Glaucoma Pearls & PitfallsIn the July 2024 issue of Review of Optometry, our 30th annual Glaucoma Report, seasoned ODs share tips on using modern tools, technology and knowledge to provide top-notch care to your patients with this chronic condition. Check out the other articles featured in this issue:
|
As the global population ages and the prevalence of glaucoma rises, the need for effective and accessible management strategies has never been more critical. Optometrists are uniquely positioned to lead the charge in the early detection and comprehensive management of this sight-threatening condition. With their specialized training, widespread accessibility and a patient-centered approach, ODs are indispensable in the fight against glaucoma.
“It is essential for optometrists to take the lead in glaucoma management,” notes Jackie Burress, OD, who practices at the Jack C. Montgomery VA Medical Center in Muskogee, OK. “We are on the frontline of eye care for the vast majority of patients. Optometrists are well-trained to provide exceptional glaucoma care, graduating from school with knowledge about anatomy, physiology, visual field interpretation and OCT analysis.”
And the role of the OD is set to get even more central to glaucoma care. “In many states, we also have the privilege of performing selective laser trabeculoplasty (SLT) procedures to allow our patients to choose the treatment option that works best for them,” Dr. Burress continues. “This is even more important now with the number of ophthalmologists declining, restricting access to care.”
Integrating glaucoma management into optometric practice, however, has its challenges, and some optometrists may be hesitant to expand their services. Below, we delve into the psychological and logistical barriers to success, while also highlighting strategies to help ODs step into a leadership role for the treatment of this growing cohort of patients.
 |
|
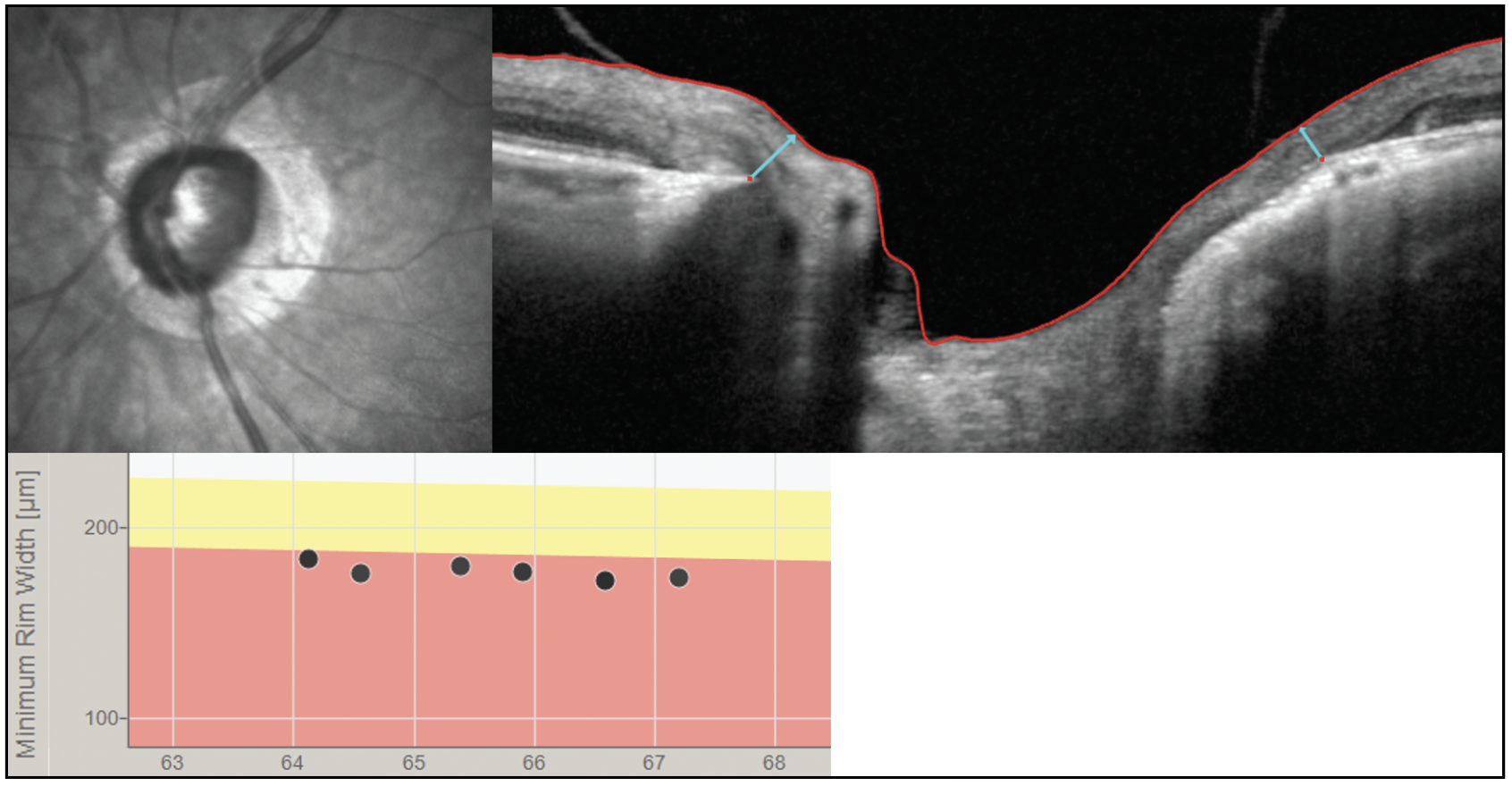
Increasingly sophisticated technologies are giving optometrists more precise information on their glaucoma patients’ disease status. For instance, the BMO-MRW image above (light blue arrows) may be a better way to track progression than the RNFL in high myopes who are suspected of having glaucoma or in those with confirmed myopic glaucoma. These new tools both improve ODs’ management of the condition and add to the slate of clinical responsibilities one must be able to perform or refer out to another provider for. Photo: Andrew Rixon, OD.Click image to enlarge. |
Key Obstacles to Overcome
Optometrists often find themselves at the crossroads of expanding their practice to include more specialized care such as glaucoma management. This transition is not without its hurdles, and there are a number of reasons why ODs might opt out of providing glaucoma care.
