As frontline eyecare providers, optometrists are tasked not only with diagnosing and managing various conditions, but also understanding and addressing the unique challenges faced by their patients. Glaucoma, a condition with a host of potential hurdles from psychological impacts and financial burdens to treatment adherence and lifestyle adjustments, is a perfect example of the important role ODs play in the overall health and quality of life of their patients.
Optometrists hold the key to managing the clinical aspects of glaucoma, and at the same time, fostering a supportive and empowering journey for those affected by it. In this article, we delve into the multifaceted challenges that glaucoma patients encounter, offering insights to help ODs provide tailored care and support as well as strategies and practical advice to improve the patient experience.
Contending With a New Diagnosis
Any medical condition comes with a variety of difficulties; however, a glaucoma diagnosis—a disease that causes irreversible vision loss—is particularly challenging for patients.
“Initially, as with the diagnosis of any chronic illness, I think there is denial, fear and uncertainty,” says Danica Marrelli, OD, clinical professor at the University of Houston, while noting that this is especially true with a condition like glaucoma, which often has no symptoms at the time of diagnosis. “It can be hard for patients to believe that they have it. They hear glaucoma and think, ‘I’m going blind.’ They can shut down and not really be able to hear or process what you are telling them, at least at first.”
The emotional toll of living with a chronic condition should not be underestimated, and glaucoma can have a significant psychological burden on patients. A strong support system will be a key component of success, and that begins with the eyecare team.
Optometrists can offer empathy, support and access to resources to help patients navigate these emotional challenges. Delivering information should be done confidently and compassionately, says James Fanelli, OD, founder and director of the Cape Fear Eye Institute in Wilmington, NC. “Look your patients in the eye and give them the one-on-one attention that shows you are invested in their care.”
When first diagnosing a patient with glaucoma, it is important to give them time to digest the news, says Andrew Rixon, OD, who practices at the Lt. Col. Luke Weathers, Jr. Medical VA Center in Memphis. “We need to acknowledge how they are feeling in that moment and be careful not to share too much information all at once. It takes time and you have to build their trust, help your patients feel empowered and make sure they know that this is a team effort, and you are available to answer any questions.”
Dr. Marrelli tries to provide information about glaucoma in little “bites” using relatively simple terms. “I don’t avoid the word ‘blindness,’ but I put it in perspective,” she explains. “This is especially important for those who have mild disease. I might say something like, ‘untreated glaucoma can lead to blindness, but we’ve detected yours very early. If we are able to control your eye pressure, I think you have a very good chance of keeping the vision that you have.’”
It is also important to help patients understand the link between intraocular pressure (IOP) and glaucoma, she notes. “I usually tell them that we have three ways to lower IOP: drops, laser and surgery. If surgery is not something I’m considering right away, I usually put that to the side (‘we don’t need to talk about surgery right now; we’ll talk about it later if we need to’).”
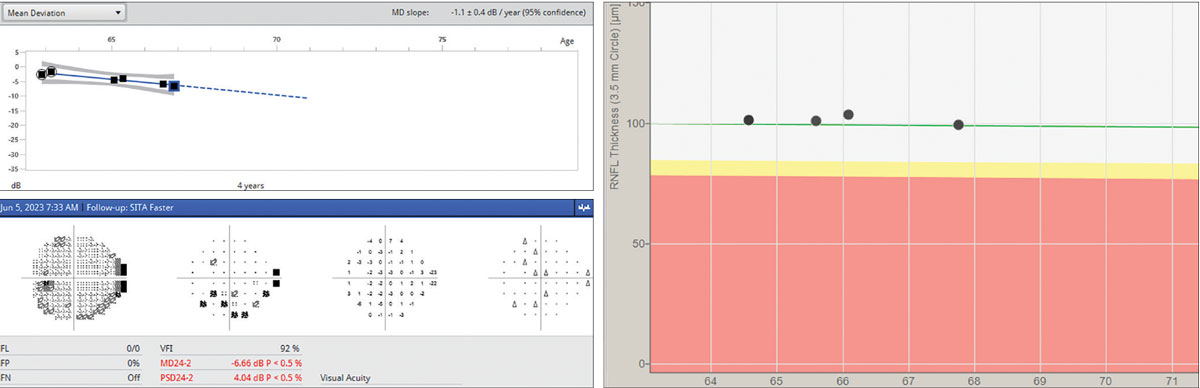 |
Fig. 1. Demonstrating to patients how their disease is progressing/remaining stable by showing them the actual resources we use to determine treatment success/failure can take some of the mystery out of the process and generate talking points that can help reinforce their knowledge of how their glaucoma is evolving. Click image to enlarge. |
Taking a straight-forward yet encouraging approach can help patients faced with a daunting diagnosis. “Glaucoma is a lifelong disease that has a significant impact on daily life,” says Marcus Gonzales, OD, clinical associate professor at the University of Houston. “As optometrists, it is important to provide both medical and emotional support. Our patients are looking to us for guidance—be reassuring. When communicating with them, acknowledge the impact of this diagnosis while also discussing their options for adapting their lives to it and transitioning to management.”
