In the United States, around 30% of soft contact lens (CL) fits are toric (most often in tandem with correction of ametropia), while 47% of patients receive a spectacle correction of 0.75 diopters of cylinder (DC) or greater in at least one eye.¹,² For astigmats, adequately correcting their astigmatism is the priority to provide clear vision.3 And yet, astigmatism may very well be the most idiosyncratic optical problem we encounter, surpassing myopia, hyperopia and even presbyopia in the uniqueness of how it manifests for each patient. Our approach to correction should be equally patient-specific.
Decisions regarding how best to correct astigmatism with contact lenses, including fitting strategies and lens modalities, are driven by numerous factors. Considerations include total amount of astigmatism, the amount of refractive vs. corneal astigmatism and cylinder orientation—specifically, with-the-rule (WTR), against-the-rule (ATR) or oblique. It’s also critical to understand each patient’s visual demands and goals for lens wear. To reduce chair time, this article will discuss the most appropriate CL designs to address various types of astigmatic correction.
 |
|
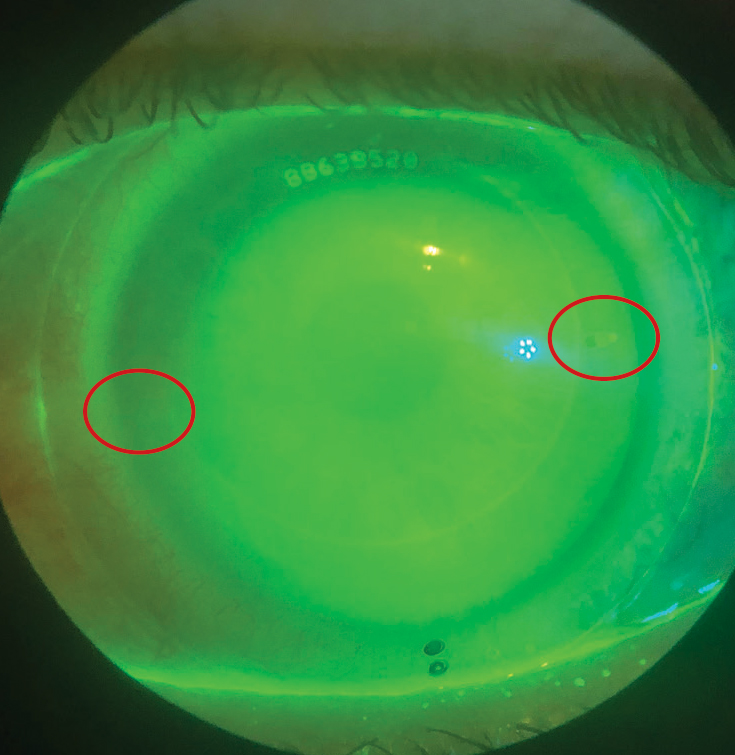
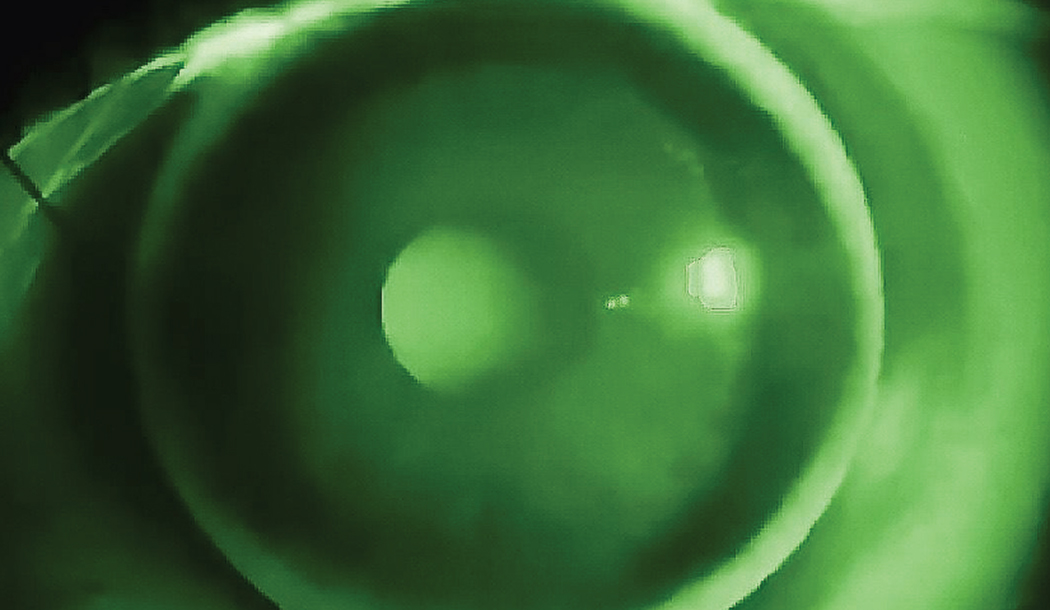
Fig. 1. This scleral has toric haptics. The flat meridian is denoted by hashmarks, which are rotated 15⁰ counterclockwise. Click image to enlarge. |
Case #1: The "Average" Astigmat
A 21-year-old female presents for a CL exam, wearing aspheric monthly replacement soft contact lenses. She is satisfied with the comfort but not her vision, noting that her glasses provide better acuity. She reports difficulty taking notes from the back of her college lecture hall but finds it challenging to wear her glasses due to fogging from mask wear.
Entering VA with CLs:
OD -2.00DS 20/20-3
OS -4.00DS 20/25
Refraction: OD -1.75 -0.50x005 20/20
