Get a Head Start on Specialty Contact LensesIn the August 2024 issue of Review of Optometry—our 48th annual Contact Lens report—experts provide the tips and tools you need to start offering specialty lenses at your practice. In two more features, the authors deep-dive into soft lens optics and CL complications. Check out the other articles featured in this issue:
|
Contact lenses have been consistently popular for decades as an alternative to spectacle lens correction that offers convenience, improved aesthetics and the ability to accommodate a wide range of vision demands. Despite their benefits—and the great strides made by manufacturers in improving the safety profile of their products—improper use and poor hygiene can lead to a variety of complications. Recognizing and managing these is crucial to maintaining the ocular health of our patients. Contact lens complications can range from mild discomfort to severe ocular conditions that may threaten vision. Here, we will delve into several common complications associated with contact lens wear, describe methods for prevention and present options for treatment.
Dry Eyes
This condition takes the cake as one of the most common issues among contact lens users, though its cause can vary. To provide these patients relief and discourage dropout, the first step for clinicians is to identify the cause of the discomfort, then decide how to proceed, whether that involves recommending artificial tears or opting for a lens with more hydrating properties.
Recognition. Symptoms of contact lens-related dry eye include dryness, irritation, redness and a gritty sensation in the eyes. Patients may also report fluctuating vision and discomfort after prolonged wear, which are leading causes of contact lens dropout. Dry eye can arise from chronic lack of sufficient lubrication and moisture on the surface of the eye, which is influenced by several factors including, but not limited to, autoimmune conditions, medication use, meibomian gland dysfunction and improper lens use and hygiene.1-3 Identifying one or more of these during a patient workup should raise your suspicion for both primary dry eye and irritation during contact lens wear.
Prevention. To prevent symptoms in these patients, recommend using high-quality lenses that allow for better oxygen permeability. Encourage patients to follow proper lens hygiene and limit wear time. Regular use of lubricating eye drops can also help maintain tear film stability, if patients are willing to tolerate such a regimen. Switching to daily disposable lenses can reduce the risk of dry eye by minimizing the buildup of deposits and ensuring a fresh, clean lens surface every day.1
