What do you do when a longtime, successful rigid lens wearer now complains of discomfort and reduced vision? Or, when an otherwise healthy contact lens patient presents with neovascularization?
A corneal topography map may be your first place to start. The same topographer you used to initially fit the patient now becomes an important problem-solving tool and may even help you diagnose corneal disease. These cases show you how.
Case 1: Distortion Or Keratoconus?
A 38-year-old female who wore rigid lenses for 20-plus years complained of discomfort with her latest pair of RGPs. She also com- plained of reduced vision and an inability to change between contact lenses and glasses after about eight hours of contact lens wear. She had this pair of lenses for more than four years, and said they were uncomfortable from the start.
 |
|---|
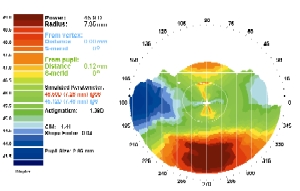
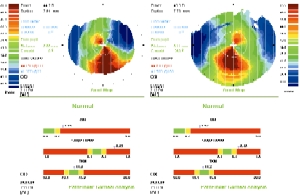
| 1. Corneal topography revealed central flattening, peripheral steepening, moderate surface irregularity and an extremely low prolate shape factor. |
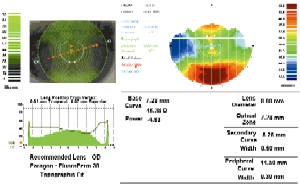 |
| 2. The patient was refit in the right eye, and the new simulated lens fit shows the initial deep tear pool centrally. |
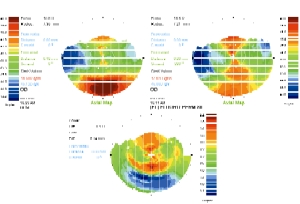 |
| 3. A week later, her corneal astigmatism increased from -1.12D to -2.62D. The shape factor also increased. |
Visual acuity with the lenses was 20/30 O.U. Over-refraction yielded no improvement.
The slit lamp exam revealed a flat-fitting fluorescein pattern with apical bearing, inferior nasal lens displacement over the limbus, moderate to excessive inferior edge lift, minimum blink-induced lens movement, poor surface wetting and moderately scratched lens surfaces. Following lens removal, the slit lamp exam showed marked central punctate staining, mid-peripheral ring imprints and negative staining over the imprinted corneal area.
Keratometry readings of 45.12/ 46.50 (6/96) O.D. and 45.75/46.50 (18/108) O.S. indicated a slight with-the-rule astigmatism. Corneal topography showed central flattening, peripheral steepening, moderate surface irregularity (CIM=1.41), and an extremely low prolate shape factor (SF=0.04) (figure 1).
Refraction after her contact lenses were removed yielded sphere powers of -3.50D for 20/50 O.D. and -4.50D for 20/40 O.S., hence the problems with interchangeability. The contact lens sphere powers were -4.50D. The base curve of the right contact lens neutralized at 7.52mm with no apparent lens warpage. This represented an approximate on-K fitting approach with a relatively large (9.6mm) overall lens diameter.
Treatment and follow-up. First, I needed to determine whether the patient had contact lens-induced corneal distortion, keratoconus, or whether RGP lens wear made her cornea more spherical. Each problem would show superior flattening and inferior steepening on topography. Based on this patient’s shape factor, I determined that she had contact lens-induced corneal distortion, even though the corneal curvature measurements were fairly steep and the topography also suggested keratoconus.
One option for this patient: I could have had her discontinue lens wear until her refraction and K readings stabilized, and then designed a contact lens based on the new values. The problem with this approach is that many eyes develop significant astigmatic increases and subsequently require more complicated bitoric lens designs to achieve an alignment fit.
Instead, I refit her lenses based on the existing corneal curvature and an alignment fluorescein pattern. If you refit immediately, you sometimes (but not always) need a bitoric. In this case, we ultimately did require a bitoric lens. I suspected that, within a year, her distortion would stabilize and her corneal astigmatism would increase; at that time, she would require a bitoric lens design.
This patient required a steeper base curve to achieve alignment and centration, so I refit the right eye in a lens that was approximately 1.50D steeper and 0.8mm smaller than the previous lens (9.6mm, and 7.29mm). This produced a lens fit that was centered and aligned (figure 2). I anticipated that the extremely low prolate shape factor in this patient would increase, and that her cornea would assume the more typical pattern of central steepness and peripheral flattening.
The patient’s corneal irregularity measurement decreased slightly from 1.41 to 1.18. Meanwhile, the shape factor increased from 0.04 to 0.20, indicating that the central cornea had steepened relative to the periphery. The apical measure of corneal toricity remained essentially unchanged. A week later, the patient’s corneal astigmatism increased from -1.12D to -2.62D (figure 3) as the lens fit and centration improved. The central cornea steepened (red), while the peripheral cornea flattened (blue).