OS -3.75 -1.00x015 20/20
Topography Sim Ks:
OD 44.25/44.25@95
OS 44.50/44.50@90
Given this patient’s vocational needs, it makes sense to fit her in lenses that will correct her astigmatism.
Spherical and aspheric lenses do not significantly “mask” corneal astigmatism.⁴ It was shown that for larger pupils (i.e., over 2mm), aspheric lenses did not provide adequate vision compared to toric CLs even in patients with 0.75 to 1.0DC.⁴ High myopes and hyperopes benefit from correction of even small amounts of astigmatism. It’s outdated to simply prescribe the spherical equivalent in patients whose refractive cylinder is less than or equal to 1/4th the spherical component of the refraction. It was reported that 71% of patients with astigmatism in the 0.75DC range prefer toric correction and that low astigmats benefit from full correction of their astigmatism.5,6 Comparing K readings to total refractive error is an important step to determine whether to refit into gas permeable (GP) lenses (and what type) vs. a toric soft contact lens.
Mass-produced soft CLs start with -0.75DC, so in deciding whether to proceed with a toric soft lens for her right eye, attention was paid during her refraction Jackson cross-cylinder (JCC) testing. For her right eye, she oscillated between 0.50DC and 0.75DC and in the left between 0.75DC and 1.00DC, indicating she would benefit more from toric correction in her CLs which matches her chief complaint. By demonstrating monocularly in the phoropter the difference between the full astigmatic correction vs. spherical equivalent, she noted a significant difference in clarity, which also confirms she is sensitive to residual astigmatism (RA).
Since her keratometry readings indicate spherical corneas, her refractive astigmatism is attributed to lenticular astigmatism and spherical GPs may not provide good clarity. We therefore fit her into soft toric CLs.