Management. For mild cases, over-the-counter artificial tears can provide relief—again, provided that patients are willing to commit to the expense and inconvenience. More severe cases may require prescription eye drops, such as cyclosporine or lifitegrast. To maintain contact lens wear, opt for a product with high water content and/or the least disruptive experience possible for the ocular surface.
Beyond contact lens use, it’s important to investigate other contributory factors to dry eye, such as autoimmune conditions (i.e., Sjögren’s syndrome), the use of certain medications (antihistamines, antidepressants and diuretics), meibomian gland dysfunction, compliance with the replacement schedule of lenses and the methods used to clean and store the lenses. A comprehensive approach to identifying and managing these factors can significantly improve the patient’s dry eye symptoms and overall eye health.1,3
 |
|
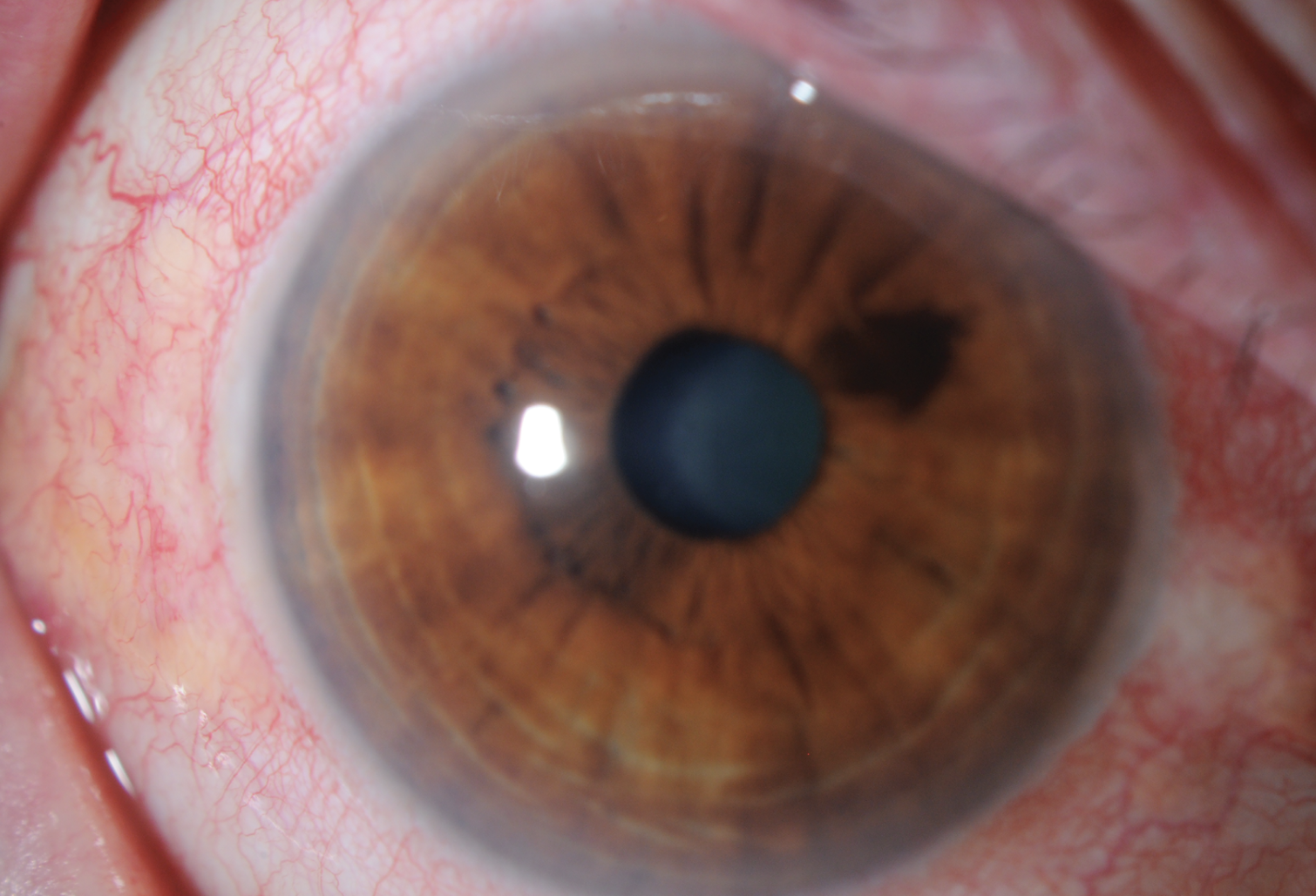
Fig. 1. The affected eye of this patient exhibits characteristic signs of viral conjunctivitis, commonly known as pink eye. The conjunctival blood vessels are visibly dilated, contributing to the overall redness. Click image to enlarge. |
Conjunctivitis
This term encompasses a spectrum of diseases and disorders that primarily affect the conjunctiva and typically arise from an underlying allergy or infection. While rare, the condition could result in serious ocular complications in severe cases, underscoring the need for immediate workup and treatment.
Recognition. Conjunctivitis can be caused by bacterial, viral (Figure 1) or allergic reactions and is often associated with improper lens hygiene, extended wear times or allergic reactions to lens materials or solutions. Symptoms include redness, swelling, itching, watery or mucous discharge and a gritty sensation in the eyes. Giant papillary conjunctivitis (GPC) is a severe form that can occur due to chronic lens wear and significant deposits, characterized by large papillae on the upper eyelid.2-4
Prevention. To prevent conjunctivitis, emphasize proper lens hygiene, including washing hands before handling lenses, using fresh disinfecting solution and avoiding contact with water while wearing lenses. Adhering to prescribed replacement schedules and using daily disposable lenses can significantly reduce the risk of contamination and allergic reactions.3,4
Management. Instruct patients to discontinue contact lens use until the condition has resolved. Treatment depends on the type of conjunctivitis. If the infection is bacterial, it can be treated with antibiotic eye drops. Viral conjunctivitis, being self-limiting, can be managed with lubricating eye drops and cold compresses. Also, advise patients about the contagious nature of viral conjunctivitis. Allergic conjunctivitis is treated with antihistamine or mast cell stabilizer eye drops.