From the start, Dr. Marrelli reminds her patients that they also have a role to play in management. “I can make recommendations about the best way to lower IOP, but they have the day-to-day role of using their medication,” she says. “I talk about the importance of not only keeping up with eye drops, but also keeping up with appointments. I let them know that initially there will be quite a few visits, but often those start to spread out once things stabilize.”
When discussing a glaucoma diagnosis for the first time, Dr. Marrelli always ends by asking the patient what questions they have. However, she notes, they often feel too overwhelmed to have questions. “I tell them to keep a notebook and jot down questions as they come up and to bring the notebook with them to the next appointment so that we can discuss them,” she says.
“Finally, I try to go back and revisit these things on subsequent visits. The ‘information dump’ or telling them everything the first time can be overwhelming, so I’ll do a little at first and add/clarify at subsequent visits.”
Treatment Adherence and Costs
Compliance with treatment regimens poses a significant challenge. However, fostering open dialogue, addressing concerns and providing practical strategies can help improve adherence.
“The first step is to develop a good doctor-patient relationship,” notes Dr. Fanelli, while emphasizing the importance of creating trust with patients. “This becomes more of a psychological approach rather than a medical approach. Different people are motivated by different things. Find something you can relate to them with then use it to help gain their trust.”
Several factors can contribute to low treatment adherence, including side effects, high costs, denial or avoidance and a lack of understanding. Remembering to take medications at the correct times can also be challenging, especially for elderly patients. Education and open lines of communication can help mitigate some of these factors, notes Dr. Gonzales.
“Side effects are a common reason patients stop their medication, and they should be addressed from the start,” he says, while underscoring the value of patient education. “It is important that your patients aren’t caught off guard, and this also helps build trust—another key aspect of treatment adherence.”
Dr. Marrelli recommends using open-ended questions when asking patients about their medication use (e.g., “tell me how you use your drops” rather than “are you using your drops?”).
“Use language that normalizes missing drops. ‘No one is perfect… everyone misses a dose now and then… I need to know how you are using your medications so I can make the best decisions about the next steps in your care,’” she says.
If the patient is non-adherent, it is important to find out why. Ask them, “What do you think is standing in the way of you getting your drops in each day?” Optometrists, Dr. Marrelli notes, should try to work with their patients to find solutions, such as tying their drop use to other daily tasks (e.g., other medication use, brushing teeth, watching the evening news).
In some cases, she says, it may be warranted to look for other medications that are less expensive or don’t have as many side effects. “We have a lot of options today.”
 |
|
Fig. 2. Optic nerve head photo OS of a 59-year-old Black female with a notch noted along the inferior temporal neuroretinal rim with an associated nerve fiber layer wedge defect. Click image to enlarge. |
The asymptomatic nature of glaucoma can lead some patients to underestimate the seriousness of the disease and the necessity of treatment. ODs play a critical role in helping their patients understand the importance of treatment adherence.
“I do my best to be proactive from day one,” says Dr. Rixon. This includes thorough patient education and ongoing communication. “I have my patients look at the testing with me. This helps them understand the process and recognize that they are a critical member of the team.”
Patients with glaucoma often feel a sense of powerlessness and lack of control. A recent study identified modifiable behavioral factors that could increase patients' self-perceived ability and confidence to manage their own eye care.1 Data showed that locus of control, level of depression and self-rated functional vision were each associated with patient behaviors, attitudes and beliefs needed for health self-management and may be important determinants of adherence behaviors. Targeting change in patients’ care beliefs and behaviors may improve activation and treatment outcomes, according to the study authors.
