 |
A 75-year-old woman presented with a complaint of an abrupt blurring of vision in her right eye while working on her computer two days earlier. She reported a dryness and scratchiness in the eye as well. Her uncorrected visual acuity in her right eye was 20/80 with pinhole improvement to 20/50. She manifested no relative afferent pupillary defect, and her examination was normal, save for corneal epithelial positive and negative staining in an amoeboid pattern. There was a similar appearance in her left eye, though much less notable. The diagnosis was anterior membrane dystrophy, and her visual symptoms were adequately explained by her poor ocular surface.
On the Map
Anterior basement membrane dystrophy, also known as epithelial basement membrane dystrophy (EBMD), map-dot-fingerprint corneal dystrophy and Cogan’s microcystic dystrophy, is one of the more commonly encountered corneal abnormalities in clinical practice.1 Typically, it develops in adults between the ages of 20 and 40.2 While EBMD is a bilateral disorder, some patients may show marked asymmetry.
EBMD is often described as map-dot-fingerprint dystrophy because of its classic biomicroscopic signs—“maps” (amorphous, grayish-white geographic areas often containing oval lacunae), “dots” (focal, grayish-white, round or comma-shaped opacities) and “fingerprints” (clusters of irregular concentric lines) within the cornea.
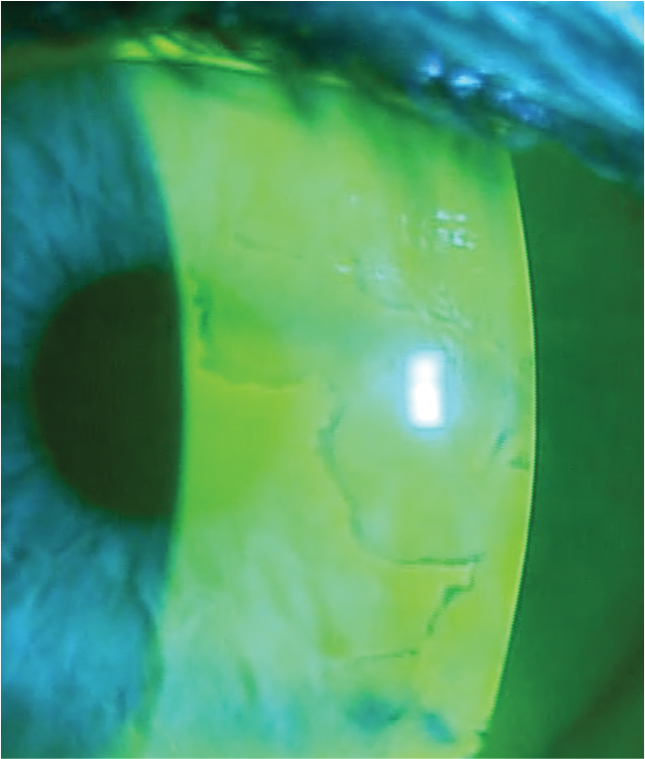
The instillation of sodium fluorescein dye helps delineate these areas, showing mostly negative staining in association with the tissue elevation created by the “maps and dots.”
Patients with EBMD are often asymptomatic, while others experience intermittent or constant blurred vision, fluctuating vision, “ghosting” (i.e., monocular diplopia) or glare. Others still may report photophobia or a foreign body sensation. Advanced cases may be predisposed toward developing a recurrent corneal erosion characterized by a periodic history of awakening with profound eye pain, blurred vision, blepharospasm or tearing.1-5
Some have classified EBMD not as a dystrophy but rather as a form of corneal degeneration.6 The corneal basement membrane adheres, via hemidesmosomal junctions, to Bowman’s layer, just anterior to the corneal stroma. Individuals with EBMD manifest a dysfunctional basement membrane, which becomes hypertrophied and misdirected.2 The basal cells in these patients manufacture aberrant projections that protrude from an abnormally thickened basement membrane into the superficial epithelium, resulting in the classic clinical findings.1,2
In addition to inducing visible changes in the cornea, the structural alterations associated with EBMD can result in impaired adherence of the overlying epithelium, prompting focal, intermittent “sloughing” of epithelial sheets.3,5,7
 |
|
The instillation of sodium fluorescein dye helps delineate maps and dots associated with EBMD by showing negative staining. Photo by Mile Brujic, OD, and David Kading, OD. Click image to enlarge. |
Treatment
EBMD does not generally require intervention. For asymptomatic patients, periodic evaluation of the corneal changes usually suffices. This may be done in a variety of ways, but anterior segment photography and/or corneal topography helps provide objective documentation.
