 |
A 71-year-old Caucasian female presented for a diabetic eye screening. She was diagnosed with type 2 diabetes about one year ago, and her endocrinologist told her that she needed to get an eye exam. She was on metformin 500mg per day and reported good blood sugar control. Her previous eye exam was one year earlier in a retail setting where she was told that she needed to be seen by a specialist.
On examination, the patient’s entering distance acuities measured 20/20 OD and 20/20 OS. Her extraocular motility testing was normal. Confrontation visual fields were full to careful finger counting OU. The pupils were equally round and strongly reactive; there was no afferent pupillary defect. The anterior segment examination was unremarkable.
Dilated fundus exam of the right eye was normal, while the left eye showed changes (Figures 1 and 2). An OCT was obtained and is also available for review (Figure 3).
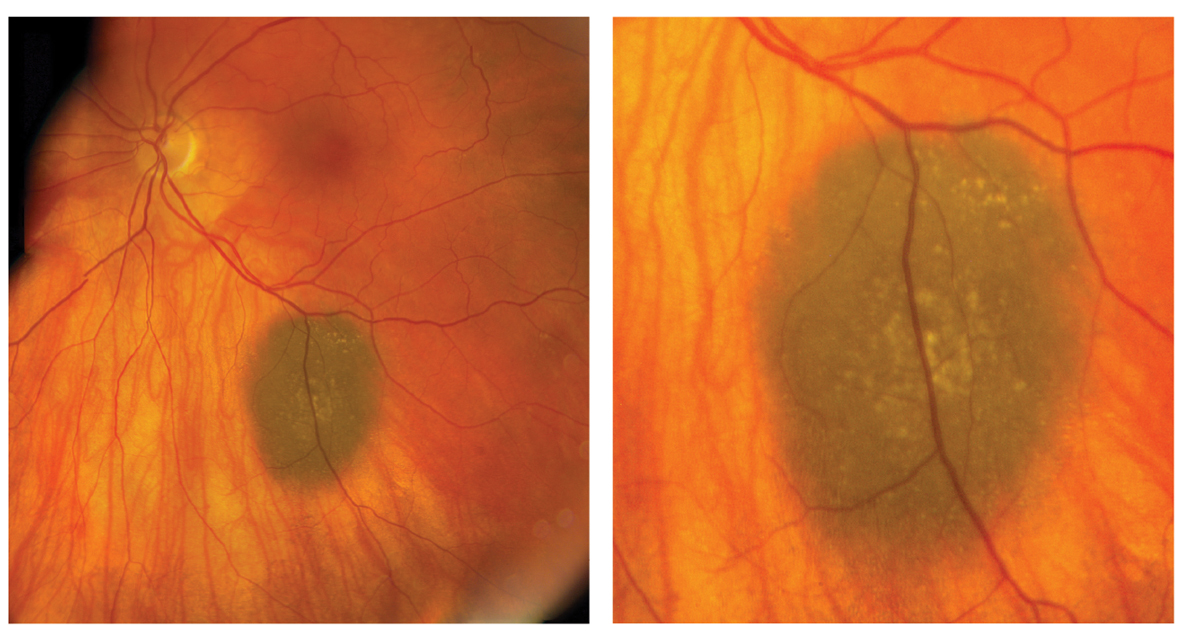 |
| Figs. 1 and 2. These are the fundus photographs of the left eye of our patient. What do they represent?” Click image to enlarge. |
Take the Retina Quiz
1. What is the most likely diagnosis for this patient?
a. Choroidal nevus
b. Choroidal melanoma
c. Melanocytoma
d. Metastatic carcinoma
2. What additional testing would be helpful in this patient?
a. Fluorescein angiogram
b. Ultrasound
c. Liver function testing
d. Chest X-ray
3. How should this patient be managed?
a. Observation
b. Enucleation
c. Plaque radiotherapy
d. Chemotherapy
4. What is your estimate of the likelihood the lesion will grow over the next five years?
a. Very low
b. Mild chance–about 25%
c. Significant chance–50%
d. Very high
5. What is the overall prognosis for this patient?
a. Very poor
b. Moderate
c. Excellent
d. Uncertain to determine
For answers, see below.