“Our study underscores the importance of identifying modifiable behavioral attributes to improve patients’ activation levels and lead to increased involvement with their own care,” they concluded, while offering the following recommendations:1
• communicate an understanding of each patient’s perspective and factors that impact their lives by linking treatment plans to patient goals
• educate patients about their condition and the need treatment adherence and for regular follow-up exams
• identify underlying patient beliefs and behaviors needed for their appropriate involvement in their own care
The financial implications of glaucoma care, including treatment costs and frequent follow-up visits, can also pose a significant burden, particularly on those without adequate insurance coverage. Cost barriers can prevent patients from accessing or adhering to necessary treatments. Optometrists should collaborate with patients to explore cost-effective treatment options, navigate insurance complexities and connect them with financial assistance programs when needed.
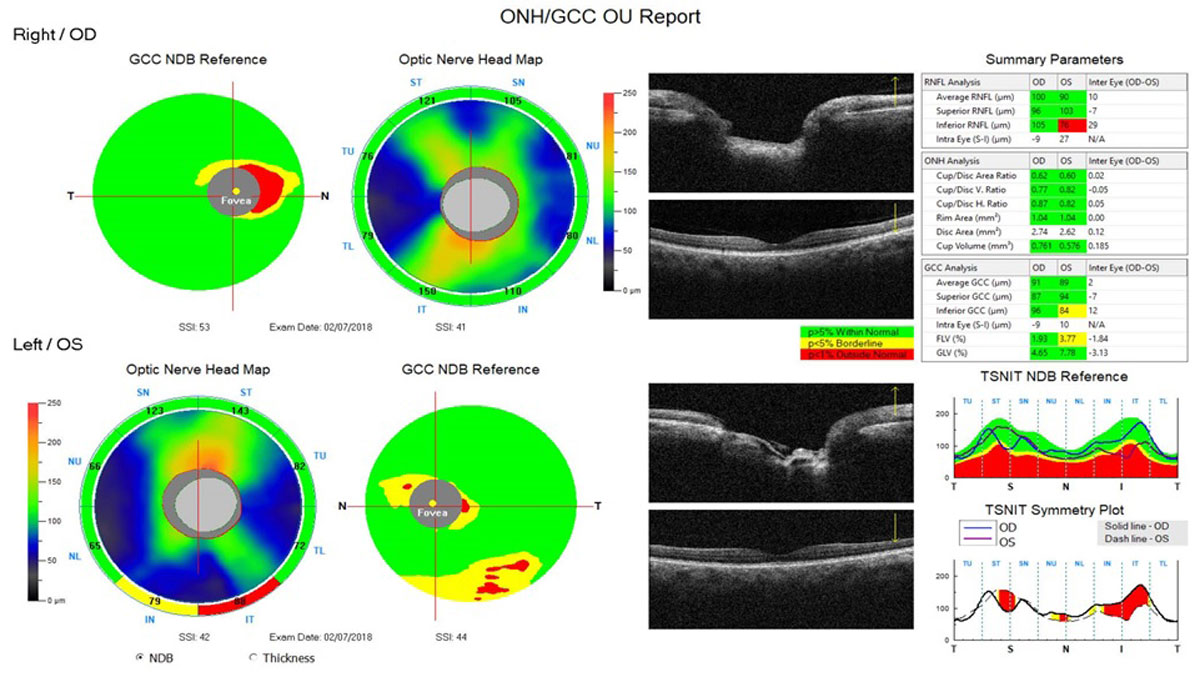 |
Fig. 3. This ONH/ganglion cell complex (GCC) analysis of the patient in Figure 2 demonstrates peripapillary nerve fiber layer and GCC defects correlating to the glaucomatous notch noted on the optic nerve. Click image to enlarge. |
Supporting Undeserved Communities
Individuals from these and/or minority communities must often contend with additional challenges, such as lack of insurance coverage, difficulty taking time off work for doctor visits, childcare issues and reliance on public transportation. These patients may also be hesitant to seek care due to a distrust of the medical establishment.
Research has shown that the prevalence of glaucoma in the United States is higher in Black and Hispanic patients compared to their white counterparts; however, these groups are less likely to receive preventive and ongoing care.
A recent analysis highlighted the existence of significant disparities in eye care among Black, Hispanic and Native American patients. Data demonstrated that glaucoma is undertreated in these racial minority groups, with Black and Hispanic individuals less likely to receive eye exams and imaging tests. These groups also have higher counts of emergency care and laser procedures.2
“Our results also demonstrate a significant disparity in care for Native American patients who were more likely to have poor vision and had substantially lower utilization of almost all eyecare services, indicating that glaucoma may be undertreated in this population,” the study authors wrote.2
There are number of factors that could account for these disparities. For instance, Black patients have been found to have reduced medication adherence, which may contribute to glaucoma progression and poor vision outcomes.
