It has been three years since the release of the three-year randomized clinical trial by the National Institute of Health (NIH) known as the DREAM Study. This was the first multicenter, double-blind study comparing the efficacy of 3,000mg fish-derived oral omega-3 (EPA/DHA) daily supplementation for the treatment of moderate-to-severe dry eye disease (DED) vs. a placebo group containing refined olive oil. The findings shocked clinicians, as well as patients, after results showed no significant benefit between omega-3 and the olive oil placebo group. It is worth noting that 61% of those in the treatment arm and 54% in the control group achieved a 10-point improvement in OSDI score; however, the difference between the two groups was not statistically significant.1
The buzz surrounding these headlines made patients question the role these supplements have on their dry eye regimens. This created a divide between practitioners who had been using this supplement for years as adjunct or stand-alone therapy with great clinical results and those who were already on the fence about its therapeutic effect and role in dry eye management. This article will review the latest discourse surrounding this supplement option and what impact the DREAM Study will have on treatment today.
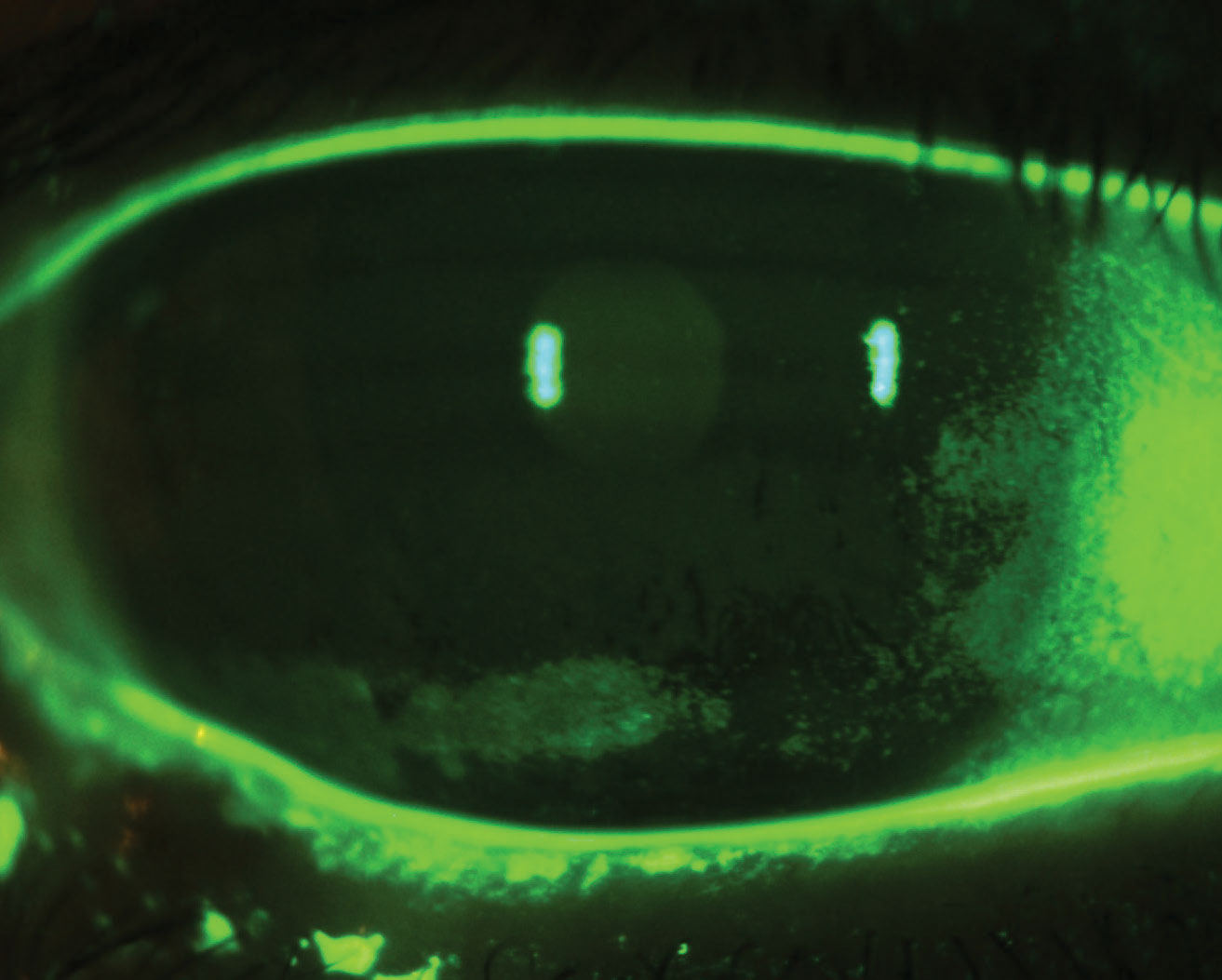
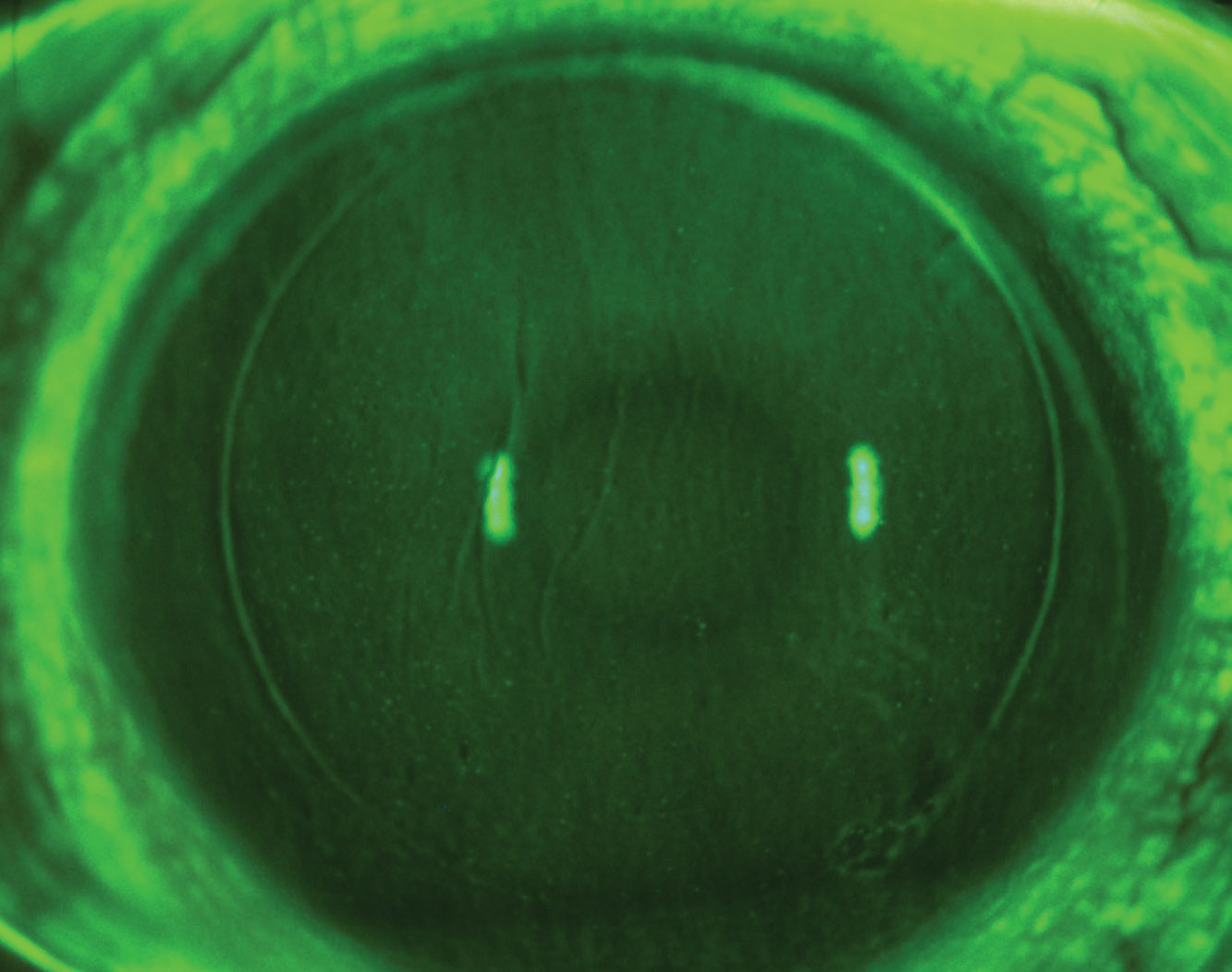 |
| LASIK-induced dry eye with diffuse SPK and micorostriae. Click image to enlarge. |
The Discussion So Far
Some criticism was aimed toward the DREAM study’s methodology based on its inclusion and/or exclusion criteria, as it allowed patients to continue their current dry eye regimen to mimic a “real-world” scenario and included those with moderate-to-severe disease.2-4 Others saw this as a positive dialogue regarding what roles overall nutrition and supplements may play in adjunct therapy.4 Shortly after, the follow-up DREAM Extension Study results were released and corroborated the study’s original findings.