Psychologically, the shift demands a significant change in mindset. Optometrists must not only enhance their knowledge and skills to diagnose and manage a chronic, progressive condition like glaucoma but also build the confidence to assume greater responsibility for their patients’ long-term ocular health. This can be daunting, as it requires overcoming self-doubt, managing patient expectations and staying updated on the latest advancements.
Logistically, the incorporation of glaucoma care can involve substantial adjustments in practice infrastructure. Optometrists must invest in advanced diagnostic equipment, adhere to regulatory requirements and potentially hire or train additional staff.
Understanding these barriers is vital to address the hesitations optometrists face and develop strategies that can support them in growing their practices to include glaucoma care.
Lack of confidence and fear of failure. Managing glaucoma requires specialized knowledge and skills. Optometrists may feel uncertain about their ability to accurately diagnose and treat this condition, fearing potential misdiagnosis or inadequate patient care.
“I believe that the greatest hurdle to new graduates is the lack of confidence in their diagnostic skills,” says Dr. Burress. “One of the best ways to learn more about disease management is to pursue an optometric residency after graduation.” There are many disease-based residencies available in a variety of practice styles, including those with the Department of Veterans Affairs in VA hospitals, optometry/ophthalmology combined practices and even private practice optometry clinics. “These afford optometrists interested in disease management more experience with complicated cases to improve their diagnostic skills and learn more about the management of these patients. If a residency is not right for that individual, though, there are numerous other resources available in the form of continuing education and hands on workshops to further strengthen one’s skills.”
Adding glaucoma care into clinical practice can be overwhelming, even for the most seasoned optometrists, adds Michael Chaglasian, OD, associate professor at the Illinois College of Optometry and chief of staff of the Illinois Eye Institute. Dr. Chaglasian is also the current president of the Optometric Glaucoma Society (OGS). No matter the level of experience, he recommends that optometrists join or form their own discussion groups. “This provides a space for optometrists to talk about cases and ask detailed questions,” he says. “What does this mean on the OCT? What is this visual field? What’s the best eye drop? What are the treatment options?”
While continuing education is important, discussion groups allow ODs the opportunity to get more individualized support and advice on specific patient cases. Dr. Chaglasian notes that the OGS developed work discussion groups for just this reason. “The nuances of individual patients can be challenging to navigate and support from your peers is an invaluable resource.”