Discussion
The slate gray-pigmented lesion along the inferior arcade in the left eye is suspicious. However, on stereoscopic evaluation, you could tell that it is flat. What’s more, there are drusen overlying it that indicates the lesion has been present for a while. It’s also important to note there is no orange pigment or lipofiscin present, which is not a good prognostic indicator and is often seen with choroidal melanoma. Given this presentation, our patient has a choroidal nevus.
Choroidal nevi are developmental tumors that are usually found as an incidental finding during a routine eye examination. In appearance, 95% of choroidal nevi are flat, slate gray and less than three disc-diameters in size. Choroidal nevi are made up of benign spindle cells and branched melanocytes.
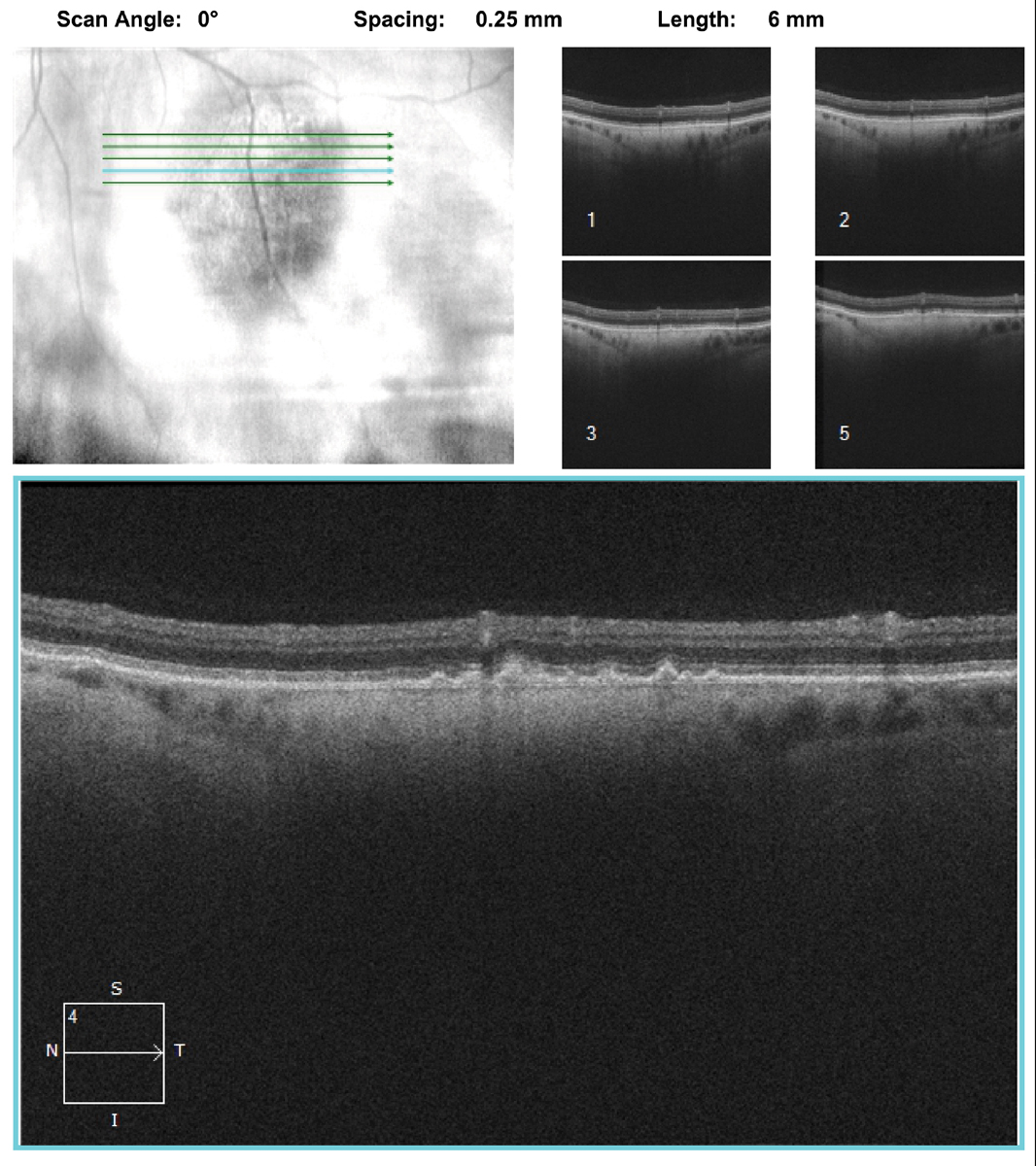 |
| Fig. 3. Note the changes in the choroid on the OCT through the lesion. What do they represent? Click image to enlarge. |
A Closer Look
In most instances, the diagnosis of a choroidal nevus is straightforward, and there is little or no concern that the lesion is a choroidal melanoma. However, that’s not always the case, especially as choroidal nevi can have features that make it more difficult to distinguish between a benign nevus and a small malignant melanoma.