The 12-month Extension Study pulled 43 patients from the original treatment arm and randomized them into two groups to compare the effects between those who continued omega-3 supplementation vs. those who discontinued the treatment. The authors reported no significant difference in the mean change between the treatment and placebo groups for OSDI score, conjunctival and corneal staining, TBUT and Schirmer’s test.5
A Cochrane review in 2019 summarized research regarding the effects of omega-3 and omega-6 polyunsaturated fatty acids (PUFA) supplementation on dry eye signs and symptoms. The review included 34 randomized controlled trials with more than 4,314 participants from 13 countries. Supplementing omega-3 as monotherapy showed little to no benefit on dry eye symptoms, relative to placebo, but improved clinical signs. However, dry eye symptoms improved when omega-3 was used as adjunct therapy along with other dry eye treatments (artificial tears, warm compresses and/or topical steroids), and when compared with omega-6 supplementation. The authors concluded that additional research is needed to improve our understanding on how to use omega-3 and omega-6 depending on the type and severity of DED.6
Research on the effect of omega-3 supplements on dry eye is ongoing in other subspecialties in eye care, such as in pre- and postoperative management, to investigate its anti-inflammatory properties. A recent prospective comparative cohort study in Korea evaluated the clinical outcomes of systemic re-esterified triglyceride (rTG) form omega-3 in patients with dry eye symptoms after cataract surgery. The researchers randomly assigned 32 of the 66 patients to the omega-3 group who received two tablets twice daily for two months of rTG form omega-3 supplement (containing a total of 1,680mg of EPA and 506mg DHA) along with artificial tears four times per day for the treatment of dry eye symptoms following uncomplicated cataract surgery. The remaining 34 patients in the control group only received artificial tears four times a day without omega-3 supplementation. At the eight-week mark, subjects in the treatment arm showed a significant improvement in Oxford corneal staining score (p-value 0.004), OSDI score (p-value 0.007), DEQ score (p-value 0.004) and MMP-9 level (p-value 0.027) compared with the control group.
Interestingly there was no significant improvement in both Schirmer’s score and TBUT given the short eight-week course; however, the authors did observe a positive trend in both parameters stating a longer follow-up would have shown significant improvements as seen in other studies. Limitations in this prospective study include exclusion criteria, duration of eight weeks, small sample size of 66 patients and lack of a double-blind study design. Despite this, omega-3 had a positive therapeutic effect on reducing ocular surface inflammation and improvement in both signs and symptoms of post-surgical dry eye syndrome.3
Furthermore, a 2019 meta-analysis compared the efficacy of omega-3 supplementation with placebo for the treatment of DED.7 A total of seventeen clinical trials were assessed providing 3,363 patients’ outcome measures—dry eye symptoms, tear break up time (TBUT), Schirmer test and corneal fluorescein staining across several countries. Interestingly, this analysis noted a significant association between the efficacy of omega-3 and the study’s country of origin.