Going hand in hand with this lack of confidence is a fear of failure. “In my experience, there seems to be a fear of failure mentality among many primary care optometrists,” says Eric Schmidt, OD, founder of Bladen Eye Center in Elizabethtown, NC. “What happens if the patient doesn’t respond to the therapy that I prescribe? What if their disease gets worse?” Such lingering worries may discourage some ODs from taking a more active role. Dr. Schmidt advises taking it in stride, as this is inevitable in many cases.
“A patient may progress on your watch, but that doesn’t equate to failure. It is a part of the disease process and we must be prepared to take the necessary next steps, whether that be additional medication or surgical intervention,” he advises. “Glaucoma is not a disease we can cure; however, it can be managed successfully. The medications at our disposal today are very good, and if we do our job—diagnose, stage and treat to the target pressure—we should be able to control the vast majority of glaucoma patients.”
Contending with a chronic condition. Unlike acute eye conditions that may resolve quickly, glaucoma demands a long-term commitment, meticulous monitoring and adaptation to evolving patient needs and treatment protocols. This not only takes a toll on patients but also on eyecare providers committed to providing exceptional patient care and outcomes.
“The chronicity of glaucoma management can most definitely cause stress to providers, especially in the event of patients trending negatively with an impact in their vision and quality of life; most notably when it affects a person’s later years,” says Brian Fisher, OD, supervisor at The Villages VA Outpatient Clinic in The Villages, Florida. “We are fortunate at our practice to have the vision impairment service team, which provides social work support to our patients, and a well-equipped and trained blind rehabilitation program. In the event of poor visual outcomes, our patients can attend an inpatient blind rehabilitation center to help improve their activities of daily living,” he notes. “Having these lines of support provides hope and reassurance not just for the patient but for the provider, too.”