“Lower adherence to medication regimens and follow-up appointments may be due, in part, to lower trust in the healthcare system among racial and ethnic minorities as mentioned previously,” the researchers noted.2
As the director of a charity eye clinic just north of downtown Dallas, Dr. Gonzales works closely with underserved communities. “In these patient populations, I have found that there can be a real distrust of doctors. They often feel neglected or treated poorly by the medical community,” he says. “This is a hurdle that must be overcome and it takes time. We have to break down those trust barriers and show that we not only care but are in invested in helping them achieve the best possible outcomes.”
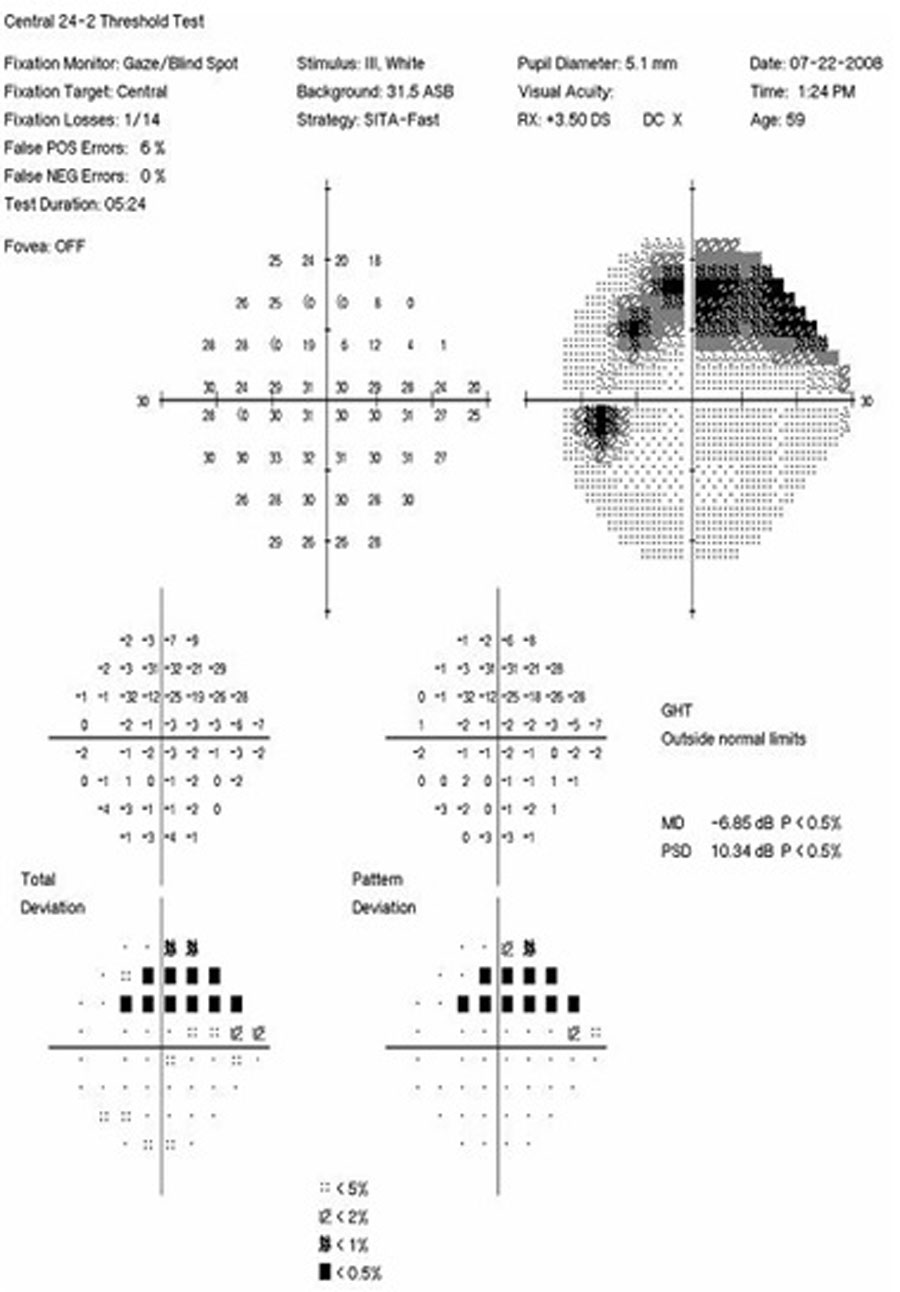 |
Fig. 4. Visual field associated with glaucomatous optic nerve seen in Figures 2 and 3. This 24-2 Humphrey visual field OS demonstrating a superior temporal arcuate defect correlating to the notch noted on the optic nerve and to the NFL/GCC defects noted on the OCT. Click image to enlarge. |
When it comes to other challenges, like transportation to appointments, Dr. Gonzales is upfront with patients about the need for various exams and testing. Initially, he notes, a glaucoma diagnosis will require frequent appointments. By giving patients a heads up, they can coordinate with families or friends if they need rides to and from appointments. “At the same time, I will make it clear that this frequency will not always be necessary,” he says. “Once we start scheduling appointments three or six months out, I direct them to community resources. For example, we have city-based transportation that can be scheduled in advance for patients who don’t have reliable access to transportation.”