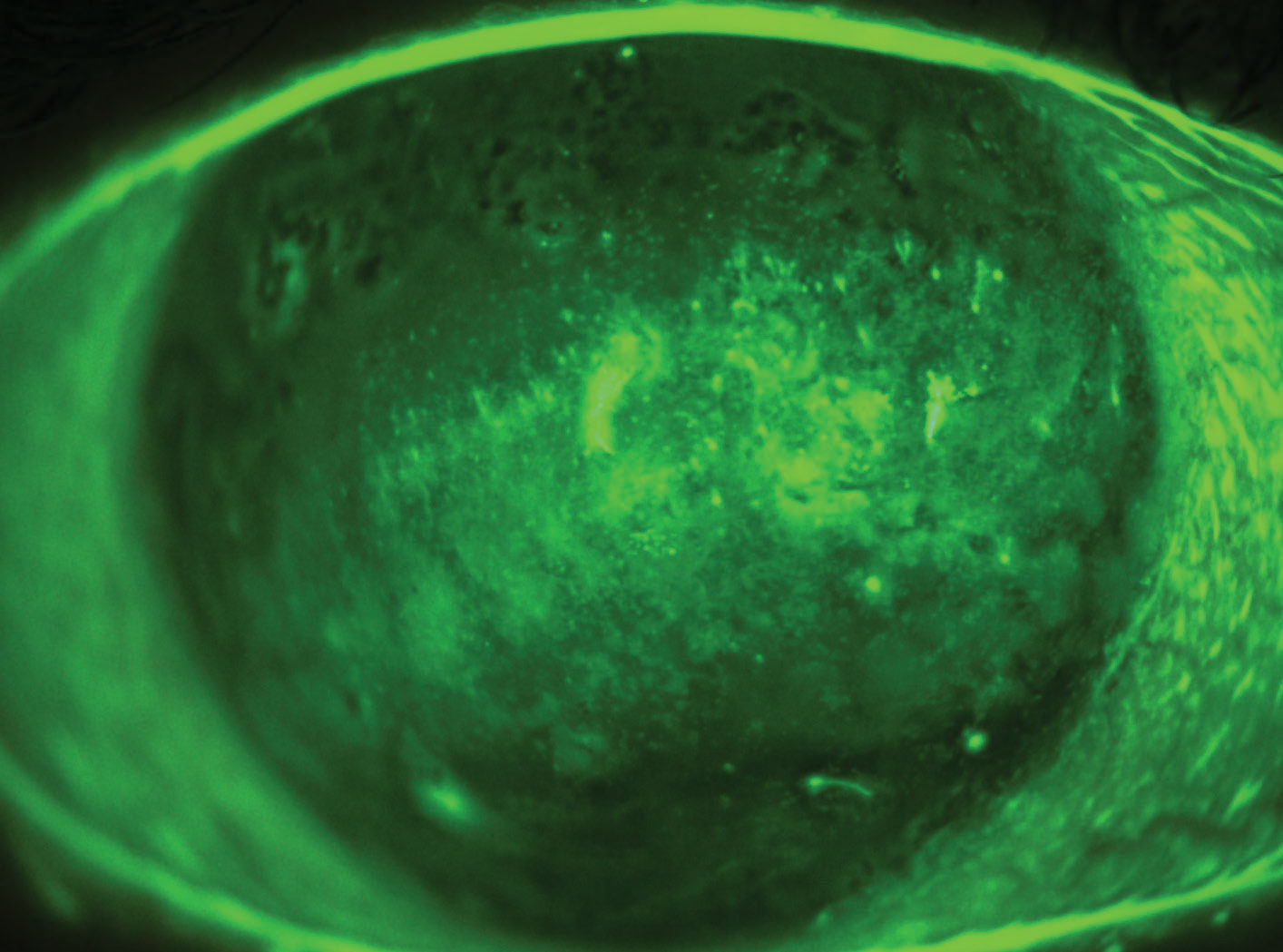 |
| Interstitial keratitis with advanced dry eye following a recalcitrant case of herpes zoster ophthalmicus (HZO). Click image to enlarge. |
For example, improvements in dry eye symptoms and TBUT were significantly higher in studies performed in India compared with other countries. The authors theorize that this higher efficacy of omega-3 supplementation may be partly due to differences in diet, as Indian culture is predominantly vegetarian with lower intake of fish-derived omega-3. The use of omega-6–containing cooking oils, such as safflower and sunflower oil, is also believed to inhibit the conversion from ALA to DHA and raise omega-6/omega-3 ratios. The outcomes of this large meta-analysis provide sufficient evidence that omega-3 fatty acid supplementation significantly improves symptoms and signs and is an effective treatment for DED.7
A recent literature review looked at several clinical trials within the past two decades regarding the efficacy of omega-3 PUFAs on DED. Trials included in this review consisted of randomized clinical trials, prospective comparative studies, and non-comparative interventional studies with levels of evidence ranging from I to III. Study sample size ranged from 12 to 905, study duration from one to 12 months, and daily dosages from 360mg to 2,000mg of EPA and 240mg to 1,050mg of DHA. This review showed that omega-3 supplementation may be an effective treatment strategy for improving both objective and subjective outcomes in DED and meibomian gland dysfunction (MGD), tear film stability and dry eye symptoms. The authors note that no formal consensus on omega-3 treatment guidelines has been established due to considerable clinical trial heterogeneity including omega-3 dosage, duration, composition, and the use of conventional objective and subjective testing that offers limited reproducibility.8