While Dr. Burress acknowledges that it can be emotionally exhausting when you have a compliant patient with great intraocular pressures (IOPs) that still continues to progress, she tries to find the positive and talk to the patients about how to maximize the vision they do have.
“Thankfully, I do have some wonderful ophthalmologists who specialize in glaucoma care for me to refer those patients to,” she says, while also noting that working with a low vision referral center is another valuable resource.
“It helps get your patients the tools they need to still function and be independent despite their vision loss,” Dr. Burress explains. “Also, always share these challenging cases with your trusted colleagues. A fresh pair of eyes may help you think of a different management strategy or at least emphasize the fact that you have done all you can do for a patient.”
Successful management of a chronic condition is a team effort that includes ODs and their staff as well as patients and families. “Treating ocular disease does require empathy and compassion for your patients,” says Dr. Burress. “It is important to let the patients know that they are important to you, and you want them to see clearly for as long as possible. Let them know you are in this with them.”
 |
|
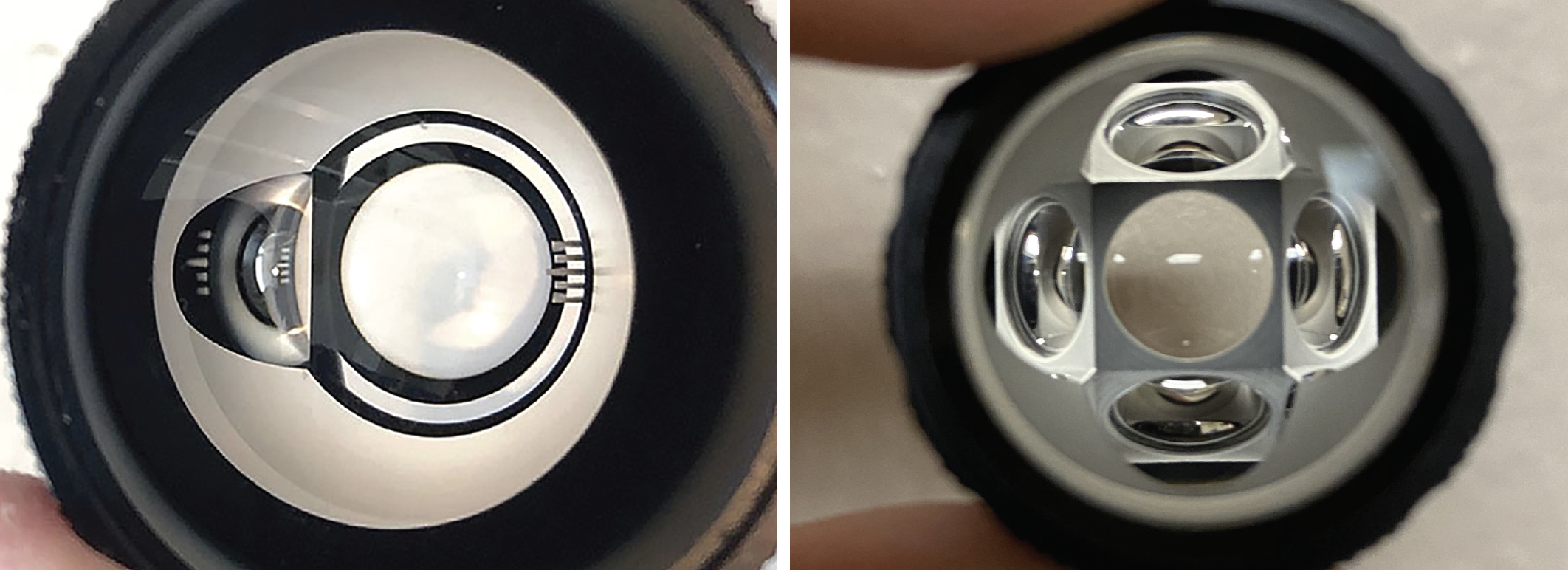
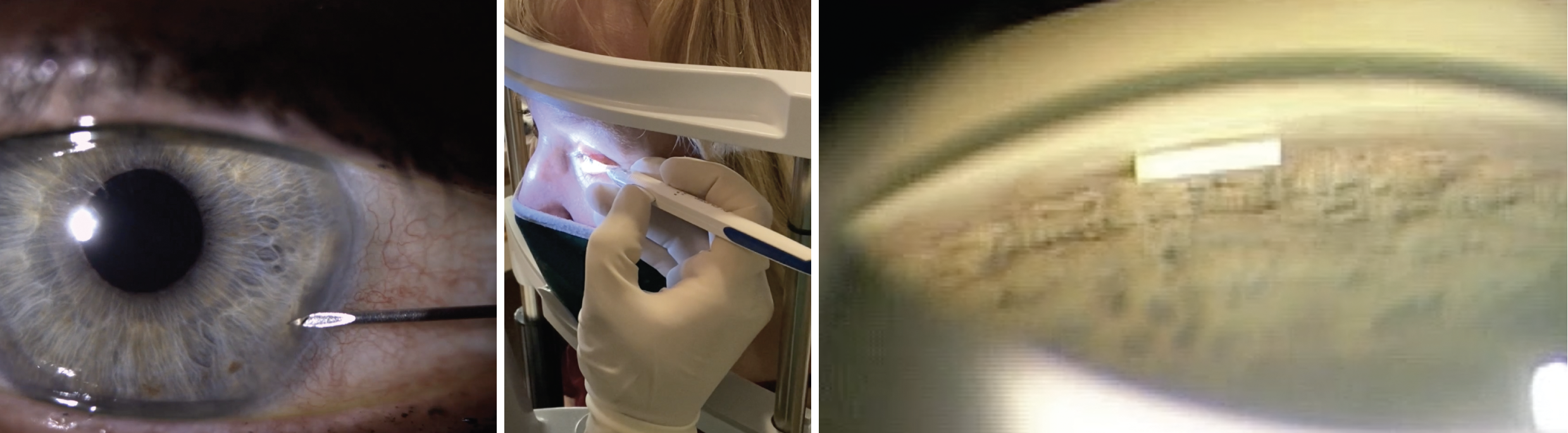
At left is a single-mirror Latina gonio lens with indexing bar, suitable for performing SLT. Other clinicians opt for the Rapid SLT lens from Volk, shown at right (notice the four mirrors), as it helps expedite procedure time and is more comfortable for patients since it does not have to be moved around to treat 360° of the eye. Such considerations will increasingly become a part of optometric practice as states continue to pass laser laws permitting ODs to perform SLT. Photos: Chris Wroten, OD, Nate Lighthizer, OD. Click image to enlarge. |
Equipment needs. To effectively manage glaucoma, optometrists need a range of advanced diagnostic and monitoring equipment. Key pieces of equipment include OCT, gonioscopy lens, fundus camera, tonometry and pachymeter. For some ODs, especially those in smaller practices or ones that don’t see a large amount of elderly people, the cost of these devices may be prohibitive.
