and arises from the posterior ciliary circulation. This is independent of the central retinal artery. In cases of central retinal artery occlusion (CRAO), the presence of an additional cilioretinal blood supply to the macula can help preserve central vision.
For answers, see below.
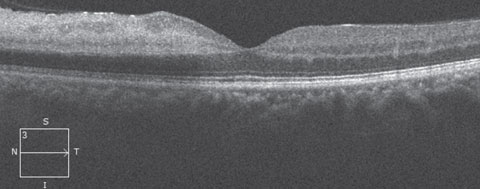 |
| Fig. 2. OCT of the patient’s left eye. Click to enlarge. |
Discussion
CLRAO was first described in 1968 and is an occlusion and infarction of retina supplied by the cilioretinal artery. Its etiologically is of three distinct types: Non-arteritic isolated CLRAO, arteritic CLRAO associated with giant cell arteritis (GCA) and CLRAO associated with CRVO) hemi-CRVO.2
Isolated non-arteritic CLRAO accounts for 5% of retinal artery occlusions.1 Systemic evaluation within this group revealed evidence of carotid atherosclerosis in 60% of patients.1 Other etiologies include: embolism, vasospasm, increased blood viscosity, hypercoagulable states, collagen vascular disease and hypotension. This condition has excellent visual prognosis—90% achieve 20/40 or better vision.1 Visual fields revealed scotomas with borders corresponding to the areas of obstruction. Scotomatous defects reduced in size at follow up visits.
Types
Arteritic CLRAO is a rare form of CLRAO. Exam findings for this entity include chalky white disc edema with associated characteristic retinal infarction on the area of ciliioretinal artery perfusion. It can also have posterior—rather than inferior—ischemic optic neuropathy. Arteritic CLRAO is often associated with GCA, and requires immediate workup and steroid treatment. It has poor visual prognosis and the goal is often to prevent visual loss in the fellow eye. The decreased visual acuity of this subgroup may primarily occur secondary to the optic neuropathy component.3
CLRAO is most commonly observed in the setting of CRVO. Often, vision loss is noticed on first awakening and a third of patients have a history of visual disturbances, possibly due to CLRAO or macular edema.4 Visual prognosis is good, as 70% of eyes improved to 20/40 or better.1 However, the severity of the CRVO plays a role in the visual prognosis. Systemic examination commonly reveals hypertension, diabetes, atherosclerotic disease and valvular cardiac disease. The risk factors of CRVO (and combined CLRAO and CRVO) are: acquired/inherited hypercoagulable states, myeloproliferative disorders, diabetes, hypertension, smoking, hyperlipidemia, increased intraocular pressure, oral contraceptives, volume depletion, renal failure and inflammatory disorders (Behcet’s syndrome, Wegener’s granulomatosis, sarcoidosis and Goodpasture’s syndrome).
Our patient’s risk factors included smoking and borderline homocysteine. Noncontributory medical history was hypothyroidism (TSH normal), beta thalassemia minor (since there is no evidence of iron overload that would cause end-organ damage) and his medications, finasteride and bupropion (which are not associated with any vascular occlusions in the literature). Given our patient’s time and onset of symptoms, risk factors and clinical presentation showing edematous optic nerve, engorged retinal veins, several flame-shaped hemorrhages and macular infarction corresponding to the cilioretinal artery, we suspected our patient had an impending CRVO with CLRAO.
OCT imaging of our patient reveals early hyper-reflectivity corresponding to intraretinal edema, and then late atrophy. The OCT angiography is quite interesting. Figure 3 shows a 3mm X 3mm composite of the superficial and deep retinal vascular layers. Here, we can see that there is good intensity, but the flow is compromised superiorly in the area of previous infarction in left eye.
