 |
A 55-year-old man reported to the office emergently with a chief complaint of blurry vision at distance in both eyes. He explained in a panic that he had woken up early that morning seeing well, then played a game on his cell phone and noticed that, after he stopped, he no longer needed his reading glasses to read.
He explained further that everything in the distance was blurry. The patient was properly medicated for hypertension and high cholesterol and denied trauma or allergies of any kind.
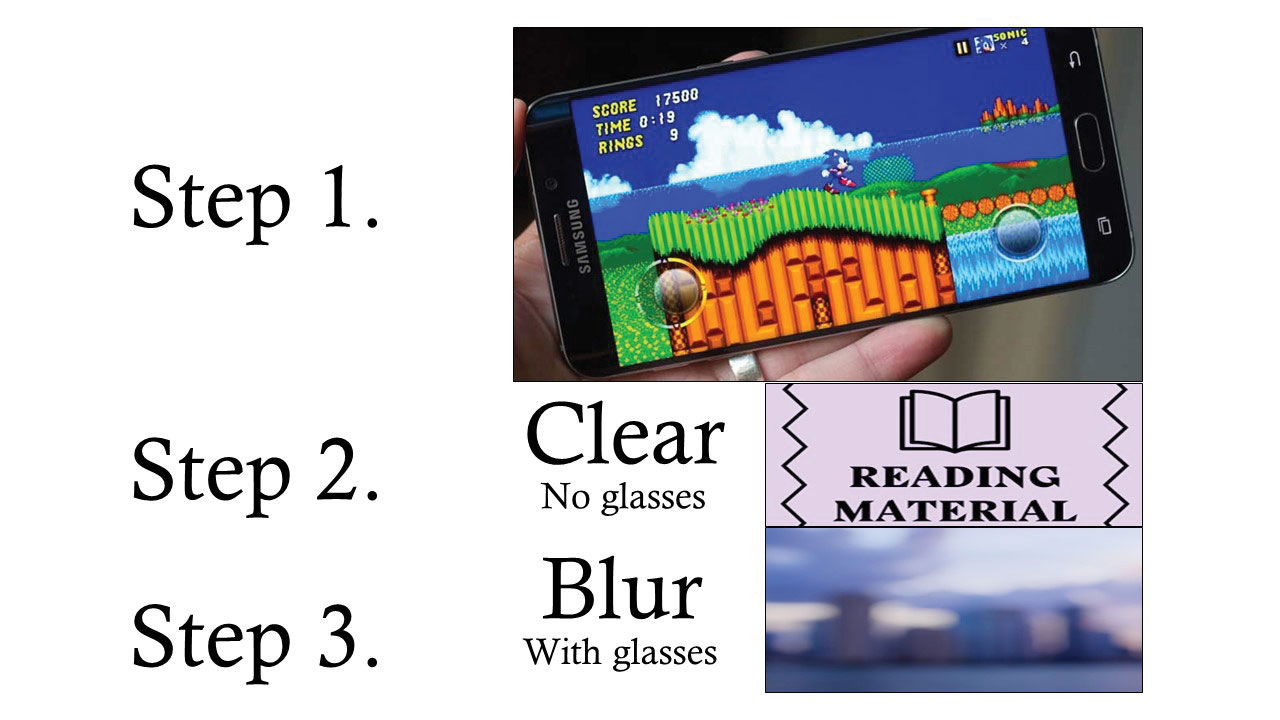 |
| The patient’s description of events: iPhone video play, followed by ability to read without reading glasses but distance vision blur. Click image to enlarge. |
Diagnostic Data
His best-corrected entering visual acuities were 20/70 at distance and 20/20 at near with a working distance of 10 inches. There was substantial improvement upon the pinhole at distance. External examination was normal for color, brightness and extraocular motilities. Confrontation fields were normal and facial Amsler grid was normal with no afferent pupillary defect.
Refraction uncovered -0.75D sphere, resulting in 20/20 vision at distance. Biomicroscopy showed normal anterior segment structures, and Goldmann applanation tonometry recorded pressures of 16mm Hg in each eye. Dilated exam uncovered normal nerves with no evidence of maculopathy or disc edema.
Additional Testing
The first important additional test is lensometry. This will permit an understanding of the previous refractive error. It can then be matched against the refraction to understand how things have changed. A detailed history should include whether vision is absent, distorted or blurry, and in which eye and when.
Workup Considerations
A very important but simple question is: has the situation improved since it was first discovered? The spectacles must be examined to rule out an issue with the optics of the lenses. Corrected and uncorrected acuities at both distance and near must be measured. Pinhole acuity may provide a clue to both refractive and corneal changes. A “punctum remotum” measurement may uncover the formation of myopia. Laser interferometry can be used to assess macular function.
Cover test can be used to detect eso posture, indicating ongoing accommodative stress. Refractive determination may include standard, auto and cycloplegic refraction. If the answer is not determined by this point, additional testing should include careful corneal examination to rule out edema or surface disease.
Topography can be used to rule out subtle changes in central and peripheral corneal curvature. Finally, if the answer is still not evident, careful dilated binocular indirect biomicroscopy of the macular region along with optical coherence tomography (OCT) of the posterior pole can rule out hard-to-detect retinal and subretinal pathologies.