“Diagnostic equipment for glaucoma equipment today has more options, is less costly and generally easier to use,” says Dr. Chaglasian. “If you know how to use the equipment, it can make an individual a near expert. While this equipment is an investment, it comes with significant benefits for the success and growth of your clinical practice.”
For ODs who are not ready—or are unable—to purchase the necessary equipment, there are creative ways to start glaucoma management. For instance, mobile technology companies allow ODs to rent an OCT for a day, or they could partner with a fellow optometrist in the area who has an OCT in-house.
Lack of familiarity with use and interpretation of OCT scanning can also be an impediment. Manufacturers provide ample training on their devices to ease newcomers into adoption. Table 1 lists common reasons for poor scan acquisition that practices, and particularly techs, must learn to be adept at spotting and correcting.
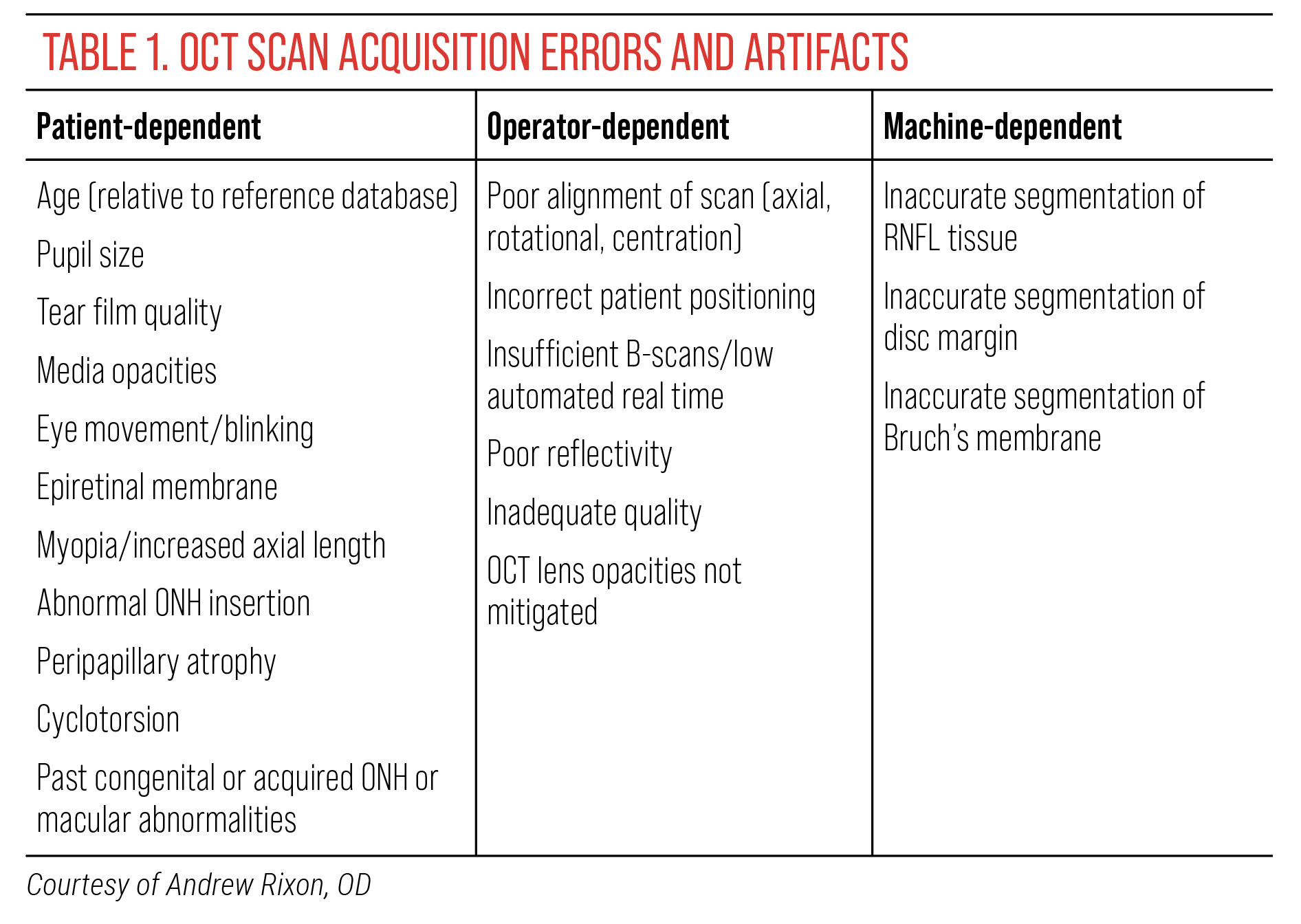 |
| Click image to enlarge. |
“I know equipment issues can also be a factor that makes an optometrist want to refer disease patients to another provider. It is important to take advantage of OD-to-OD referrals in this case,” says Dr. Burress. “Often times, another local provider is happy to perform testing you don’t have in your office, such as an OCT, which can then be sent back to the referring provider for review/interpretation.”