Maintaining healthy neuromodulation of the corneal nerve plexus is important in DED, especially in neurotrophic corneal disease.4 The acknowledgement of neurosensory abnormalities as an etiologic factor in dry eye was added to the definition and classification of DED in the TFOS DEWS II report.9 A prospective, comparative pilot study in 2017 investigated the effects of oral omega-3 supplementation on central corneal sub-basal nerve plexus in DED. Study participants received either omega-3 (1,000mg EPA plus 500mg DHA) or placebo (olive oil 1,500mg) daily for 90 days, and mean change in sub-basal plexus was quantified using in vivo confocal microscopy. Those in the omega-3 group saw a reduction in OSDI score and tear osmolarity, as well as increase in corneal nerve branch density and length compared with placebo suggesting neuroprotective effects.10
A 2018 cross-sectional study evaluating the relationship between omega-3 and omega-6 in postmenopausal women with DED and MGD found that dietary consumption of both fatty acids was not associated with DED; however, high omega-3 and moderate omega-6 consumptions were found to be protective against MGD. Saturated fatty acids have a higher melting point, and it is theorized that unsaturated fatty acids, such as omega-3, may have an effect on meibomian lipid composition by lowering the melting point; therefore, improving its fluidity and secretion.11
Despite these significant findings, those specializing in ocular surface and dry eye have not changed their prescribing patterns based on their own clinical experience. In fact, this has shifted the conversation for some eye care providers to learn more of the effects nutraceuticals can have in managing dry eye, especially when more patients are now looking for alternative therapies instead of prescription medications.