Final CL Rx:
OD 8.6/14.5/-1.50 -0.75x010 20/20
OS 8.6/14.5/-3.75 -0.75x010 20/20
Our Fitting Protocol for Soft Toric Contact lenses1. When choosing a trial lens, it’s always best to prioritize matching the axis, followed by the cylinder amount and sphere power. 2. For the axis, round towards 180 for WTR and 90 for ATR astigmatism. In case #1, we would round to axis 180 OD and 10 OS. 3. When working with the cylinder power that is between options, we generally round down because most rotate ~5° on average and this will decrease visual distortion.⁷ When going down on the cylinder power, it’s customary to then round up on the sphere to maintain the spherical equivalent power. For example, when fitting the patient in case #1, for OS we would pull -4.00 -0.75x10 from the fitting set, but for the OD, since the only choice we have is to over-correct the cyl at -0.75DC, we would compensate by going down on the sphere power and pull -1.50 -0.75x180). Lastly, be aware that there may be flexure along the power meridian, depending on the lens design and thickness, and often the patient requires less astigmatism for that reason alone. 4. For patients under the age of 40, round up the sphere when the fitting set only comes in -0.50D steps. For those over 40, round down. 5. For stable axis misalignment due to CL rotation, remember the acronym “LARS”: Left Add, Right Subtract. If the lens rotates clockwise, this is considered left rotation and the degree of rotation is added to the spectacle axis. Counterclockwise rotation is right rotation and requires subtracting. In case #1, the right trial lens rotated 5° left, so we add 5° to the refractive axis to come up with 10°. When the patient applies this 2nd trial lens, it should still only rotate 5° left. We aren’t trying to eradicate the rotation itself; instead, we are simply changing the optical orientation of the lens to improve vision. The higher the cyl power and/or the higher the percentage of the Rx that is composed of cyl, the more precision in axis location is needed for good visual acuity; conversely, the more axis misalignment there is, the worse the acuity will be.⁸ |
Case #2: The “Moderate” Astigmat
A 44-year-old male primarily wears glasses, and occasionally two-week disposable CLs, which he wished to update. His occupation requires him to be in front of the computer more than nine hours a day. Summer is coming and he wants to have contact lenses to wear for sports like baseball and golf but also admits to having bad environmental allergies.