Diagnosis and Pathogenesis
The diagnosis and this issue is simple accommodative spasm (AS). This condition is a condition commonly observed in children, adolescents and young adults. It can occur in older adults but is considered rare and a diagnosis of exclusion.1-4 There is no familial tendency for this binocular vision disorder.4
In AS, there is prolonged contraction of the ciliary muscle, causing pseudomyopia to varying degrees in both eyes.3 It may also manifest as an inability to allow proper adaptation of the ciliary muscle with or without measurable myopia.3 As a rule, this is a functional ailment triggered by prolonged near work and stress.1-6 The most common symptoms include blurring of distance vision, varying visual acuity as well as pains in the orbital region and the head.1-4
Other known causes of increased myopia include AS produced by ciliary body inflammation via ocular diseases such as iritis, uveitis and choroidal effusion (possible mechanism is supraciliary exudation causing ciliary body repositioning with relaxation of zonular fibers and increased convexity of the crystalline lens) and ciliary spasm secondary to the topical pharmaceutical bimatoprost (theorized to induce forward displacement of the iris and lens).2 Diabetes and cataract formation are known causes of the “myopic shift.” However, they typically are not associated with acute symptoms or concentrated near work and may occur monocularly.
In cases where the AS is produced by uncorrected hyperopia, the issue can be remedied by dispensing the plus correction with or without the use of cycloplegia (i.e., cyclo therapy).7 Stubborn or exaggerated cases may require the aid of the cycloplegic to ease the transition and break the cycle.7 Cases that are predominantly caused by an overactive or underactive system typically respond to visual therapy techniques such as accommodative rock and used of a Hart chart.
Occasionally, organic disorders are associated. Central lesions involving the dorsal midbrain and quadrigeminal plate have been described in the literature as producing disorders of accommodation.5 Here, the condition is often arrested following a lumbar puncture that results in the resolution of the papilledema.5 Closed head trauma is another identified source of false myopia production. The mechanism of the AS is speculated to be related to pathophysiology of intracranial swelling.5
In cases where the refraction has been altered by corneal refractive surgery, AS can manifest as intractable headache rather than blurred vision. Here, the refractive surgery was performed during an episode of AS. The vision may acceptable while the ciliary muscle remains contracted.7 This is a diagnosis of exclusion and can be uncovered with cycloplegia, which can also be used to break the cycle.7,8 Unfortunately, when the condition is resolved, the refraction may change, precipitating either the need for spectacles or an enhancement procedure.8
Case Resolution
The patient reported their symptoms had been improving since they were detected early in the morning and that this sort of thing had never happened before. Visual acuity was measured at near with the correction on and off and was 20/20, indicating a high probability that the health of the back of the eye was intact. Visual acuity at near through their corrective multifocal prescription was 20/20 but at a reduced working distance, indicating increased myopia. This was also uncovered in the dry distance refraction. There was no esophoric posture on distance or near cover test.
Following a dilated examination of the posterior poles of both eyes, we advised the patient regarding what had happened. The patient was offered two courses of action: (1) monitor the condition throughout the remainder of the day and report improvements or worsening or (2) proceed with relaxation of the ciliary body using an additional topical short-acting cycloplegic drop. The patient chose to monitor the condition throughout the day and informed us that after approximately 2.5 hours that their distance vision had returned to normal.
We concluded care by advising the patient on how to avoid the circumstances that might cause the issue again. We reminded him that as targets are increased in size (electronic magnification) or brought closer (relative distance magnification), they are easier to see, creating an atmosphere that will prolong the near activity. This can stress the struggling system and produce AS. While the issue seems logical, there is minimal reporting of this in the literature regarding patients of this age in association with handheld electronic devices.
Dr. Gurwood is a professor of clinical sciences at The Eye Institute of the Pennsylvania College of Optometry at Salus University. He is a co-chief of Primary Care Suite 3. He is attending medical staff in the department of ophthalmology at Albert Einstein Medical Center, Philadelphia. He has no financial interests to disclose.
| 1. Ijaz U, Habib A, Rathore HS. A rare presentation of cyclitis induced myopia. J Coll Physicians Surg Pak. 2018;28(3):S56-S57. 2. Padhy D1, Rao A2. Bimatoprost (0.03%)-induced accommodative spasm and pseudomyopia. BMJ Case Rep. 2015;23;2015. pii: bcr2015211820. 3. Lam DS, Cheuk W, Leung AT, Fan DS, Cheng HM, Chew SJ. Eye care when using video display terminals. Hong Kong Med J. 1999;5(3):255-257. 4. Lindberg L. Spasm of accommodation. Duodecim. 2014;130(2):168-73. 5. Kawasaki A, Borruat FX. Spasm of accommodation in a patient with increased intracranial pressure and pineal cyst. Klin Monbl Augenheilkd. 2005;222(3):241-3. 6. McMurray CJ, Burley CD, Elder MJ. Clear lens extraction for the treatment of persistent accommodative spasm after head trauma. J Cataract Refract Surg. 2004;30(12):2629-31. 7. Silbert JA, Alexander A. Cyclotherapy in the treatment of symptomatic latent hyperopia. J Am Optom Assoc. 1987;58(1):40-6. 8. Airiani S, Braunstein RE. Accommodative spasm after laser-assisted in situ keratomileusis (LASIK). Am J Ophthalmol. 2006 ;141(6):1163-4. |