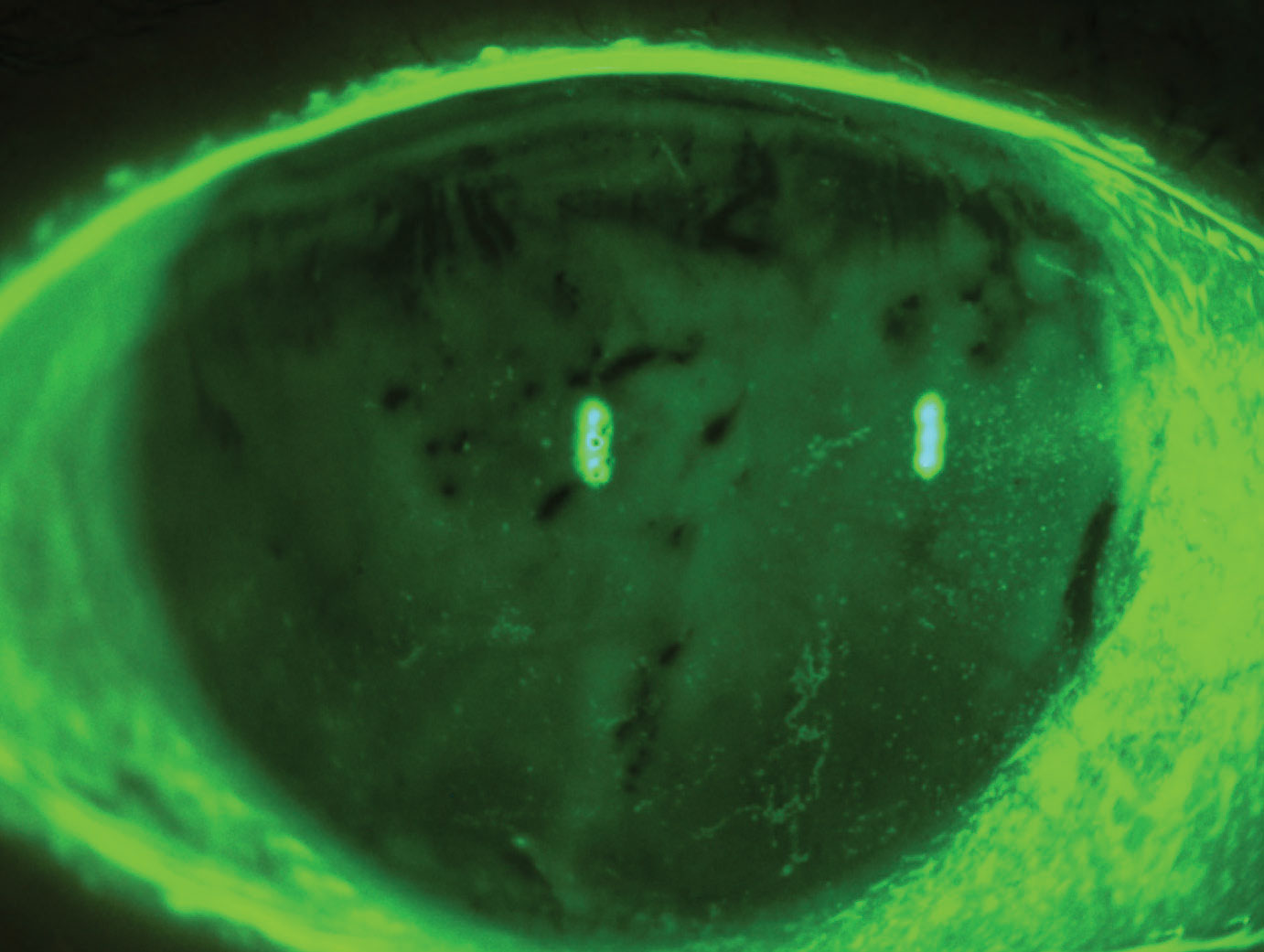 |
| Evaporative dry eye syndrome with reduced TBUT and diffuse superficial punctate keratitis. Click image to enlarge. |
A Personal Take
The power behind using a treatment that has many systemic benefits such as omega-3 has made it easy for many of us to continue prescribing it as stand-alone or adjunct therapy for our dry eye patients. Our colleagues in the cardiovascular world prescribe it as monotherapy or in combination with statins to significantly reduce triglyceride levels and risk of heart attack and stroke in diabetics and hypercholesterolemic patients. When taken at therapeutic levels, EPA has been found to reduce markers of vascular inflammation, endothelial dysfunction, improve HDL functionality and slow the development of atherosclerotic disease.12
We now know that the source, form and dosage influence omega-3’s bioavailability and effect. The re-esterification process involves the removal of the artificially induced alcohol in the chemically modified ethyl ester form to create a more natural triglyceride form of omega-3 that is better tolerated, has lower gastrointestinal side effects, and achieves superior bioavailability.3,13
Patients need specific guidance and instructions when selecting any nutraceutical including omega-3 supplements. They can easily become overwhelmed with the plethora of products available, specifically by marketing and labeling. It is recommended to stay with reputable brands who offer third party testing for purity and consistency. Storing fish oils away from heat and light prevents further breakdown of omega-3 and refrigeration for liquid forms is also beneficial. I have found better patient compliance and clinical improvement in symptoms and signs of dry eye when staying within therapeutic dosages between 1,000mg to 3,000mg EPA/DHA per day.