For patients with GPC, recommend switching to daily disposable lenses, using peroxide disinfection or reducing wearing time to minimize allergen exposure and lens deposits once condition resolves. In severe cases, a short course of topical corticosteroids may be necessary. If not managed appropriately, conjunctivitis in contact lens wearers can lead to more severe conditions. Persistent or recurrent conjunctivitis should prompt a reevaluation of the patient’s contact lens hygiene practices, lens material and solution compatibility. 3,4
Corneal Neovascularization
This possible complication of contact lens wear results from the ingrowth of blood vessels from the limbal vascular plexus into the cornea. The risk of corneal opacification increases as the condition progresses, threatening the patient’s vision. However, in the early stages, patients may be asymptomatic; thus, clinicians must be well-versed in signs and symptoms to be able to intervene before a patient’s vision starts to decline.
For A Deeper DiveEach of the topics discussed in this broad overview warrants additional study. In the online version of this article, you’ll find links to the following resources from our archives: |
Recognition. Corneal neovascularization can result from a wide range of ocular pathologies and conditions including but not limited to inflammatory disorders, chemical injuries, limbal stem cell deficiency, allergies, trauma, surgery, corneal infections, autoimmune diseases, corneal graft rejection, congenital diseases, ischemia, degeneration and systemic conditions such as diabetes mellitus and vitamin A deficiency.
In contact lens users, a common cause of corneal neovascularization is a lack of oxygen, or hypoxia. Epithelial edema can also occur secondary to hypoxia. Several factors can cause chronic hypoxia from contact lens use including contact lens overwear, poor care or sensitivity to contact lens solutions. Symptoms include redness and irritation, or the patient may be asymptomatic.
Neovascularization can be superficial, deep, sectoral or involve 360° of the cornea. In contact lens users, a small amount (1mm to 2mm) of peripheral superficial vascularization is common; however, having growth or progression of more than 2mm or involving a middle or deeper stroma is not common. Although rare, deep stromal vessel growth is of greater concern and can lead to significant complications. Vessel growth into the visual axis, although exceptionally rare, can lead to visual impairment via intracorneal hemorrhage, lipid exudation and scarring, all of which potentially compromise the patient’s vision.2,5