Refraction: OD -0.50 -2.50x105 20/20
OS -0.50 -2.50x075 20/20
Topography Sim Ks:
OD 45.50/44.00@15
OS 45.75/44.00@165
In this case, refractive astigmatism is significantly greater than corneal astigmatism, and most GP options are likely suboptimal to adequately correct residual astigmatism (RA). A hybrid design GP cannot have the RA incorporated into the CL, as front toric optics don’t exist. There isn’t enough corneal cylinder for a back or bitoric GP, and a front toric GP can be less comfortable or have problems with stability. In addition, the patient is looking for part-time wear and adaptation to GPs is easier with consistent wear. Sclerals would allow for good stability and incorporation of front surface toricity, but he prefers something low maintenance.
This patient would benefit from the convenience and hypoallergenic nature of daily disposable toric CLs. Since mass-produced contact lenses only come in 10° steps, it is impossible to exactly align the CL axis with the refractive axis. Fortunately, the lenses displayed stable rotation of 5° to 10° to the right OD and 5° to 10° to the left OS, providing better axis alignment and a visually favorable outcome.
Final CL Rx:
OD 8.5/14.3/-0.50 -2.25x100 20/20
OS 8.5/14.3/-0.50 -2.25x080 20/20
 |
|
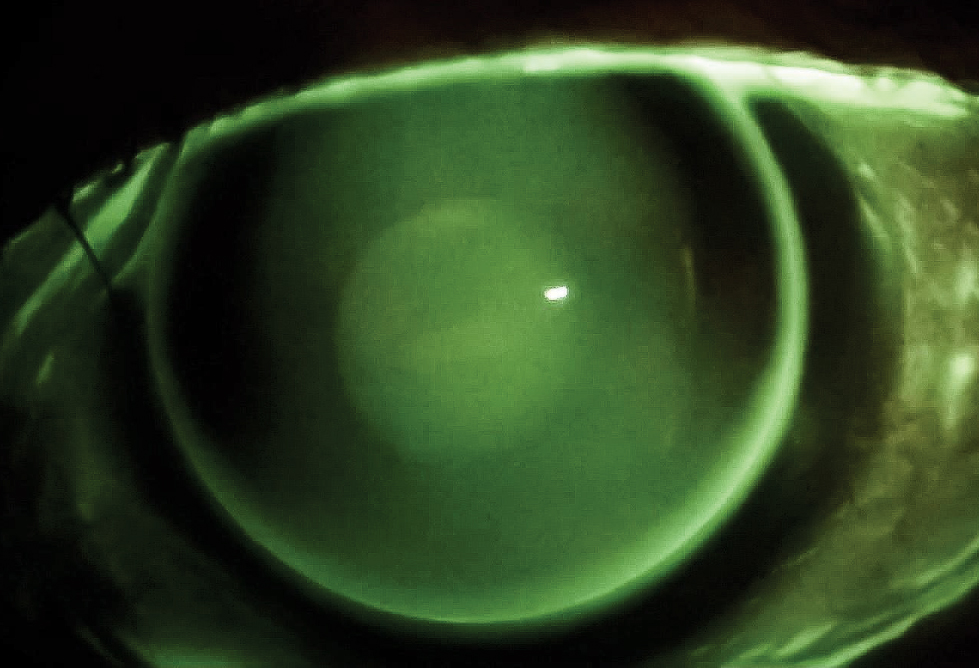
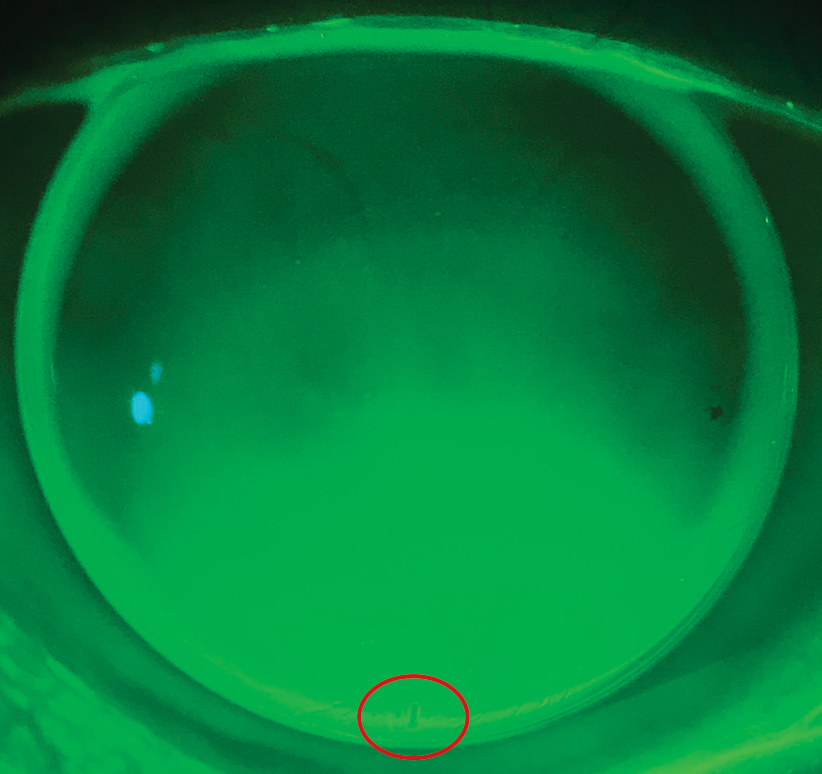
Fig. 2. Evaluation revealed a high-riding, lid-attached fit. There was a dumbbell-shaped fluorescein pattern with pooling in the vertical meridian and bearing in the horizontal indicative of WTRA. This is how a spherical GP looks on a toric cornea. Photo by John Gelles, OD. Click image to enlarge. |
Case #3: The Astigmat Who Has “Tried Everything”
A 17-year-old male presents for a contact lens fitting. He’s been seen at two practices over the last eight months and says that after trying numerous designs, no CLs have been comfortable nor delivered vision as clear as his glasses. He plays varsity baseball and doesn’t like the appearance of sport goggles. After reviewing his previous records, it appears he has tried most of the commercially available soft toric CLs.
Refraction:
OD +6.00 -1.50x120 20/20
OS +6.00 -1.75x064 20/20
Topography Sim Ks:
OD 40.98@38/39.60@128 1.38D oblique
OS 40.89@148/40.15@58 0.74D oblique
The patient has a horizontal visible iris diameter (HVID) of 12.2mm and 6mm pupils in normal illumination and 7.5mm in dim illumination.