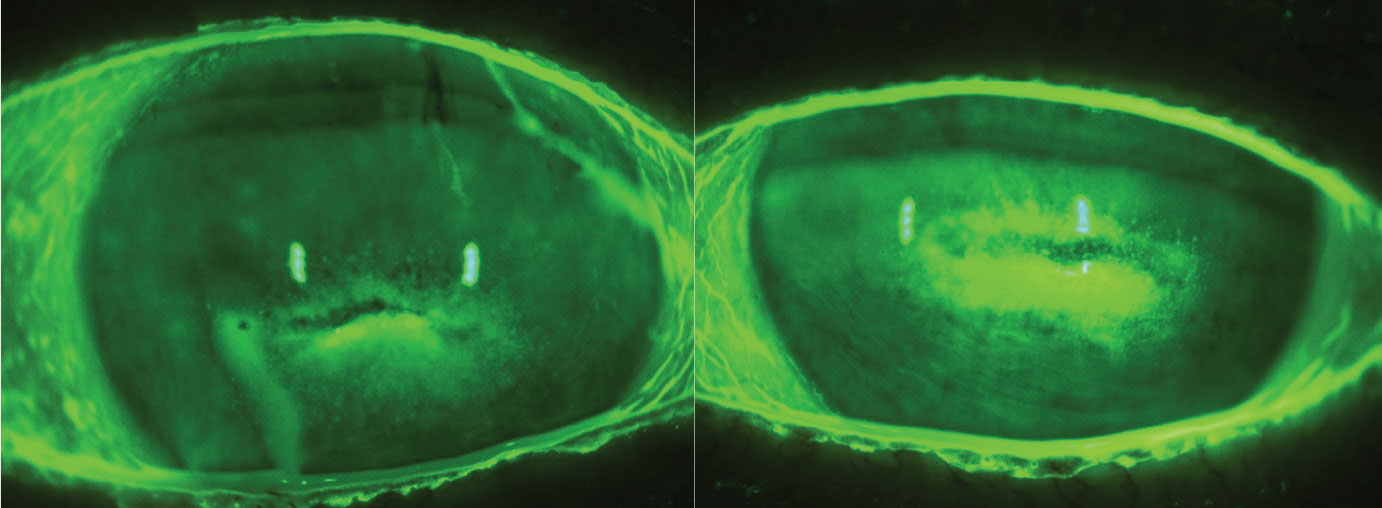 |
| Stage 2 neurotrophic keratitis. Click image to enlarge. |
Prior to prescribing an omega-3 regimen to my patients, I ensure that there are no absolute contraindications as well as minimal medication interactions, and consider any dietary restrictions. A 2017 systematic review found that fish oil reduced platelet aggregation in healthy patients; however, this did not increase pre- or post-surgical bleeding risk and therefore discontinuation prior to surgery is not needed.14 Caution should still be taken with doses above 3,000mg of EPA/DHA, especially with the elderly who are on blood thinners (warfarin, heparin, apixaban) or those with hemophilia, due to its blood-thinning effects.6 Substituting cod or other fish liver oils instead of omega-3 supplements is not ideal as these liver oils contain high levels of fat-soluble vitamins A and D that may lead to toxicity.
Be sure to consult with the patient’s primary care physician and check blood pressure on patients taking hypertension medication who are planning to start a high-dose omega-3 regimen as it may have a hypotensive effect. It is important to note that consuming fish or fish oil may have a chemo-resistant effect and should be avoided on the days surrounding chemotherapy treatment.15
There are patients who may show improvement in clinical signs prior to symptomatic relief, and vice versa, so keep this in mind before you consider it a failed treatment. As a general practice, I normally explain to patients that it may take anywhere from three to six months to allow for maximum levels of omega-3 in the blood stream; similar to checking HbA1c. It is good clinical practice to obtain baseline omega-3 levels prior to starting a regimen.6 This will help determine if there is a true omega-3 deficiency or an omega-3/omega-6 ratio imbalance.
Third party labs such as OmegaQuant and LipidLab offer simple to use in-office and at-home tests that provide quantitative metrics of a patient’s omega-3 index, omega-3/omega-6 ratio, arachidonic acid (AA) to EPA ratio and other inflammatory markers. These tests help tailor your treatment dosage, motivate patients for better compliance and even improve their dietary choices for overall health. For non-responders, I incorporate omega-6 gamma-linolenic acid (GLA) as monotherapy or in combination with omega-3, due to its documented effects in improving symptoms of irritation and lower ocular surface inflammation.16,17
 |
| Exposure keratopathy secondary to nocturnal lagophthalmos. Click image to enlarge. |
Takeaways
Dry eye is a multifactorial process that is influenced by systemic health, nutrition, metabolism and other exogenous factors.18 Incorporating a treatment that has a therapeutic role in dry eye and offers multiple systemic health benefits, has made omega-3 a topic of interest for many researchers and clinicians alike.