Dr. Marrelli also sees a lot of patients from underserved areas who often don’t have insurance and/or find the cost of glaucoma medications and care to be challenging. “I work with companies to see if the patient might qualify for patient assistance to receive their medications for free,” she says. “If they don’t qualify, I look at generic possibilities to reduce the cost of medications as much as I can.
“Laser, while costing more initially, may ultimately be more cost-effective for some glaucoma patients,” she adds. “For patients within our larger county, I often try to refer them in to our county system, which can provide comprehensive care on a sliding scale.”
Optometrists must be aware of such disparities to ensure they can properly care for these populations and help them navigate an already challenging diagnosis.
AI's Role in Glaucoma
Discussions around artificial intelligence (AI) and its potential use continue across various professions, including optometry, is no exception. A recent study published in JAMA Ophthalmology suggests that AI was able to match or outperform human specialists in glaucoma and retinal disease management.3
The overall pairwise comparisons revealed that both trainees and specialists rated the chatbot’s accuracy and completeness more favorably than those of their specialist counterparts, with specialists noting a significant improvement in the chatbot’s accuracy.
While acknowledging that further testing is needed, Andy Huang, MD, lead author explained, “For patients, the integration of AI into mainstream ophthalmic practice could result in quicker access to expert advice, coupled with more informed decision-making to guide their treatment.”
Although Dr. Gonzales has not used AI in his own practice, a preliminary look at the tool highlighted some of its potential. “When I asked the chatbot questions regarding glaucoma, such as ‘What can you tell me about glaucoma?’ or ‘How can I best manage my glaucoma?’ I received good information,” he says. “The responses to my questions were very broad, but it offered a starting point.”
Where does he think AI might be useful? “I think this could be helpful for young doctors or those who may not have a lot of experience with this condition. It could be a resource that assists ODs in the development of a concise initial discussion about glaucoma,” Dr. Gonzales suggests, while emphasizing that the nuances of individual patients must be taken into account.
Dr. Rixon says that he believes that AI and chatbots could be helpful additions to patient education with the caveat that there is still a need for oversight. “We are in the fourth industrial revolution, and that’s AI,” he says. “There's a lot of concern surrounding this technology, but I think that we have to be willing to embrace the positives while still recognizing and prioritizing human skill.”
Takeaways
The various challenges associated with managing patients suffering from glaucoma, including psychological impacts, financial burdens and treatment adherence struggles go hand-in-hand and all have an effect on the patient experience. Through a holistic approach, optometrists can not only provide comprehensive clinical care, but also help their patients adapt to a life-changing diagnosis.
“Empowering your patients is an important part of glaucoma management,” says Dr. Rixon. “From the beginning, help them understand that they can take control over their disease and find ways to empower them as they adjust to their ‘new normal.’”
ODs have a responsibility to help these patients navigate a multitude of challenges on their journey to help preserve vision and maintain a good quality of life by addressing the clinical aspects of this condition and also understanding and supporting them through the emotional, practical and financial obstacles they face.
By fostering a compassionate and collaborative approach, ODs can help their patients to overcome these challenges and thrive despite the diagnosis of glaucoma.
 |
Click image to enlarge. |
|
1 1. Morse AR, Hark LA, Gorrochurn P, et al. Association of psychosocial factors with activation among patients with glaucoma. 2024;S2589-4196(24)00027-9. 2. Ciociola EC, Sekimitsu S, Smith S, et al. Racial disparities in glaucoma vision outcomes and eye care utilization: an IRIS registry analysis. Am J Ophthalmol. 2024;S0002-9394(24)00126-0. 3. Huang AS, Hirabayashi K, Barna L, et al. Assessment of a large language model’s responses to questions and cases about glaucoma and retina management. JAMA Ophthalmol. 2024;142(4):371-5. |