A patient complaining of vision fluctuation with every blink, despite trying multiple brands of toric soft contact lenses, is likely to have an unusual sagittal depth and corneal diameter. To achieve a better, more comfortable fit, match the sagittal depth and diameter of the cornea and the lens.⁹Sagittal depth of the cornea is impacted by HVID, eccentricity, corneal curvature and scleral shape, although HVID has the greatest impact.¹º For the same corneal curvature, the larger the cornea, the greater the sagittal depth and a larger diameter lens will be necessary for stability.
Most commercially available lenses have a diameter that ranges from 13.8mm to 14.5mm and are designed for an average cornea with an HVID between 11.6mm to 12.0mm. However, 50% of patients have an HVID that falls outside this range and may do better with a custom lens.⁹Custom designs can be ordered in nearly any sphere and cylinder powers in 0.1D steps and to 1° axis increments, as well as nearly any diameter and base curve (BC). This comes in handy for the visually discriminative patient and enables practitioners to fit a broad range of corneal curvature and diameter combinations.
This patient has a flatter than average corneal curvature, larger than average HVID (12.2mm), oblique astigmatism and large pupils, all of which contribute to his poor VA with toric lenses. The presence of RA, as well as the goal of wearing the lenses for sports, makes a corneal GP an undesirable choice; a dusty baseball diamond isn’t a good environment for comfortable GP wear. A hybrid design GP is again contraindicated, as front surface toricity is not available. That leaves either a custom soft toric or a scleral lens. A custom soft lens was elected due to his previous familiarity and schedule constraints.
When designing custom soft lenses, clinicians should calculate the lens diameter using the HVID + 3.0mm formula to ensure better stabilization.¹¹ At minimum, a 1.5mm overlap on either side of the cornea should be planned for, with 0.5mm to 1.0mm of movement on primary gaze. To enhance on-eye stability, the diameter can be increased or additional prism can be added to the ballasting design of the lens. This adds more weight to the lens to bring and keep the optics in place, which was necessary for this patient’s right eye due to the oblique axis of the astigmatism.