Prevention. Look for signs of a tight-fitting lens or conjunctival drag. Tight lenses tend to be comfortable initially, so it’s important to carefully evaluate lens fit. An excessively tight lens will show minimal or no post-blink movement. Perform the digital push-up test by raising the lower eyelid margin with the thumb to move the lens upward and then assessing speed of recentering and amount of digital force necessary to move the lens upward. A tight lens will be difficult to move during the test or the lens will recenter slowly. Also, look for conjunctival drag during the blink or push-up test. Encourage patients to adhere to appropriate wear schedules and avoid overnight lens wear as well as give their eyes regular breaks from lens wear.5
Management. Treatment may include switching to a better fitting lens, updating to lenses with higher oxygen permeability or reducing lens wear time. Overnight wear of contact lenses is uncommon these days, but patients should be strongly advised to limit lens wear to waking hours. In advanced cases, patients may need to stop wearing contact lenses altogether. Topical corticosteroids can be used to aid in vessel regression. In severe cases or when there is vessel growth into the visual axis, refer the patient to a cornea specialist.2,5
 |
|
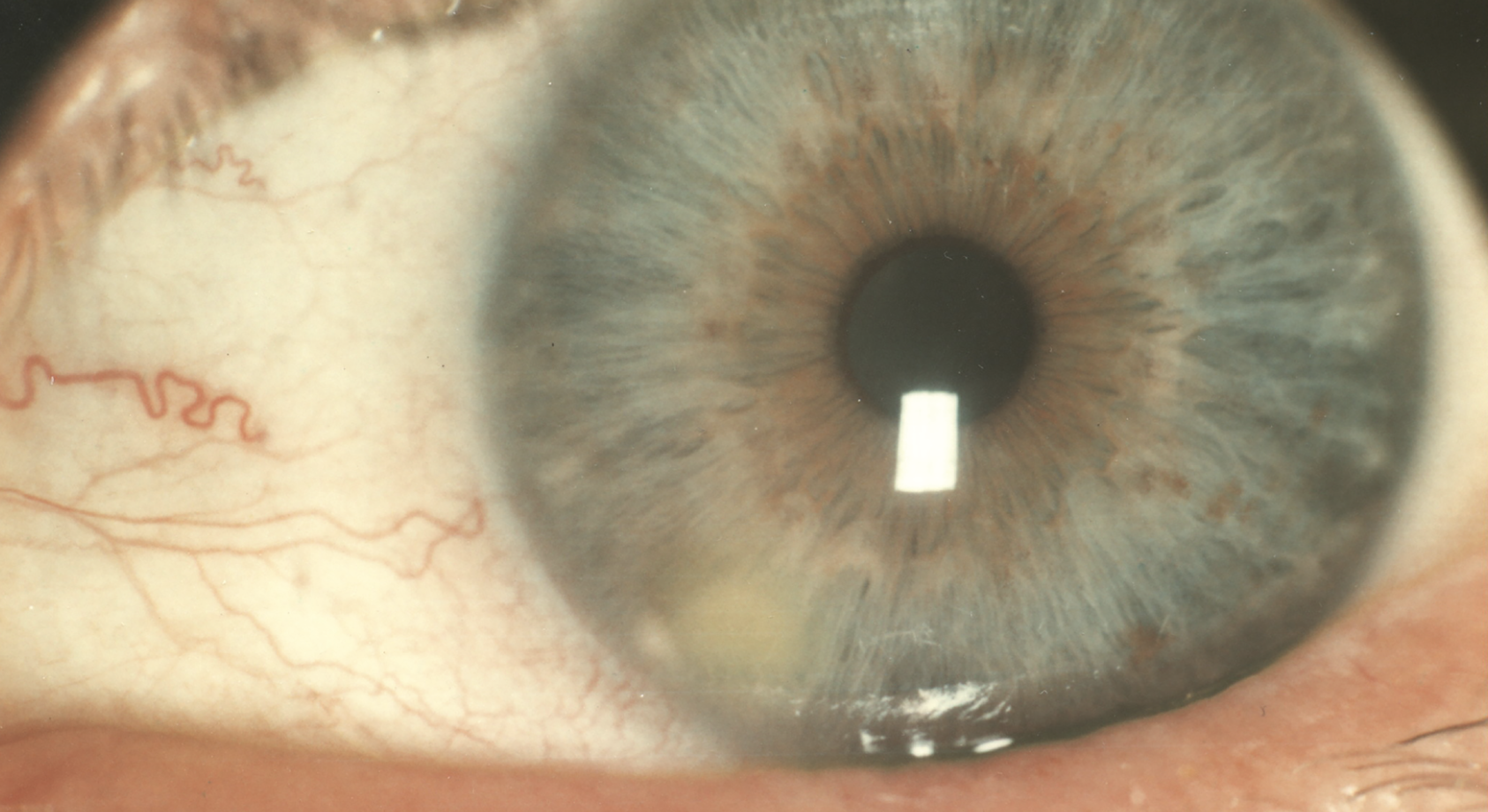
Fig. 2. Note the marginal infiltrate located at the periphery of the cornea, appearing as a small, localized white or grayish opacity, distinctly positioned near the limbus of the eye. Surrounding the infiltrate is a mild conjunctival injection, indicating a localized inflammatory response. This condition is typically associated with inflammatory processes, such as ocular surface disease or contact lens-related complications. Click image to enlarge. |
Sterile Corneal Infiltrates
Treatment for this complication depends directly on its origin, which may vary from case to case. Clinicians should familiarize themselves with the wide array of signs and symptoms, initiate the appropriate management plan as soon as possible and counsel patients on proper lens hygiene to avoid recurrence.