Most patients’ symptoms related to EBMD are similar to dry eye complaints. Ocular lubricants may help alleviate intermittent visual disturbances or discomfort. More substantial disease may warrant hypertonic agents, as these help to deturgesce the epithelium and enhance the cellular adhesion between the epithelial cells and underlying stroma.3,8 An alternative to hypertonic solutions is FreshKote (Eyevance Pharmaceuticals, now a part of Santen), a non-prescription ocular lubricant that contains colloidal particles of rather large molecular weight that impart a high oncotic pressure. This agent may work in a similar capacity to hypertonic salt solutions, but with better overall lubrication and without the associated stinging upon instillation.
Contact lenses also have been used to resurface the irregular epithelium and overcome any accompanying visual disturbances.3 Both soft and rigid lenses may be used in this capacity; however, select a material with a high Dk/t to minimize corneal edema. Patients with visual symptoms may also be treated via prophylactic epithelial debridement. A study involving 74 eyes of 55 patients treated over 15 years showed that simple manual debridement helped improve visual acuity by at least one Snellen line and diminish the incidence of recurrences.9
For patients who suffer from corneal erosions, acute care involves removal of the loose epithelium, topical cycloplegia, prophylactic topical antibiotics and oral or topical nonsteroidal anti-inflammatory agents as needed for pain. Bandage contact lenses often help facilitate re-epithelialization.8,10,11
Following resolution of the erosion, take steps to protect the eye while sleeping to prevent recurrences. Ointments, both bland and hypertonic, can prevent abrupt detachment of the epithelium upon awakening.3,12,13 Likewise, sleep masks or goggles and nocturnal bandaging help prevent unconscious ocular trauma that could initiate a spontaneous erosion.
Those who do not respond to conservative management strategies may require more intensive therapy. Noninvasive treatment may involve pharmaceutical agents that mitigate the effects of matrix metalloproteinase. The combination of oral doxycycline 50mg BID and a topical steroid such as prednisolone acetate 1% or fluorometholone 0.1% TID has been effective in reducing symptoms associated with recurrent erosion.14,15
An advanced but still noninvasive option for recalcitrant cases is an amniotic membrane. This supportive therapy can greatly help regenerate corneal irregularities and provide a comfortable and visually clear surface.16,17
Another option that has been shown to ameliorate symptoms and visually rehabilitate eyes with EBMD is autologous serum tears. These tears are specially formulated from a patient’s own serum derived from blood drawn in a lab, formulated at 20% to 40% concentration and used four to eight times per day, depending upon severity. Autologous serum tears provide nutrients and growth factors not found in commercially available artificial tears and have wide applications for dry eye and other ocular surface disorders.18,19
Stromal puncture can manage recurrent corneal erosions by initiating scar formation at the level of the basement membrane, which can facilitate better adhesion between the epithelium and corneal stroma.13,20 Using a 25-gauge needle under topical anesthesia, the clinician places 0.1mm-deep perforations, breaching Bowman’s membrane at 0.25mm intervals, within the area of concern. This technique can also be achieved using the Nd:YAG laser.21
Other surgical options include superficial keratectomy using a diamond burr and excimer laser phototherapeutic keratectomy.21-24 These two techniques appear to have similar efficacy, though diamond burr treatment reportedly has less of a tendency to induce secondary corneal haze and recurrence.25,26
Takeaways
The patient presented here deferred an amniotic membrane and autologous serum tears in favor of more conservative therapy. She was prescribed non-preserved artificial tears and a hypertonic saline drop, both to be used QID in the affected eye. She returned two weeks later with some improvement in vision and appearance but found the hypertonic saline uncomfortable. The saline and tears were replaced by FreshKote to be used six times daily. She missed her follow-up appointment but relayed over the phone that she was seeing and feeling better and would return if she developed any further problems.
Dr. Sowka is an attending optometric physician at Center for Sight in Sarasota, FL, where he focuses on glaucoma management and neuro-ophthalmic disease. He is a consultant and advisory board member for Carl Zeiss Meditec and Bausch Health.
