 |
Q:
A patient presented with a history of accidentally getting eucalyptus oil in both eyes, with subsequent corneal abrasions. What is a good protocol for handling chemical burns?
A:
Chemical burns to the eye are an emergency all optometrists should feel comfortable treating and managing, says Trennda Rittenbach, OD, staff doctor at the Palo Alto Medical Foundation. It is critical to train your front office and phone staff to get these patients in immediately when they call. The first and most important step is copious irrigation of the eye with any brand of sterile irrigating solution, something you should stock in every exam lane. “Evert the upper and lower lids to irrigate all parts of the eye and adnexa, as chemical could remain trapped in the lower cul-de-sac or under the upper lid,” she advises. Use litmus paper five to 10 minutes after irrigation in order to determine the pH. It is imperative to continue irrigation until the pH is neutralized.
Dr. Rittenbach cautions that a careful corneal exam, along with the conjunctiva and anterior chamber, is critical in order to not miss any collateral damage. “I commonly see oil splash burns from cooking that result in first- and sometimes second-degree burns to the eyelids, so also carefully examine the adnexa,” she advises. Pay attention to intraocular pressure (IOP) readings, as alkaline chemical burns may cause immediate or delayed rises. Alkaline chemicals can penetrate the eye more easily due to their lipophilic nature, therefore can also damage the trabecular meshwork, ciliary body and possibly the lens.1
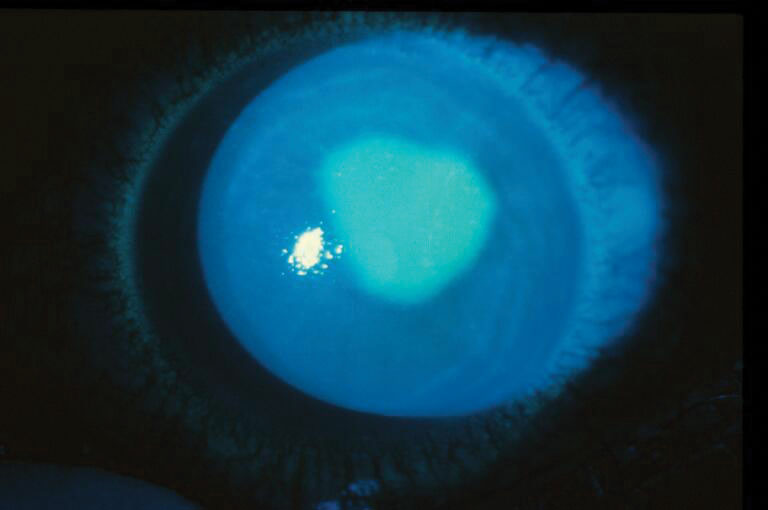 |
| Chemical burns can create painful epithelial defects. Photo: Brian Den Beste, OD. Click image to enlarge. |
Investigate the Agent
This particular patient was rubbing eucalyptus oil onto his forehead for religious reasons, and it ended up in both eyes. This resulted in severe pain from bilateral epithelial defects centrally extending to the periphery OU. “After doing some quick research, I was able to find that an alcohol-based agent is sometimes used in non-pure forms of essential oils,” Dr. Rittenbach notes.
Acidic chemicals that commonly cause ocular injuries are battery acid, acetic acid such as nail polish remover or vinegar, toilet bowl cleaners and some swimming pool agents. A very common injury optometrists see is from hydrogen peroxide–based contact lens solutions. Some common alkaline substances that can cause serious ocular injuries are oven cleaner, drain cleaner, chlorine bleach, lime found in plaster, cement and mortar, and ammonia products usually found in cleaning products and fertilizer. Get a detailed history and ask the patient to bring in the product they got into their eye(s).
Treatment will depend on clinical signs, and ranges from frequent lubrication and topical steroids to amniotic membranes. Autologous serum tears may be necessary if there has been a loss of limbal stem cells. If the IOP is elevated, be sure to manage that as well.
The patient did well with erythromycin ointment every four hours and Refresh Celluvisc (carboxymethylcellulose sodium 1% gel, Allergan) six to eight times per day, according to Dr. Rittenbach. The next day, slit lamp exam showed immense improvement with only a small central area of epithelial loss. By day six, the epithelium was completely healed.
It is vital to assess the presence and degree of limbal ischemia as well as any opacification of the cornea. An injected conjunctiva puts one a little more at ease. Blanching can indicate ischemia, usually associated with an alkali burn, that can lead to limbal stem cell loss and tissue necrosis. These patients may have a poor outcome with corneal scarring, loss of vision and life-long dry eye and may possibly need surgical intervention such as a corneal transplant.
A white, blanched eye or a cornea that is not healing quickly warrants a referral to an anterior segment or cornea specialist.
Dr. Ajamian is the center director of Omni Eye Services of Atlanta. He currently serves as general chairman of the education committee for SECO International. He has no financial interests to disclose.
1. Baradaran-Rafii A, Eslani M, Haq Z, et al. Current and upcoming therapies for ocular surface chemical injuries. Ocul Surf. 2017;15(1):48-64. |