On clinical exam, it’s not always easy to determine if the lesion is flat or minimally thickened. Fortunately, OCT can often help. Though not designed for tissue differentiation (like the standardized A-scan), the OCT can help determine if there is elevation, or if fluid is present.
Indeed, in our patient, we can see the nevus is flat but, interestingly, we can also see the posterior contours of the lesion within the choroid. This is a more dense or a homogenous localized area posterior to the retinal pigmented epithelium (RPE) within the choroid. Standardized A- and B-scans would be great additional tests for this patient, but they’re not critical, as the OCT and clinical exam provide the necessary information to make the right diagnosis.
In addition to the presence of overlying drusen, other clues that may be helpful in differentiating a suspicious nevus from a small melanoma include the presence of RPE hyperplasia or atrophy, bony pigment spicules and even choroidal neovascularization. Any of those findings are signs of chronicity and suggest that the lesion has been present for some time. An actively growing melanoma does not have time to develop these more chronic changes.
In contrast, most melanomas are usually over 3.0mm in thickness, can be variably pigmented and may have lipofuscin present, which, as discussed earlier, suggests greater malignant potential. Ultimately the best way to determine if a suspicious lesion is a melanoma or a nevi is to take a photograph and document growth of the lesion over time. Choroidal nevi will rarely show any significant growth.
Risk Factor Features
A question that often gets raised: do melanomas develop from transformation of preexisting nevi, or are they in fact separate entities? Most experts agree that the vast majority develops as separate entities. Malignant transformation from preexisting nevi is exceedingly rare, occurring between one in 4,800 to one in 8,800 individuals.1 In one retrospective analysis of approximately 1,300 patients with small melanocytic lesions less than 3.0mm in thickness, the authors identified five factors associated with risk for growth: (1) tumor thickness greater than 2.0 mm; (2) subretinal fluid; (3) visual symptoms; (4) orange pigment; (5) posterior tumor margin touching the disc.2
In patients who had no risk factors, lesion growth was observed in only 4%.2 Growth occurred in 36% of patients who had at least one risk factor, and in 50% of those with three or more risk factors.2 These features may be remembered more easily using the mnemonic “To Find a Small Ocular Melanoma”.2 Clinical factors associated with an increased risk of metastasis included: (1) posterior margin touching the disc; (2) documented growth; and (3) increased tumor thickness (at least 1.1mm).3
In our patient, we were able to determine that her nevus was discovered over 10 years ago. Though we didn’t have any old fundus photos to compare with, the fact that it was noted that long ago is further confirmation that this is just a nevus and will likely not change over time. She did not have diabetic retinopathy, but we did explain the importance of good blood sugar control and the importance of annual follow-up exams, given that she has a choroidal nevus as well as the long-term risk of developing diabetic retinopathy.
Retina Quiz Answers
1) a; 2) b; 3) a; 4) a; 5)c.
1. Singh AD, Kalyani P, Topham A. Estimating the risk of malignant transformation of a choroidal nevus. Ophthalmology. 2005;112: 1784-9. 2. Shields CL, Shields JA, Kiratli et al. Risk factors for growth and metastasis of small choroidal melanocytic lesions. Opthalmology. 1995;102:1351-61. 3. Shields, CL, Cater JC, Shields JA, et al. Combination of clinical factors predictive of growth of small choroidal menalocytic lesions tumors. Arch Ophthmol. 2000; 118:360-4. |