Unique to this case, the optic zone (OZ) needs to be made larger to accommodate his large pupil size. An increase of the OZ by 1mm resolved his complaint of glare and haloes in dim illumination.
When vision is less than adequate, it’s most efficient to check the fit first before doing an over-refraction. A poorly fitting or excessively rotating lens will diminish vision and cause an over-refraction to be variable and unreliable. First, perform spherical over-refractions, but if they don’t produce a visually significant improvement, perform a sphero-cylindrical over-refraction (SCOR). A cross-cylinder calculation to determine the new lens power can be obtained using a website, app, or lab consultation.
Final CL Rx:
OD 8.6/15.4/+7.00 -1.75x120/9.5 OZ/1.3 BD prism for stabilization
OS 8.8/15.2/+6.50 -2.00x74/9.5 OZ/1.0 BD prism for stabilization
 |
|
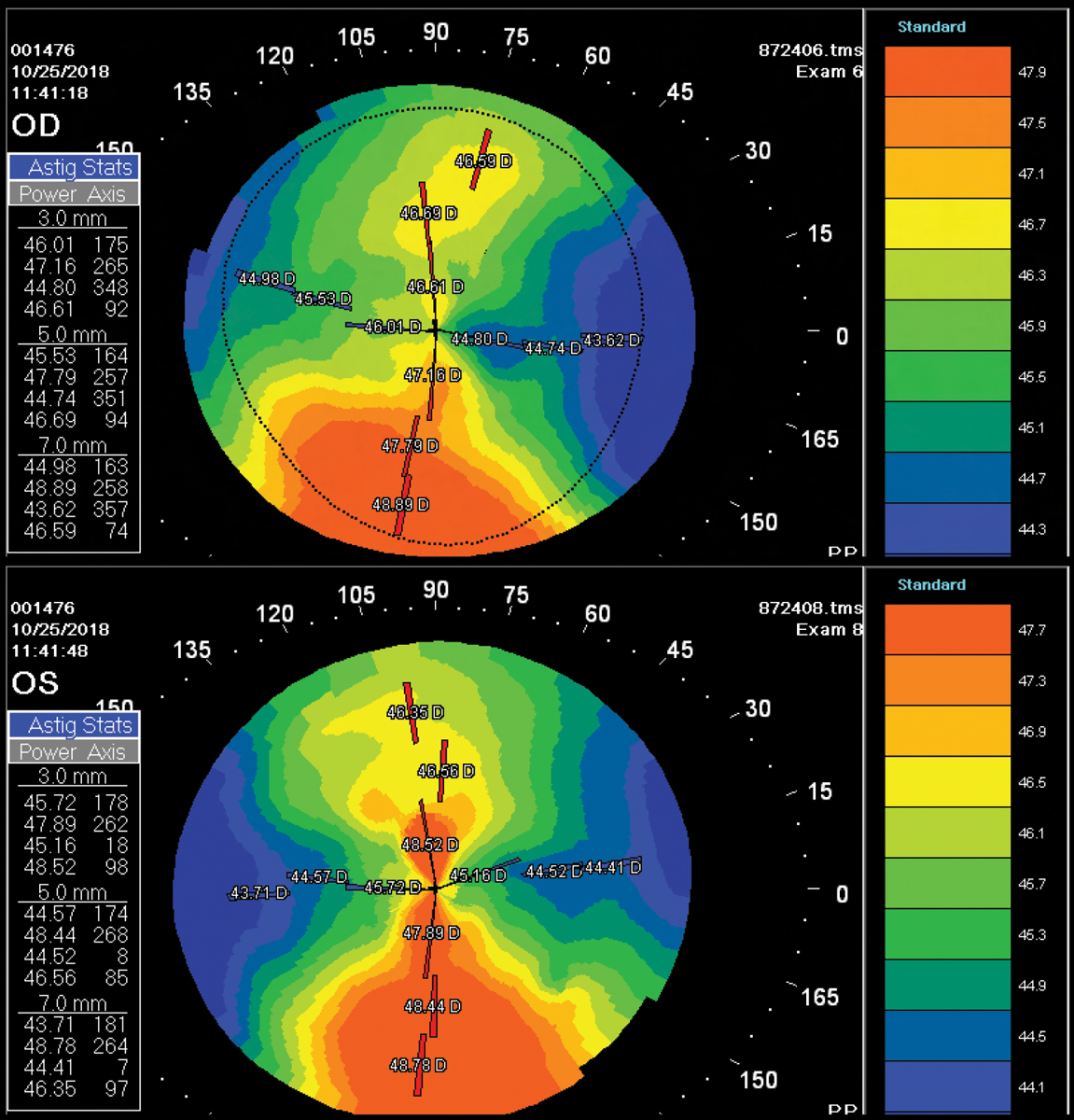
Fig. 3. Distorted corneal topography because of temporary corneal warpage from a high-riding GP contact lens. Click image to enlarge. |
Case #4: The Astigmat with Fluctuating Vision
A 15-year-old female presents for a contact lens evaluation and fit. She has noticed her vision fluctuating while playing tennis on her high school team. In addition, she feels her overall vision is sharper in her glasses than with contact lenses. The mother is concerned, as the patient will be learning to drive soon. She has been wearing quarterly replacement soft toric lenses the past two years after initially trying corneal GPs but struggling with comfort. The patient has a shy demeanor and is clearly worried about her vision.
Entering VA (CLs):
OD 20/30
OS 20/40
Refraction: OD +4.25 -1.75x005 20/20
OS +5.25 -2.00x178 20/25
Topography Sim Ks:
OD 43.17@101/41.04@11 2.13D WTRA
OS 43.08@82/40.82@172 2.26D WTRA
The patient has an HVID of 11.3mm and smaller fissures. She would benefit from a CL design that would provide consistent visual correction independent of lens rotation or movement. Her refractive astigmatism and corneal astigmatism are similar in both amount and orientation, and with both measuring ≤2.50D, she has a wide array of options. Since corneal GPs, sclerals and hybrid lenses all rely on the tear layer to correct astigmatism, they can correct her refractive error without inducing blur with lens movement.