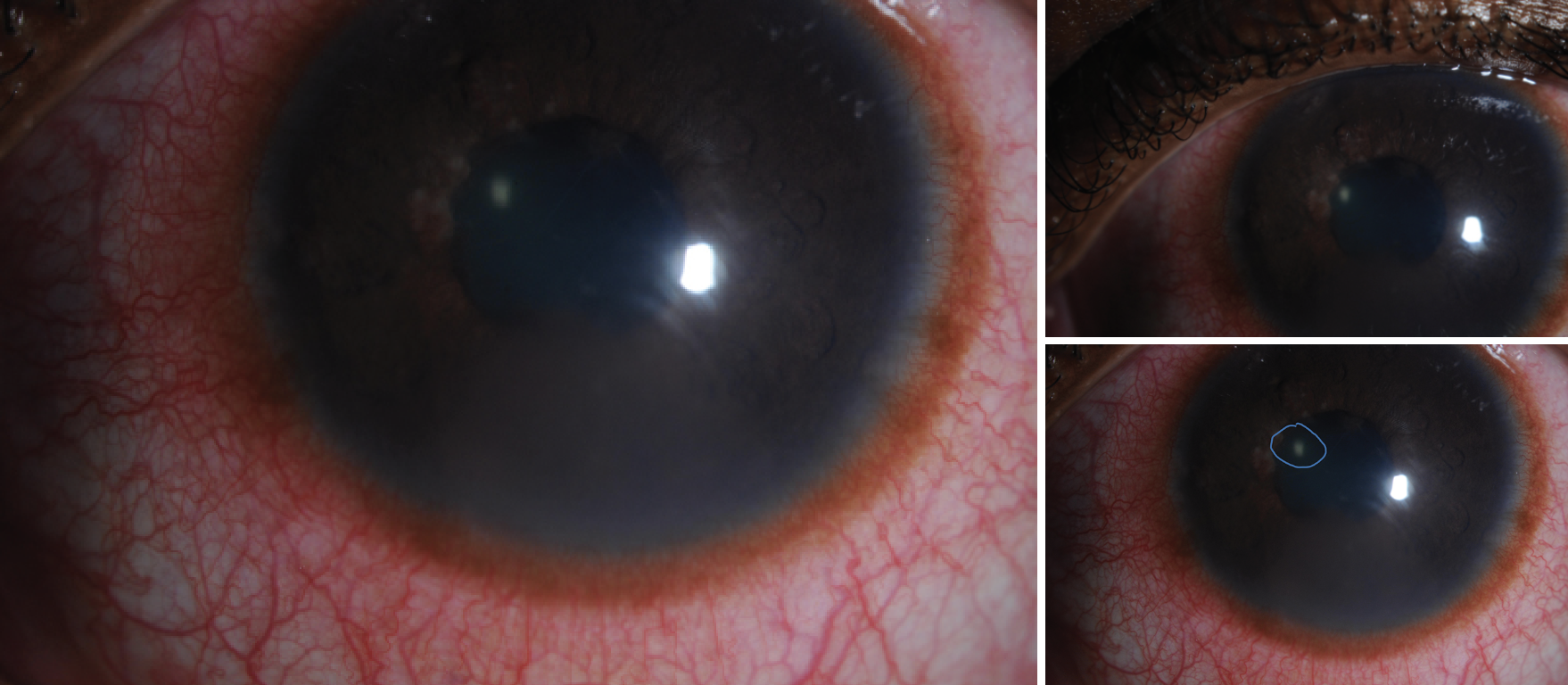
Recognition. These white or grayish opacities can be epithelial, subepithelial or anterior stromal, often resulting from an inflammatory response to contact lens wear, especially extended wear (Figures 2 and 3). Other risk factors include, but are not limited to, hypoxia, poor contact lens hygiene and lens case contamination. Symptoms can include mild to moderate pain, redness, tearing, photophobia and reduced visual acuity.
It is important to note that corneal infiltrates can be sterile or infectious in origin. Differentiation is critical to ensure appropriate treatment and prevent complications. Often, the patient history, symptoms and clinical signs are key factors in distinguishing between sterile and infectious infiltrates.2,3,6,7 Under the slit lamp, sterile corneal infiltrates are typically seen as small, localized spots in the peripheral cornea with little to no epithelial staining and can be associated with other signs of inflammation, such as conjunctival injection.2,3,6,7
Prevention. Avoiding corneal infiltrates involves proper lens hygiene, forgoing overnight wear and ensuring appropriate lens fit and material. Encourage patients to adhere strictly to lens replacement schedules and to avoid using expired or damaged lenses and solutions. Daily disposable lenses can reduce the risk by eliminating the need for cleaning and minimizing the chance of contamination.2,3,6
 |
|
Fig. 3. A close-up view of a patient’s eye reveals an infectious corneal infiltrate with a moderately severe conjunctival injection. The cornea appears slightly hazy, with a distinct grayish-white spot indicating the presence of an infiltrate. Click image to enlarge. |
Management. Regardless of the etiology of the infiltrate, patients should be instructed to immediately discontinue contact lens use to prevent further irritation and allow the cornea to heal. Sterile infiltrates resulting from inflammation of the cornea can be treated with topical steroids. However, if there is a suspicion of a bacterial infection or if the infiltrates are accompanied by epithelial defects, antibiotic drops should be prescribed; a commercially available fluoroquinolone is usually adequate. Lubricating eye drops can help alleviate discomfort and promote healing by maintaining a moist ocular surface.