Current research shows that omega-3 is here to stay; however, we look forward to future studies that can shed light on improving our dosage and composition protocols, provide faster patient screenings to identify those who have omega-3 deficiencies and establish treatment guidelines that can be tailored to our patients.
Dr. Rojas is a cofounder of DeNovo Eye in McKinney, TX where he specializes in ocular disease, specialty contact lenses and myopia management. He is a consultant for Johnson & Johnson Vision.
1. Dry Eye Assessment and Management Study Research Group, Asbell PA, Maguire MG, et al. n-3 fatty acid supplementation for the treatment of dry eye disease. N Engl J Med. 2018;378(18):1681-90. 2. Chi SC, Tuan HI, Kang YN. Effects of polyunsaturated fatty acids on nonspecific typical dry eye disease: a systematic review and meta-analysis of randomized clinical trials. Nutrients. 2019;11(5):942. 3. Park J, Yoo YS, Shin E, et al. Effects of the re-esterified triglyceride (rTG) form of omega-3 supplements on dry eye following cataract surgery. Br J Ophthlamol. 2021;105(11):1504-9. 4. Pellegrini M, Senni C, Bernabei F, et al. The role of nutrition and nutritional supplements in ocular surface diseases. Nutrients. 2020;12(4):952. 5. Hussain M, Shtein RM, Pistilli M, et al. The Dry Eye Assessment and Management (DREAM) extension study - a randomized clinical trial of withdrawal of supplementation with omega-3 fatty acid in patients with dry eye disease. Ocul Surf. 2020;18(1):47-55. 6. Downie LE, Ng SM, Lindsley KB, Akpek EK. Omega-3 and omega-6 polyunsaturated fatty acids for dry eye disease. Cochrane Database Syst Rev. 2019;12(12):CD011016. 7. Giannaccare G, Pellegrini M, Sebastiani S, et al. Efficacy of omega-3 fatty acid supplementation for treatment of dry eye disease: a meta-analysis of randomized clinical trials. Cornea. 2019;38(5):565-73. 8. Hyon JY, Han SB. The protective effect of polyunsaturated fatty acids against dry eye disease: a literature review. Appl Sci. 2021; 11(10):4519. 9. Craig JP, Nelson JD, Azar DT, et al. TFOS DEWS II Report Executive Summary. Ocul Surf. 2017;15(4):802-12. 10. Chinnery HR, Naranjo Golborne C, Downie LE. Omega-3 supplementation is neuroprotective to corneal nerves in dry eye disease: a pilot study. Ophthalmic Physiol Opt. 2017;37(4):473-81. 11. Ziemanski JF, Wolters LR, Jones-Jordan L, et al. Relation between dietary essential fatty acid intake and dry eye disease and meibomian gland dysfunction in postmenopausal women. Am J Ophthalmol. 2018;189:29-40. 12. Preston Mason R. New insights into mechanisms of action for omega-3 fatty acids in atherothrombotic cardiovascular disease. Curr Atheroscler Rep. 2019;21(1):2. 13. Dyerberg J, Madsen P, Møller JM, Schmidt EB. Bioavailability of marine n-3 fatty acid formulations. Prostaglandins Leukot Essent Fatty Acids. 2010;83(3):137-41. 14. Begtrup KM, Krag AE, Hvas AM. No impact of fish oil supplements on bleeding risk: a systematic review. Dan Med J. 2017;64(5):A5366. 15. Daenen LG, Cirkel GA, Houthuijzen JM, et al. Increased plasma levels of chemoresistance-inducing fatty acid 16:4(n-3) after consumption of fish and fish oil. JAMA Oncol. 2015;1(3):350-8. 16. Sheppard JD Jr, Singh R, McClellan AJ, et al. Long-term supplementation with n-6 and n-3 PUFAs improves moderate-to-severe keratoconjunctivitis sicca: a randomized double-blind clinical trial. Cornea. 2013;32(10):1297-304. 17. Barabino S, Rolando M, Camicione P, et al. Systemic linoleic and gamma-linolenic acid therapy in dry eye syndrome with an inflammatory component. Cornea. 2003;22(2):97-101. 18. Al-Namaeh M. A systematic review of the effect of omega-3 supplements on meibomian gland dysfunction. Ther Adv Ophthalmol. 2020;12:2515841420952188. |