While lack of equipment is a hurdle that must be overcome, it does not have to be a reason to forgo glaucoma management altogether.
Medication costs and accessibility. Glaucoma meds can come with a high cost, and limited coverage for certain drugs can affect accessibility and adherence. Navigating these challenges may make some ODs question whether or not they want to dive into glaucoma management. However, this is not an insurmountable issue and ODs have the resources to meet medication-related challenges head on.
For Dr. Fisher, the main logistical issues for his glaucoma practice are the costs of topical medications and access to certain classes of newer drugs/formulations, such as approval for Vyzulta (latanoprostene bunod, 0.024%, Bausch + Lomb), Rhopressa (netarsudil ophthalmic solution 0.02%, Alcon) or Rocklatan (netarsudil and latanoprost ophthalmic solution 0.02%/0.005%, Alcon). “To gain approval, one must show therapeutic failure or have adverse effects from each of the following topical formulations: prostaglandins, beta-blockers, alpha agonists and/or carbonic anhydrase inhibitors,” he notes.
There are a number of ways to contend with these issues, but one route is to bypass meds altogether and consider SLT as a first-line treatment option, suggests Dr. Fisher. “SLT has proven itself to be an effective method for lowering IOP,” he says. “SLT is often considered in cases of inadequate IOP reduction with medications, intolerance, allergy or poor adherence to medications (e.g., due to cost, cognitive decline, insufficient dexterity or tremor) and may be recommended at various points in the treatment arc, including as the initial treatment option.” The LiGHT trial established SLT as an ideal first-line intervention, too.
For ODs who do not currently have the practice authority to perform laser procedures, a strong relationship with an ophthalmologist in their community will be critical, “especially those who integrate glaucoma care into their clinical practice,” says Dr. Chaglasian.
 |
|
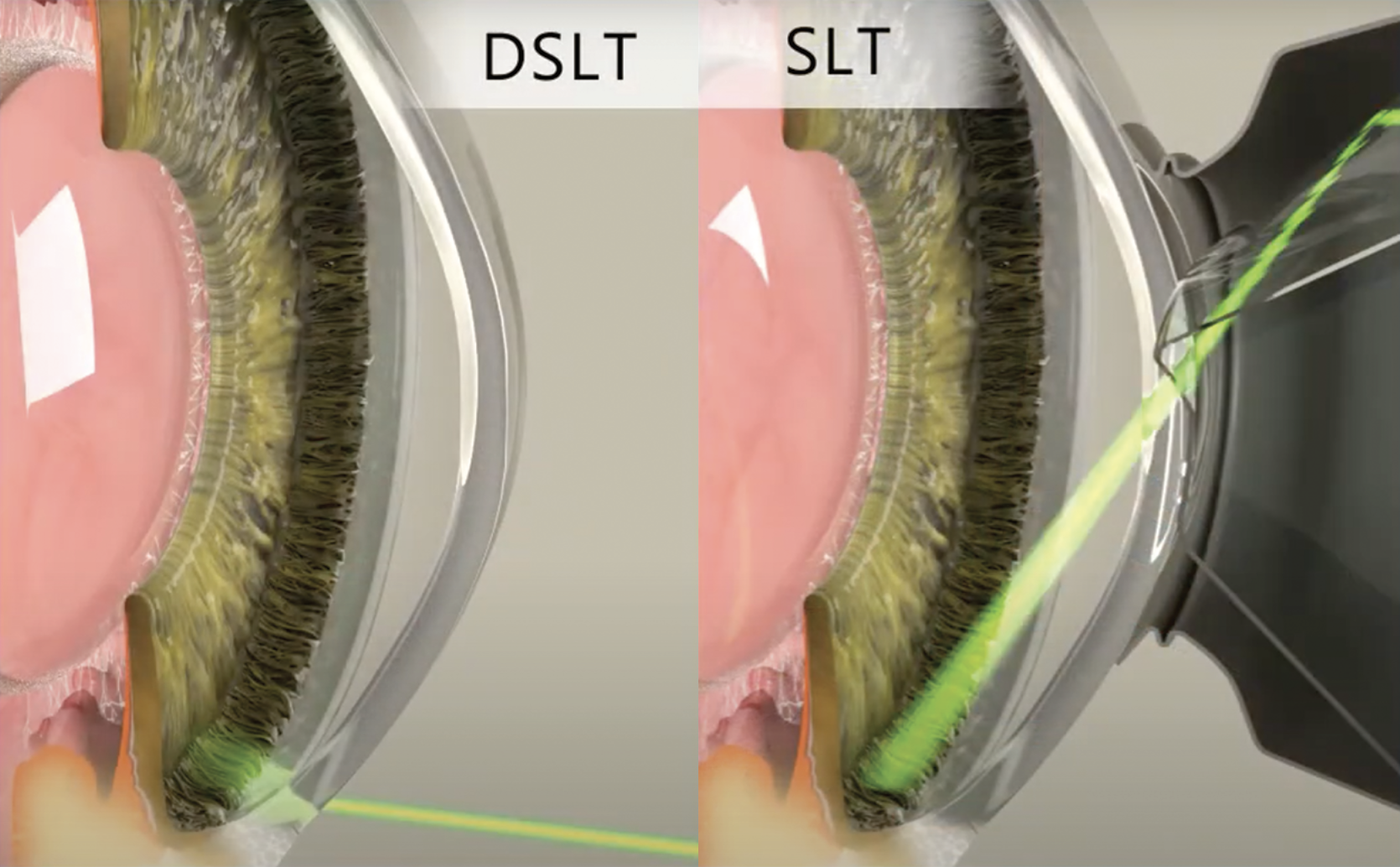
A newer technique known as direct SLT obviates the need for a gonio lens by delivering laser energy directly through the limbal area. This may allow more optometrists to transition their practices to offering SLT, as the learning curve may be lower than in traditional SLT. Photo: Belkin Vision. Click image to enlarge. |