The patient should be monitored closely to confirm resolution of infiltrates and to ensure there are no additional complications. If infiltrates recur, reassess the lens material, fit, wearing modality, cleaning/disinfecting solution and patient’s compliance with care instructions.2,3,6
Corneal Abrasion
Characterized by scratches or injuries to the surface epithelium of the cornea, corneal abrasions represent the most common form of ocular trauma and often arise due to improper lens handling or wearing damaged lenses (particularly for GP lens patients). Once an abrasion is identified, prompt action helps minimize a patient’s risk of developing a potentially vision-threatening infection.
Recognition. Symptoms of corneal abrasion include sudden onset of severe eye pain, tearing, redness, light sensitivity and a gritty sensation. Patients may have difficulty keeping the eye open, making examination difficult.3,8
Prevention. Educate patients on proper lens handling and hygiene, emphasizing the need for thorough hand washing before inserting or removing lenses, and spend extra time reviewing proper insertion and removal techniques to avoid scratching the cornea. It is also important to recommend regular replacement of lenses according to the prescribed schedule and discourage use of damaged or torn lenses.3,8
Management. Patients should be treated with topical antibiotics to prevent infections—a fluoroquinolone or aminoglycoside is the drug of choice due to Pseudomonas coverage. Ointment formulations should be used for comfort while healing and for overnight use. Cycloplegics can also be administered in the office for pain control due to discomfort from ciliary spasm. Use lubricating eye drops or ointments to provide relief and promote healing. The patient should be monitored daily until resolved.3,8
Microbial Keratitis
This painful, sight-threatening infection moves fast—and so should you. Here’s guidance on diagnosing, preventing and managing this condition in contact lens wearers.
 |
|
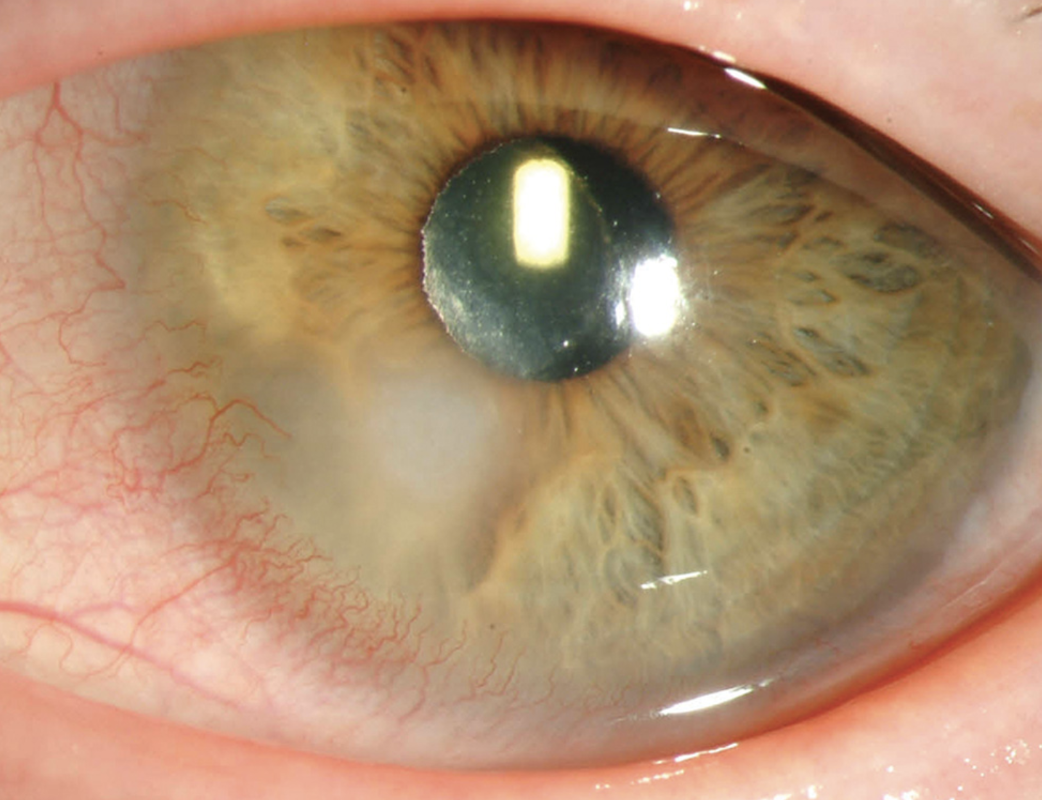
Fig. 4. Extended contact lens wear and poor hygiene practices, such as using tap water to clean lenses, can result in MK, often of a bacterial etiology. Photo: University of Iowa. Click image to enlarge. |
Recognition. Microbial keratitis (MK) can result from bacterial, viral, fungal or amoebic infections, as well as noninfectious sources like trauma or extended contact lens wear (Figure 4). In contact lens wear, the etiology is most often bacterial.