1. Labbe A, Nicola RD, Dupas B, et al. Epithelial basement membrane dystrophy: evaluation with the HRT II Rostock Cornea Module. Ophthalmology. 2006;113(8):1301-8. 2. Kobayashi A, Yokogawa H, Sugiyama K. In vivo laser confocal microscopy findings in patients with map-dot-fingerprint (epithelial basement membrane) dystrophy. Clin Ophthalmol. 2012;6:1187-90. 3. Laibson PR. Recurrent corneal erosions and epithelial basement membrane dystrophy. Eye Contact Lens. 2010;36(5):315-7. 4. Itty S, Hamilton SS, Baratz KH, et al. Outcomes of epithelial debridement for anterior basement membrane dystrophy. Am J Ophthalmol. 2007;144(2):217-21. 5. Payant JA. Eggenberger LR. Wood TO. Electron microscopic findings in corneal epithelial basement membrane degeneration. Cornea 1991;10(5):390-4. 6. Sayegh RR, Kouyoumjian PB, Vedula GG, et al. Cocaine-assisted epithelial debridement for the treatment of anterior basement membrane dystrophy. Cornea. 2013;32(6):889-92. 7. Bozkurt B, Irkec M. In vivo laser confocal microscopic findings in patients with epithelial basement membrane dystrophy. Eur J Ophthalmol. 2009;19(3):348-54. 8. Watson SL, Lee MH, Barker NH. Interventions for recurrent corneal erosions. Cochrane Database Syst Rev. 2012;9:CD001861. 9. Itty S, Hamilton SS, Baratz KH, et al. Outcomes of epithelial debridement for anterior basement membrane dystrophy. Am J Ophthalmol. 2007;144(2):217-21. 10. Fraunfelder FW, Cabezas M. Treatment of recurrent corneal erosion by extended-wear bandage contact lens. Cornea. 2011;30(2):164-6. 11. Moutray TN, Frazer DG, Jackson AJ. Recurrent erosion syndrome—the patient’s perspective. Cont Lens Anterior Eye. 2011;34(3):139-43. 12. Hykin PG, Foss AE, Pavesio C, Dart JK. The natural history and management of recurrent corneal erosion: a prospective randomised trial. Eye. 1994;8(Pt 1):35-40. 13. Ramamurthi S, Rahman MQ, Dutton GN, Ramaesh K. Pathogenesis, clinical features and management of recurrent corneal erosions. Eye (Lond). 2006;20(6):635-44. 14. Wang L, Tsang H, Coroneo M. Treatment of recurrent corneal erosion syndrome using the combination of oral doxycycline and topical corticosteroid. Clin Exp Ophthalmol. 2008;36(1):8-12. 15. Dursun D, Kim MC, Solomon A, Pflugfelder SC. Treatment of recalcitrant recurrent corneal erosions with inhibitors of matrix metalloproteinase-9, doxycycline and corticosteroids. Am J Ophthalmol. 2001;132(1):8-13. 16. Kotomin I, Valtink M, Hofmann K, et al. Sutureless fixation of amniotic membrane for therapy of ocular surface disorders. PLoS One. 2015;10(5):e0125035. 17. Miller DD, Hasan SA, Simmons NL, Stewart MW. Recurrent corneal erosion: a comprehensive review. Clin Ophthalmol. 2019;13:325-335. 18. Lee JH, Kim MJ, Ha SW, Kim HK. Autologous platelet-rich plasma eye drops in the treatment of recurrent corneal erosions. Korean J Ophthalmol. 2016;30(2):101-7. 19. Azari AA, Rapuano CJ. Autologous serum eye drops for the treatment of ocular surface disease. Eye Contact Lens. 2015 May;41(3):133-40. 20. Malecha MA. Anterior stromal puncture for recurrent corneal erosion after laser in situ keratomileusis. J Cataract Refract Surg. 2004;30(2):496-8. 21. Tsai TY, Tsai TH, Hu FR, Hou YC. Recurrent corneal erosions treated with anterior stromal puncture by neodymium: yttrium-aluminum-garnet laser. Ophthalmology. 2009;116(7):1296-300. 22. Tzelikis PF, Rapuano CJ, Hammersmith KM, et al. Diamond burr treatment of poor vision from anterior basement membrane dystrophy. Am J Ophthalmol. 2005;140(2):308-10. 23. Ryan G, Lee GA, Maccheron L. Epithelial debridement with diamond burr superficial keratectomy for the treatment of recurrent corneal erosion. Clin Experiment Ophthalmol. 2013;41(6):621-2. 24. van Westenbrugge JA. Small spot phototherapeutic keratectomy for recurrent corneal erosion. J Refract Surg. 2007;23(7):721-4. 25. Pogorelov P, Langenbucher A, Kruse F, Seitz B. Long-term results of phototherapeutic keratectomy for corneal map-dot-fingerprint dystrophy (Cogan-Guerry). Cornea. 2006;25(7):774-7. 26. Sridhar MS, Rapuano CJ, Cosar CB, et al. Phototherapeutic keratectomy versus diamond burr polishing of Bowman’s membrane in the treatment of recurrent corneal erosions associated with anterior basement membrane dystrophy. Ophthalmology 2002; 109(4):674-9. |