A new laser procedure called direct SLT (Belkin Vision) does not require a gonio lens, lowering the learning curve. Some even speculate that a laser law may not be required for an OD to perform this procedure; obviously, check with your state authorities before diving in.
Insurance and reimbursement. Navigating the complexities of medical insurance, billing and coding is essential for effective glaucoma management in optometry. By staying informed about insurance coverage, using accurate codes and maintaining thorough documentation, optometrists can streamline and improve reimbursement.
ODs who have limited experience with medical plans might be hesitant to move forward with glaucoma management, but Dr. Schmidt encourages his fellow optometrists not to let concerns around insurance and reimbursement hold them back from practicing to their full potential.
“It is really incumbent upon our profession to get credentialed with Medicare, Blue Cross, UnitedHealthcare and the rest,” he notes. “If you are not credentialed, then you cannot provide this medical eyecare that your patients need and our asking for, and this is a disservice not just for your patients but for your practice as well.” Getting your practice onto medical insurance plans benefits many more patients than just those with glaucoma and should be a priority regardless, he says.
Legal concerns and liability. Dr. Schmidt is often asked, “If I start treating glaucoma, does that increase my liability?” And while the answer is yes, he urges ODs not to let that stop them from incorporating management of this condition into their clinic practice. “If you maintain quality care and manage your patients properly, the likelihood of an issue arising is low,” he notes. “Additionally, your professional liability insurance should already cover this.”
While the glaucoma management does come with potential liability issues, these risks can be mitigated with diligent practice and proactive strategies. This includes adhering to a high standard of care, maintaining thorough documentation and fostering clear patient communication. Ultimately, safeguarding patients’ vision while protecting your professional practice requires a balanced approach of clinical excellence and legal awareness.
Patient compliance. This is a critical factor in the successful management of glaucoma, but ensuring patient adherence to prescribed therapies and follow-up appointments remains a significant challenge for optometrists.