Signs and symptoms include pain, redness, blurred vision, photophobia, tearing, discharge, tear film debris and anterior chamber reaction. Patients may also notice a white or grayish spot on the cornea and experience a gritty or foreign body sensation in the eye. Visual acuity can be significantly reduced in severe cases.
MK is one of the most serious complications of wearing contact lenses. For an infection of the cornea to occur, the offending organism must bind to and penetrate the corneal epithelium. Contact lens–induced hypoxia can cause compromised corneal epithelial integrity, impaired wound healing and increased bacterial binding, which may predispose a patient to infection. Patients will experience moderate to severe pain, photophobia, redness and discharge.
Slit lamp findings will show a focal, irregular stromal infiltrate greater than 1.5mm in size in the central, midperipheral or peripheral cornea, along with diffuse infiltration and an overlying epithelial defect. Other findings include lid edema, diffuse general and limbal conjunctival injection, anterior chamber reaction and possible hypopyon. Without proper antimicrobial treatment, patients will worsen rapidly.2,3,9-11
Prevention. As with so many of these complications, the best way to ensure prevention is to educate patients on the importance of proper lens hygiene, avoiding overnight wear (unless using lenses specifically designed for it) and avoiding contact with nonsterile water while wearing lenses. Daily disposable lenses can significantly reduce the risk of infection by eliminating the need for cleaning and reducing the chance of contamination. In addition, solution efficacy is important, especially for those not using daily disposables. Ensuring the use of effective and appropriate contact lens solutions can help reduce the risk of infection.2,9-11
Management. Regular and prompt evaluation of patients presenting with keratitis is essential to determine the appropriate treatment and prevent long-term complications. Discontinuing contact lens use immediately is critical. When treating noninfectious keratitis, lubricating drops or ointments alleviate discomfort and promote healing, anti-inflammatory drugs reduce redness and discomfort and prophylactic antibiotics prevent secondary infections.
For noninfectious keratitis, such as contact lens–induced red eye without an infectious component, superficial punctate keratitis and some autoimmune-related keratitis, steroids are appropriate to reduce inflammation and alleviate symptoms. Monitor the patient closely for signs of improvement and potential side effects such as increased intraocular pressure or secondary infections. For suspected herpetic infections, start topical antivirals.
For infectious keratitis, prompt treatment with appropriate antimicrobial agents is essential. In cases of bacterial keratitis, broad-spectrum antibiotic eye drops such as fluoroquinolones (e.g., moxifloxacin) are the first line of treatment. In more severe or unresponsive cases, fortified aminoglycosides or cefazolin may be necessary.
Establishing a definitive diagnosis through cultures and corneal scrapings is crucial to guide therapy. Not all cases of MK are cultured at diagnosis; however, culturing should be considered for centrally located lesions, lesions larger than 2mm, cases where empirical fluoroquinolone therapy has failed and any monocular or immunocompromised patient. If your office is not equipped to culture, referral to a cornea specialist is appropriate.