The patient’s comfort and vision improved, and she was able to increase her wearing time. The post-wear spectacle refraction O.D. was now -3.75 -1.00 x 030 for 20/20, which would allow me to prescribe glasses that she could interchange with her contacts. This could reduce her dependence on contact lenses and prevent further contact lens-induced warpage.
As expected, over six to nine months the patient’s corneal astigmatism continued to increase, and I observed mid-peripheral corneal bearing with the fluorescein fit. She required a bitoric contact lens some nine months after the initial refitting to resolve the mid-peripheral bearing.
Discussion: Corneal topography can help you differentiate corneal warpage from true keratoconus. The key differentiating indicator is shape factor or eccentricity.
Keratoconic eyes generally have high shape factors (more than 0.6), while eyes with contact lens-induced distortion typically show low prolate (less than 0.1) to oblate (0 to -0.1) shape factors. Some additional ways to distinguish the two:
- Keratoconic eyes usually manifest a Munson’s sign, Fleischer’s ring or Vogt’s striae, while eyes with corneal distortion may only show superficial epithelial swirl staining.
- Best-corrected acuity is reduced with corneal distortion, but is better than it is in keratoconus.
- Astigmatism may be significant with corneal distortion, yet is usually less severe than with keratoconus.
Designing a contact lens for a cornea that is flatter centrally than peripherally can be challenging. Use of diagnostic lenses or a topography-generated contact lens design to achieve the appropriate base curve to corneal fitting relationship is imperative to success. Once the patient begins wearing the new lenses, it is necessary to reconfirm the K- reading and spectacle Rx without the lenses in place. These values should return to original baseline levels. A difference map that compares the initial and one-week follow-up visits will demonstrate the changes induced by the new lenses. Resolving corneal warpage is not a short-term solution. Further curvature changes can develop after 9-12 months. These may require additional refitting and possibly the use of toric lenses.
Case 2: Unexplained Neovascularization
A 34-year-old female pharmacy student wore daily wear Biomedics 38 soft contact lenses for 16-plus hours daily. She denied sleeping in her lenses and said she had worn soft lenses full time for the past 5-6 years with no apparent difficulty. Her last complete visual exam was about 2-3 years ago.
 |
|---|
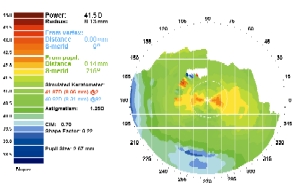
| 4. An inferior area of flattening O.S. coincided with the zone of corneal pannus and invasive vascularization. This is inconsistent with normal corneal shape. |
Distance acuity with her contact lenses was 20/20 O.U. Slit lamp examination showed that the lenses centered over the cornea with full corneal coverage and a soft lens pushup measurement of 50% movement (optimum movement). There was no central corneal staining upon lens removal.
However, there was marked inferior pannus and neovascularization under the lower lid of the left eye; this penetrated the corneal tissue approximately 1.5mm toward the pupil. Also, there was diffuse negative corneal staining overlying the corneal pannus.
Spectacle refraction yielded -2.50 -0.25 x 090 for 20/20 O.D. and -2.25 -1.00 x 075 for 20/20 O.S. Simulated K readings were 41.87/42.00 (98/008) O.D. and 40.62/41.87 (92/002) O.S.
Topography showed minimal corneal irregularity, a normal prolate corneal shape with central steepening and peripheral flattening, and low apical corneal toricity. There was an area of flattening inferiorly on the left eye. This coincided with the zone of corneal pannus and invasive vascularization, and was not consistent with the normal corneal shape (figure 4).
Treatment and follow-up. My goal was to increase the oxygen to reverse the blood flow so that only ghost vessels remained. While RGPs would accomplish this, lens awareness prevented the patient from choosing this option. I ultimately chose the PureVision lens because of its high oxygen transmissibility (Dk/t of 110 at -3.00D).
About one week later, the vessels lost their blood flow and were barely visible as ghost vessels . A month later, there was no return of blood flow into the ghost vessels. Spectacle refraction stabilized to pre-lens wear values, and acuity was 20/20 O.U. Staining was no longer visible over the pannus. Topography showed a slight steepening of the corneal curvature along with minor increases in corneal irregularity, shape factor and apical corneal toricity, but the software judged these values to represent a normal corneal topography.
Discussion: Neovascularization, especially extensive vessel proliferation with granulation tissue, is not a normal finding in an otherwise normal contact lens wearer. It represents edematous tissue and an attempt by the cornea to get more oxygen to that tissue.
The location of this patient’s vessels was especially uncommon. Neovascularization associated with chronic corneal ede- ma from hydrogel lens overwear typically presents with circumcorneal vessels that just barely penetrate the cornea (about 0.25-0.50mm). The area under the upper and lower lids often shows more extensive vascularization, presumably due to decreased oxygenation in those areas. While this phenomenon is more often seen under the upper lid, it’s extremely unusual to see it present inferiorly on the cornea.