“Compliance issues are a recurrent frustration when treating glaucoma patients,” says Dr. Burress, while emphasizing the importance of trust and honesty between you and your patients. “Let them know you are in this journey with them and educate them that you can’t treat their glaucoma to the best of your ability, unless they are honest about their medication compliance.”
Many times, she notes, education about your concern for their vision and the possibility of them losing it is enough to help with compliance. Another avenue for patients who struggle with compliance is SLT, suggests Dr. Burress.
While all optometrists should be concerned about how to improve compliance, that is not a reason to avoid managing glaucoma patients, says Dr. Schmidt. “When caring for these patients, a decent portion of every visit should reiterate the importance of using their drops as well as educating patients on glaucoma and the consequences of noncompliance.
“We are here to not only provide comprehensive care but also to support patients on what can be a very overwhelming and life-changing journey,” he continues. “I would argue that, as primary eye care providers optometrists are the ones best suited to take a leadership role in the management of these patients.”
 |
|
As sustained-release drug delivery becomes more commonplace in glaucoma care, patient adherence to daily drug instillation regimens will become less of a concern. Some states even allow optometrists to perform the procedure. These images show Dr. Nate Lighthizer implanting the device. OD-to-OD referrals can help optometrists who lack experience or legal status to deliver such high-level care to their patients. Photo: Nate Lighthizer, OD. Click image to enlarge. |
Clinical Pearls for Success
Optometrists should, according to Dr. Fisher, consider the following viewpoints to optimize the treatment of glaucoma patients:
- Detect early to prevent functional vision impairment and disability.
- Maintain visual abilities for patients to live independently and stay physically active.
- Reduce psychological stress.
- Negate the medication and medical costs.
“Optometrists’ primary goal in the management of glaucoma is to ensure a lifetime of visual function to meet patients’ visual demands,” he notes. “No perfect formula exists to determine which therapeutic approach is best. By evaluating patients’ risk for visual decline, medication adherence and burden, along with the pros and cons of surgery, clinicians can individualize a therapeutic plan to address any apparent progression and preserve vision as long as possible.”
Dr. Burress emphasizes the significance of the initial diagnosis. “Spend time explaining the disease process with them and that IOP needs to be reduced to prevent progression and vision loss,” she suggests. “Let them know that medication is going to be a lifelong commitment.” Also remember to explain side effects of the medications, such as latanoprost causing conjunctival erythema and increasing the pigmentation of the iris, or potential ocular surface irritation from preserved topical drugs.
“Gonioscopy is important,” she emphasizes. “This lets you know the anatomy of the eye and correctly identify the type of glaucoma. It also lets you know if the patient is a good candidate for an SLT procedure.” You’ll need to perform this routinely as you take on more glaucoma patients (see the online version of this article for a link to a primer on gonioscopy technique and interpretation).
Additionally, she advises ODs not to forget about serial tonometry if you have a patient who is progressing, but IOPs are always great at your exam time. “People often schedule exams for the same time of day. While the normal diurnal curve shows the majority of patients have the highest IOP reading in the morning, I have seen some with higher IOPs in the afternoon. Everyone is unique and needs to be treated as such.”
Takeaways
Both patients and optometric practice as a whole benefit when ODs take a leadership role in glaucoma management, leveraging their accessibility and ongoing patient relationships to ensure timely diagnosis and effective treatment.
“It is critical for ODs to take the lead in glaucoma management. Glaucoma is a visually devastating disease with minimal symptoms until it reaches the advanced stage,” Dr. Fisher emphasizes. “Early detection is imperative, and management can help stave off progression and ensure a lifetime of preserved vision.”
By stepping up to this challenge, optometrists can significantly enhance patient outcomes, reduce the burden on the healthcare system and fulfill an essential role in the health and vision of their patients. No matter the hurdle, integrating glaucoma care into clinical practice is possible. ODs have the skills and knowledge to ensure their patients have optimal outcomes while simultaneously enhancing the field of optometry at large.
“There is such a great opportunity for optometrists to step up in even larger numbers to address the growing need of glaucoma care,” concludes Dr. Chaglasian. “Much of glaucoma care and management is relatively straightforward and not as complex or risky as people may think. It is a rewarding area of care that ODs are equipped to handle and can be easily implemented into their practices.”