Due to her past failure with corneal GPs and her smaller palpebral fissure width, she was refit into hybrid lenses. Hybrids are a standard 14.5mm diameter like that of mass produced soft toric CLs vs. sclerals, which are often larger and can be more cumbersome for handling, contributing to lower patient success.¹² In addition, since the application/removal process and care regimen of hybrids is like that of soft CLs, they provide minimal disruption for a habitual soft CL wearer and can be a natural transition for those patients hesitant to try something new but dissatisfied with their current lens modality.
Final CL Rx
OD 8.0/14.5/med/+4.00sph 20/20
OS 7.9/14.5/med/+4.50sph 20/25
Understanding the personality of the patient in addition to her refractive needs can help in finding the most suitable CL design. Most hybrid lenses can be empirically ordered, allowing patients a positive visual experience with their initial application. Studies have shown hybrid lenses are a good option for patients with moderate to higher amounts of regular astigmatism (provided there’s minimal residual astigmatism), and some patients experience better VA and contrast sensitivity and less glare compared to with soft toric CLs.1,13 In cases when the refractive astigmatism and corneal astigmatism are similar, but the patient is GP intolerant, hybrid contacts lenses are an excellent option to deliver stable, clear vision.
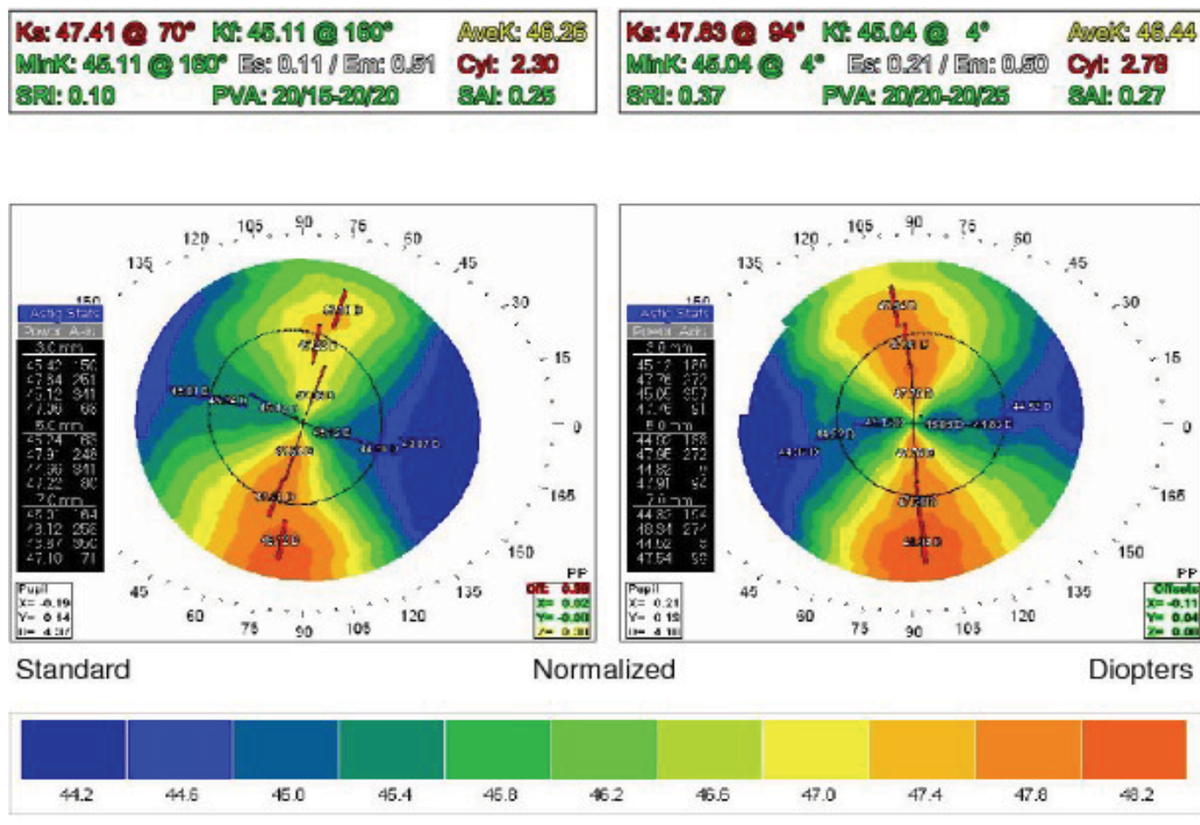 |
Fig. 4. The topography one week after cessation of CL wear. Click image to enlarge. |
Case #5: The New Wearer with High Astigmatism
A 14-year-old female, accompanied by her dad, has been referred for a CL fitting by her pediatric ophthalmologist. She is a high school freshman with no previous contact lens history but has worn glasses since age five. Her dad inquires about hybrid CLs, and her mom wears corneal GPs.