Corneal topography can help you detect corneal edema and monitor its resolution. High-Dk silicone-hydrogel lenses or RGPs are required to provide sufficient corneal oxygen flux to eliminate hypoxia and edema, and reverse the associated neovascular response.
You must rule out other possible causes for neovascularization. These include congenital or acquired syphilis, Cogan’s syndrome, tuberculosis, Mooren’s ulcer, Terrien’s marginal dystrophy and collagen vascular diseases such as rheumatoid arthritis. Chronic corneal lipid keratopathy can be a problem with long-standing neovascularization and can cause corneal opacification and loss of vision.
Case 3: College Student Notes Vision Change
A 19-year-old male college student who wore daily wear soft toric lenses noticed a slight reduction in his distance acuity. He had worn soft lenses full time (14 to 16-plus hours daily) for the past 5-6 years without any apparent difficulty, and denied sleeping in them. His last complete visual exam was about 1-2 years ago.
 | 5. Topography shows oblique astigmatism, slight inferior asymmetry and an increased shape factor. Pathfinder analysis showed normal topographic indices. |
|---|
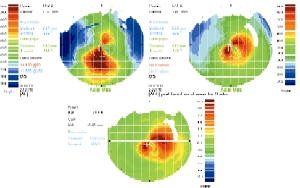 |
| 6. The difference between the original topography and the stabilized pattern shows extensive central steepening and keratoconic development. |
Distance acuity with his lenses was 20/25 O.U. Slit lamp examination showed that the lenses were centered with full corneal coverage and the soft lens pushup test measured 60% (relatively tighter than optimum movement). There was good orientation of the base apex line of the prism ballasted cylinder. There was no corneal staining upon lens removal and no apparent corneal edema.
Refraction (without lenses) yielded -6.25 -1.75 x 011 for 20/50 O.D. and -6.50 -1.25 x 152 for 20/50 O.S. New spectacle refraction yielded -8.00 -2.25 x 030 for 20/25 O.D. and -8.50 -2.75 x 160 for 20/20 O.S. Simulated K readings were 41.37/44.75 (22/112) O.D and 41.50/44.62 (160/70) O.S.
Corneal topography revealed oblique astigmatism with slight inferior asymmetry and a somewhat increased shape factor. Pathfinder analysis showed normal topographic indices (figure 5). Since there seemed to be no problem, I increased his contact lens Rx and instructed him to return in one year.
At his next annual exam, the patient reported blurred and double distance vision, dry feeling lenses and red eyes. He had worn his lenses nine hours that day and said he normally wore them 13-15 hours daily. Between visits another practitioner had provided him with a low-Dk, tight-fitting soft toric lens to wear for soccer practice.
Slit lamp examination showed that the lenses geometrically centered with full corneal coverage. The soft lens pushup test measured 75% (significantly tighter than optimum movement) and 10 temporal rotation. I also observed heavy calcium deposits on the anterior lens surface; moderately severe peripheral neovascularization; and severe epithelial bullae, which indicated extensive corneal edema.
I didn’t attempt a spectacle refraction given the distortion of his severely edematous cornea. Simulated K readings were 38.87/46.25 (132/42) O.D. and 41.25/ 46.62 (80/170) O.S.
Corneal topography showed a centrally steep, relatively symmetrical irregular astigmatism. Corneal irregularity and shape factor values were significantly elevated, presumably due to extensive corneal edema. Apical corneal toricity was slightly elevated.
Treatment and follow-up. The topography software suggested the possibility of keratoconus, although at that time I thought this was an erroneous reading due to corneal edema.
My first concern was to reduce the corneal edema. I told the patient to discontinue lens wear for about three weeks, and instill Muro 128 (5%) drops during the day and ointment at bedtime. During this time, I monitored the corneal integrity and topography. I expected a normal astigmatic pattern to return, but it never did.
The patient had indeed developed keratoconus. The difference between his original topography and the stabilized pattern shows the extensive central corneal steepening and keratoconic development (figure 6). Soft lenses were no longer an option. I designed an RGP lens, which corrected the patient’s vision to 20/20 O.U.
Discussion: Keratoconus can be very insidious in its early development, especially when it develops concomitantly with soft contact lens wear and severe corneal edema. Corneal topography is vital to demonstrate the changes that can occur to the cornea over time.
Corneal topography is an important tool, both for initial contact lens fitting and as a diagnostic aid when the patient develops problems. This can lead to a more comfortable fit for your patient and may even help you diagnose ocular disease.
Dr. Lebow is in private practice in Virginia Beach, Va. He often writes on corneal topography and has served as a consultant to Zeiss Humphrey Systems.

