The following case is featured in the "You Make The Diagnosis" section of the June 2024 Optometric Retina Society quarterly e-newsletter, which can be found here.
 |
| Click image to enlarge. |
 |
| Click image to enlarge. |
 |
| Click image to enlarge. |
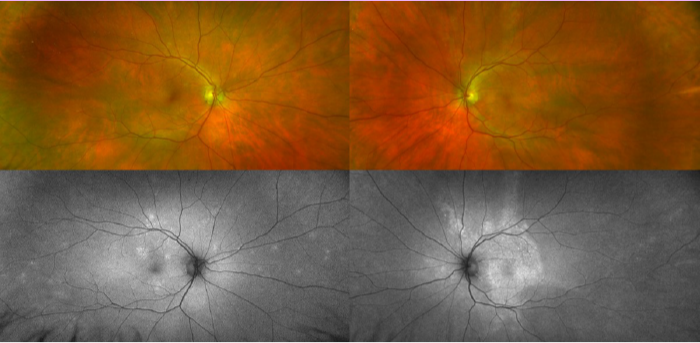
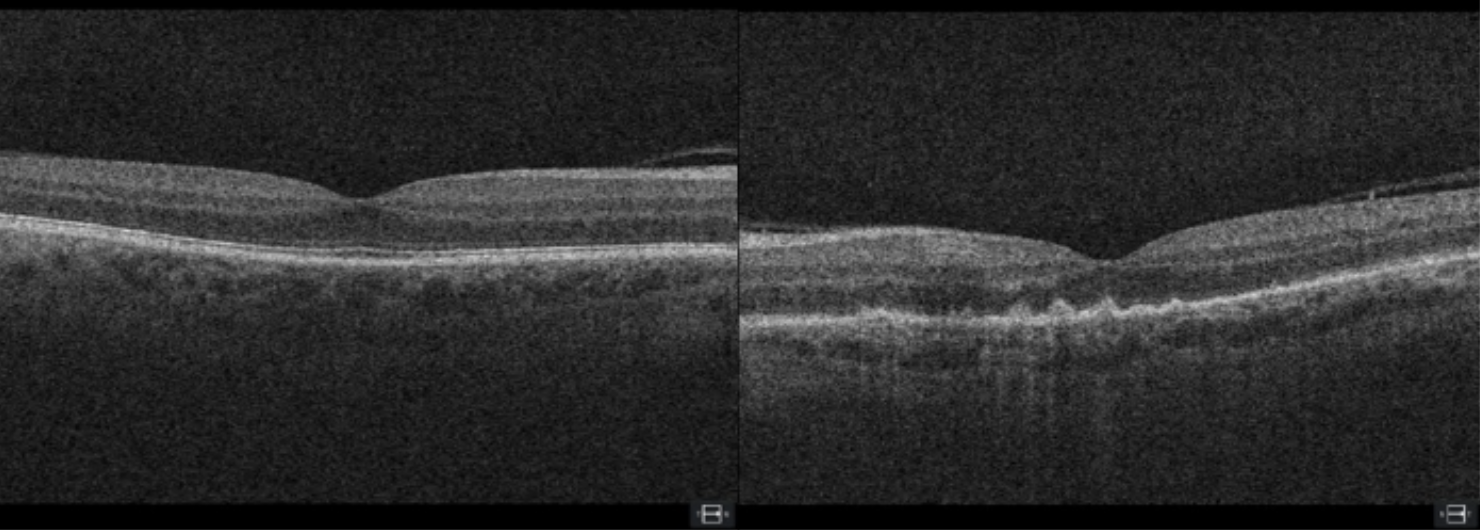
Fundus autofluorescence showed hyper-autofluorescent multifocal lesions OD and hyper-autofluorescent placoid-like lesions OS corresponding to the lesions noted on fundoscopy. OCT imaging revealed hyperreflective retinal pigment epithelium (RPE) nodules and ellipsoid zone (EZ) disruption OS >> OD. Given the presence of bilateral chorioretinitis and the maculopapular rash on his abdomen and arms, treatment was withheld until infectious titer results were available. He was instructed to stop timolol. Serology returned positive for serum T. pallidum antibodies at 44.70 Chemiluminescence Units (CU) (normal: <0.90) and T. pallidum reflexed-RPR at 1:1024 (normal: not present) with an automated message sent to the Maryland Department of Health. He was admitted same-day to the hospital ED and received IV penicillin G 4 million units continuously for 14 days. Additional STI testing was negative for HIV, hepatitis C, chlamydia, and gonorrhea. Follow up was scheduled at 6- and 12-month visits with infectious disease at hospital discharge. One-month ophthalmic follow up revealed significant functional and structural improvement in the left eye with IV penicillin treatment including BCVA 20/30-2 OS (PH 20/25+1).
Systemic and ophthalmic manifestations of syphilitic infection are caused by the spirochete bacterium Treponema pallidum. Transmission of the disease occurs primarily via sexual contact, while congenital syphilis may occur through transplacental passage from mother to fetus during pregnancy.1-3 Syphilitic infection most commonly affects males but spans patients of all decades of life. Recent statistics from the Center for Disease Control (CDC) suggest an alarming increase in prevalence for all stages of syphilis in the United States in the last one year (17.0%) and five years (78.9%) between 2018 and 2022.4 Among groups most affected by this epidemic outbreak include gay, bisexual, and other men who have sex with men (MSM). Syphilitic infection is categorized by four stages: primary, secondary, latent (early and late), and tertiary. Ocular complications of syphilitic infection can occur at any stage of the disease but present most commonly in secondary, late latent or tertiary syphilis.1,5-7 Uveitis is the most common ophthalmic presentation with posterior uveitis and panuveitis frequently encountered posterior segment findings.1,3,6,7 Acute syphilitic posterior placoid chorioretinitis (ASPPC), as diagnosed here, is a rare posterior manifestation of ocular syphilis.5 Clinical findings include a large, yellow, placoid lesion located within the posterior pole at the level of the RPE.3,7 SD-OCT is the gold standard for ASPPC diagnosis given its characteristic findings of EZ disruption and hyperreflective nodular elevations of the RPE.7Diagnosis of syphilis is made with a combination of nontreponemal and treponemal tests. For patients exhibiting signs of neurosyphilis such as meningitis, cranial nerve involvement, stroke, or altered mental status, it is recommended to conduct a CSF analysis to confirm neurosyphilis diagnosis.6 All patients diagnosed with ocular syphilis should also have HIV testing performed given the elevated risk of comorbid infection.6 The preferred treatment for syphilis at all stages of disease is parenteral penicillin G as recommended by the CDC.6 Treatment for ocular syphilis recommends aqueous crystalline IV penicillin G with 18-24 million units per day for 10-14 days.6 After completion of therapy, patients should have clinical and serological testing performed at 6- and 12-months.6 All sexual partners should also be evaluated and, in specific cases, treated presumptively.6 Healthcare providers must report all syphilis cases by stage to their local or state health department.8
1. Kiss S, Damico FM, Young LH. Ocular manifestations and treatment of syphilis. Semin Ophthalmol. Jul-Sep 2005;20(3):161-7. doi:10.1080/08820530500232092 |

