 |
When considering the role of oral antibiotics, there are many situations in which an ocular condition would necessitate prescriptive use. Obvious examples include acute bacterial infections of the eyelid, cornea or conjunctiva. But on some occasions, oral antibiotics can be used in noninfectious ocular disease. An example of this is with the often underappreciated and multipurpose drug doxycycline.
Doxycycline
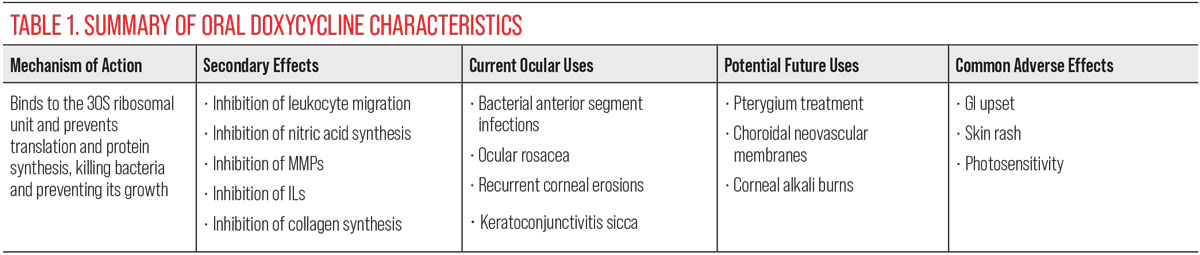
This drug is a member of the tetracycline antibiotics and is widely used in the treatment and management of bacterial infections, including ones that are ocular and systemic. Doxycycline is a metal ion chelator that is effective in killing gram-positive and -negative bacteria as well as preventing bacterial growth. To achieve this, it binds to the 30S ribosomal unit and prevents translation and protein synthesis, which kills the bacteria. It is the most commonly used drug in its class because of its high lipophilicity and ability to cross numerous cell membranes to reach a site of action. Systemically, doxycycline has long been used in the treatment of skin infections and sexually transmitted infections, and in the prophylaxis of Lyme and malaria.1,2
In addition to its antibacterial use, doxycycline is used in noninfectious ocular conditions such as acne rosacea, recurrent corneal erosions and keratoconjunctivitis sicca. It does not seem intuitive that an oral antibiotic would be effective in cases such as these, suggesting that the medication possesses additional function in controlling inflammation. In fact, doxycycline is commonly used systemically in rheumatoid arthritis. Understanding the supplementary mechanisms of doxycycline can allow for more effective use in the treatment of many other ocular conditions.2,3
Doxycycline is not only an antibacterial agent but an immunomodulator. A secondary effect of this drug is in preventing calcium-dependent microtubular assembly and production of lymphocytes, thereby inhibiting leukocyte migration. It also inhibits nitric acid synthases, which contributes to its anti-inflammatory effect; these functions are the basis of use in conditions such as rheumatoid arthritis. On the ocular surface in particular, doxycycline is shown to inhibit the synthesis and activity of matrix metalloproteinase (MMP), interleukin-1 (IL-1) synthesis, B cell function and collagen synthesis. All these processes, if left uninhibited, promote inflammation and damage to the ocular surface. This is confirmed through studies that have been able to demonstrate the effectiveness of doxycycline use in corneal burns, which are noninfectious etiologies.3,4
 |
|
Click image to enlarge. |
Ophthalmic Implications
Because of the many properties that doxycycline possesses, there is ongoing research into its treatment benefits. It has been established that in addition to VEGF, MMPs are also elevated in conditions that produce choroidal neovascular membrane (CNV), such as age-related macular degeneration (AMD). In fact, inflammation is a key aspect in the overall underlying pathophysiology of AMD. Animal studies have already demonstrated a significant prevention of CNV formation with oral doxycycline administration by inhibiting endothelial cell migration. In mice with induced CNV, there was a 50% decrease in neovascular choroidal volume with oral doxycycline use compared to placebo.3,5
Another ocular condition characterized by angiogenesis, but in the anterior segment, is pterygia. These lesions are much more common and are due to epithelial cell overgrowth and dysregulation of cells over the cornea. MMPs have been implicated in more advanced lesions, as they have been shown to be present in cells at the pterygium leading edge. Their presence is responsible for the damage that occurs to Bowman’s layer, allowing for the local infiltration of abnormal pterygium cells that are made up of fibronectin and pro-inflammatory cytokines. Fibronectin functions in the processes of cellular adhesion and migration, whereas pro-inflammatory mediators such as VEGF and IL are angiogenic. In one study, doxycycline was effective in reducing fibronectin and subsequently pterygium epithelial cell infiltration. Furthermore, neovascularization that occurs in conjunction with pterygium formation was reduced by 30% in the doxycycline-treated group compared to placebo. Many animal models showed regression in these lesions altogether. Similar results were also seen in damage and neovascular formation with corneal alkali burns.6
This data suggests that, along with antimicrobial functions, doxycycline also possesses strong anti-angiogenic properties. This could be of significant importance in cases of ocular diseases that result in neovascularization, as there is evidence that it may be effective in both anterior and posterior segment diseases. This is attributed to reports that doxycycline, even at low doses, significantly reduced blood vessel growth and migration by inhibiting levels of tumor necrosis factor-alpha, ILs and MMPs.3
 |
|
Choroidal neovascular membrane, produced in conditions like AMD, are linked with elevated MMP levels. Doxycycline can inhibit MMP synthesis on the ocular surface. Click image to enlarge. |
Unlike steroids and anti-VEGF agents that are routinely used to treat ocular inflammation and angiogenesis, doxycycline is cost-effective and readily available, easily administered and offers a better safety profile. Common adverse reactions include gastrointestinal symptoms, skin rash, headache or photosensitivity. More serious but rare effects can result in leukopenia, hemolytic anemia, dysuria, shortness of breath, intracranial hypertension and Stevens-Johnson syndrome. More often than not, however, oral doxycycline is easily tolerated.1
Doxycycline has long been established for bacterial infections both systemically and on the ocular surface, but little is appreciated in practice regarding its additional effects. More research is needed to solidify its potential use in anterior and posterior neovascular conditions.
Dr. Labib graduated from Pennsylvania College of Optometry, where she now works as an associate professor. She completed her residency in primary care/ocular disease and is a fellow of the American Academy of Optometry and a diplomate in the Comprehensive Eye Care section. She has no financial interests to disclose.
1. Patel RS, Parmar M. Doxycycline hyclate. In: StatPearls. Treasure Island (FL): StatPearls Publishing. Updated May 22, 2023. 2. Smith VA, Cook SD. Doxycycline-a role in ocular surface repair. Br J Ophthalmol. 2004;88(5):619-25. 3. Cox CA, Amaral J, Salloum R, et al. Doxycycline’s effect on ocular angiogenesis: an in vivo analysis. Ophthalmology. 2010;117(9):1782-91. 4. Dan L, Shi-long Y, Miao-li L, et al. Inhibitory effect of oral doxycycline on neovascularization in a rat corneal alkali burn model of angiogenesis. Curr Eye Res. 2008;33(8):653-60. 5. Plantner JJ, Jiang C, Smine A. Increase in interphotoreceptor matrix gelatinase A (MMP-2) associated with age-related macular degeneration. Exp Eye Res. 1998;67(6):637-45. 6. Solomon A, Grueterich M, Li DQ, et al. Overexpression of insulin-like growth factor-binding protein-2 in pterygium body fibroblasts. Invest Ophthalmol Vis Sci. 2003;44(2):573-80. |