Regardless of culturing, immediate treatment with a fluoroquinolone is essential. If a patient was cultured, the treatment regimen may be altered based on species and sensitivity reports. Steroids should generally be avoided initially until the infection is controlled with appropriate antibiotics. Once the infection is under control, steroids can be introduced to reduce inflammation and prevent scarring, but this should only be done under close supervision.
Acanthamoeba keratitis should be considered in patients with known exposure to fresh water (e.g., swimming in a lake) or tap water, disproportionate pain relative to clinical appearance or cases not responding to antibiotics. Close follow-up is essential to monitor healing and prevent complications. Referral to a cornea specialist is warranted if you suspect any of the following:
- atypical or complicated cases, such as suspected fungal or Acanthamoeba
- if the keratitis does not respond to initial treatment within a reasonable time frame
- if the keratitis is severe with extensive corneal involvement or along the visual axis
- if there is a high risk of complications such as corneal scarring, neovascularization or perforation
Cases that may require long-term immunosuppressive therapy, specialized medical management or surgical intervention (i.e., corneal transplantation) should also be managed by a cornea specialist.2,3,9,10
Takeaways
Contact lenses offer clear vision and convenience but not without potential complications, most of which result from poor patient compliance and hygiene. These complications can be effectively managed through proper recognition, prevention and prompt intervention. Carefully assess each case’s severity, response to treatment and potential complications to determine the best course of action. Furthermore, educate patients regularly on the importance of proper lens care, adherence to wear schedules and regular eye exams. By doing so, eyecare providers can significantly reduce the incidence of contact lens complications and help patients maintain optimum ocular health and vision.
Dr. Attar is an associate professor and director of optometric services at the University of Mississippi Medical Center in Jackson, MS. She is the sole optometrist at the state’s esteemed medical school and holds dual doctorates in optometry and health administration, complemented by an MBA. Dr. Attar is a fellow of the American Academy of Optometry, chairs the AAO Retina Special Interest Group and is the vice chair of the American Optometric Association Leadership Development Committee. Her achievements have been recognized through numerous awards, including Mississippi Young OD of the Year, SECO Young OD of the Year, AOA Young OD of the Year and Women in Optometry Young OD of the Year. Dr. Attar is on advisory boards for Heidelberg Engineering, Apellis and OcuTerra Therapeutics and is on the speaker bureau for Tarsus Pharmaceuticals.
1. Golden MI, Meyer JJ, Zeppieri M, Patel BC. Dry eye syndrome. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. February 2024. www.ncbi.nlm.nih.gov/books/NBK470411. 2. Hashmi MF, Gurnani B, Benson S. Conjunctivitis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; January 2024. www.ncbi.nlm.nih.gov/books/NBK541034. 3. Sharif Z, Sharif W. Corneal neovascularization: updates on pathophysiology, investigations and management. Rom J Ophthalmol. 2019;63(1):15-22. 4. Gurnani B, Kaur K. Contact lens-related complications. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. June 2023. www.ncbi.nlm.nih.gov/books/NBK587443. 5. Baum, Jules M.D.; Dabezies, Oliver H. Jr. M.D. Pathogenesis and treatment of “sterile” midperipheral corneal infiltrates associated with soft contact lens use. Cornea. 2000;19(6):777-81. 6. Steele KR, Szczotka‐Flynn L. Epidemiology of contact lens‐induced infiltrates: an updated review. Clin Exp Optom. 2017;100(5):473-81. 7. Domingo E, Moshirfar M, Zeppieri M, et al. Corneal abrasion. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. January 2024. www.ncbi.nlm.nih.gov/books/NBK532960. 8. Efron N. Contact Lens Complications E-Book. Elsevier Health Sciences. 2018. 4th Eds. 9. Sharma SP, Dwivedi S, Kumar S, et al. Bacterial and fungal keratitis: current trends in its diagnosis and management. Current Clinical Microbiology Reports. 2023;10(4):1-13. 10. Gurnani B, Kaur K. Bacterial keratitis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. January 2024. www.ncbi.nlm.nih.gov/books/NBK574509. 11. Verani JR, Lorick SA, Yoder JS, et al. National outbreak of Acanthamoeba keratitis associated with use of a contact lens solution, United States. Emerg Infect Dis. 15(8):1236-42. |