Retinal arterial circulation can be obstructed at any point from the ophthalmic artery to the distal arterioles. The location of the obstruction determines the pattern of visual loss and clinical signs. The most common complaint is sudden, painless loss of central vision restricted to one eye. Thirty percent of symptoms occur upon awakening, which may be due to reduced retinal perfusion secondary to nocturnal hypotension.1
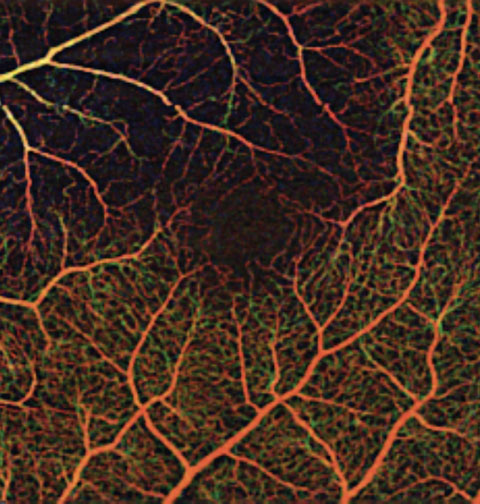 |
| Fig. 3. OCT Angiography of the patient’s left eye. |
Management and Treatment
Our patient was given 325mg of aspirin in office and was sent immediately to the nearest ER for stroke work up. In addition, our patient was required to get the following promptly: laboratory work (CMP, HLA-B27, D-dimer, HLA-B51, ESR/CRP, Anti ds-DNA, lipid panel, anti- CCP, ACE, anti-cardiolipin antibodies, ANA, ANCA, TSH, iron studies, HIV), hypercoagulable state, carotid doppler, ECHO, hematologist evaluation, neuroimaging and neuro consult.
Laboratory workup came out normal except for CBC Hb 12.5, MCV 62.5, hemoglobin electrophoresis consistent with beta thalassemia trait and borderline homocysteine.
Brain MRI, head/neck CTA and carotid Doppler were all normal. From these results, the patient was told to continue aspirin and clopidogrel. In addition, the rheumatologist started him on oral prednisone with slow taper for suspected vasculitis and collagen vascular disease.
One month from initial presentation, visual acuity OS improved to 20/20 and visual field showed a paracentral defect while off aspirin and with prednisone tapering. Four months from initial presentation, the patient’s visual acuity remained 20/20 in both eyes and visual field defect improved on clopidrogel and off prednisone.
Overall the prognosis of CLRAO combined with CRVO depends on type of CRVO (ischemic, nonischemic).2 Ischemic CRVO has more complications with possible neovascularization and, ultimately, poorer visual outcome. Nonischemic CRVO patients usually recover visual acuity of 20/40 or better in 70% of patients. Visual field defects (often paracentral) are due to CLRAO, and improve over time.1
No proven treatments for CLRAO exist. Management usually consists of observation, identification of the underlying cause and treating complications including macular edema and neovascularization when combined CRVO/CLRAO.5 Our patient was treated with AC paracentesis before presentation at BPEI. This may have been done to help lower the IOP which may allow the embolus to dislodge and move further downstream. Whether treatment over observation helped improve this patient’s visual outcome will remain unknown.
Despite the realization that these cilioretinal artery obstructions involve the macula, the visual prognosis is quite good.2 Even if a portion of the fovea is involved and the presenting visual acuity is poor, the vision usually improves over a period of days to weeks. Most likely an area of borderline hypoxia is present at the peripheral margins of the injured retina.5 It seems that the poorest prognostic sign is encirclement of the entire foveola by retinal opacification.
|
1. Brown G, Moffat K, Cruess A, et al. Cilioretinal artery obstruction. Retina. 1983;3:182–7. 2. Hayreh, S. Ocular vascular occlusive disorders: natural history of visual outcome. Prog Retin Eye Res. 2014 Jul;41:1-25. 3. Spierer O, Waisbourd M. Amaurosis fugax, anterior ischemic optic neuropathy and cilioretinal artery occlusion secondary to giant cell arteritis. Isr Med Assoc J. 2015;17(6):392-3. 4. Berkani Z, Kitouni Y, Belhadj A, et al. Cilioretinal artery occlusion and central retinal vein occlusion complicating hyperhomocysteinemia: a case report. J Fr Ophtalmol. 2013;36(7):e119-27. 5. Stoffelns B, Laspas P. Cilioretinal Artery Occlusion. Klin Monatsbl Augenheilkd 2015;232(4):519-24. 6. McLeod D. Central retinal vein occlusion with cilioretinal infarction from branch flow exclusion and choroidal arterial steal. Retina. 2009;29(10):1381-95. 7. Subash M., Balaggan K, Zambarakji H. Delayed cilioretinal artery occlusion after a hemiretinal vein occlusion. Int Ophthalmol. 2011;31(3):215-7. |