Refraction: OD +0.75 -4.50x002 20/20
OS +0.75 -4.25x170 20/20
Topography Sim Ks:
OD 44.51@94/40.37@004 4.14D WTRA
OS 45.05 @80/40.76@170 4.29D WTRA
It was evident during the refraction that the patient is sensitive to small cylinder power and axis adjustments. The high amount of refractive WTR astigmatism aligned with the measurements from corneal topography. As for the option of hybrid CLs, flexure was a concern given the amount of corneal astigmatism. A contact lens design with a toric back surface would provide a horse/saddle type fit, better aligning to the overall toric corneal shape. GP lenses were recommended with a discussion involving adaptation and highlighting all their benefits. It has been shown the manner in which GP contact lens options are presented has an impact on success of new GP wearers.15⁵
The patient was empirically fit in bitoric GPs:
OD 8.44/7.75/+1.00/-2.75/10.0
OS 8.33/7.67/+1.00/-2.50/10.0
Tangible Hydra-PEG coating can be added to the lenses to improve initial comfort and wettability, potentially assisting with adaptation for novice lens wearers, as in this case.¹⁶ The patient found insertion, removal and handling of the contact lenses easy. Empirical fitting of toric GPs is successful for patients with moderate to severe astigmatism.17 Using online fitting calculators, methods such as Mandell-Moore or laboratory consultants can aid in determining parameters, saving chair time. Although this patient ultimately required one minor adjustment to her left CL, the initial GPs ordered fit well, provided good vision and were dispensed, starting the patient down the path of lens adaptation.
Case #6: The High Astigmat with Anisometropia
A 30-year-old female grad student with a history of amblyopia OS is referred for a contact lens fit for her left eye. She presents wearing glasses, but says she suffers frequent headaches during wear. She was able to successfully wear a two-week replacement soft toric lens on her right eye but was unsuccessful OS with a custom soft toric, a bitoric GP and piggybacking of the bitoric GP.
Entering VAs (SRx):
OD 20/30-2
OS 20/50
Refraction:
OD -4.50 -3.00x180 20/25-2
OS +1.25 -7.25x174 20/40
HVID=11.7
Topography Sim Ks:
OD 45.95@90/42.85@180 3.1D WTRA
OS 48.00@86/42.25@176 5.75D WTRA
Sclerals are her final remaining option, but 1.00D of residual astigmatism is still expected because she has 6.75D of refractive astigmatism (after vertexing) and only 5.75D WTR corneal astigmatism. However, unlike hybrid lenses, sclerals can correct residual lenticular astigmatism and there’s no limit on how much corneal toricity can be corrected, since they vault the cornea. A scleral lens will provide her with good comfort and consistent vision.
The rotational stability of scleral lenses allows for reliable incorporation of front-surface toricity. Front toric optics can be incorporated into scleral lenses one of two ways: (1) prism ballasting by the same mechanism as corneal GP lenses or (2) using toric haptics for scleral alignment, as some degree of scleral toricity or asymmetry exists approximately in 94% of the population.¹⁸ Her corneal and scleral toricities are highly correlated, requiring not only a toric haptic but also toric limbal curves to improve scleral lens centration and alignment.19,20
Using a diagnostic fitting set that has toric haptics, the front toric optics could be ordered on the very first lens. This is done by taking note of the exact axis position of the laser markings indicating the flat meridian after the lens has settled on the eye for 20 minutes and performing a SCOR.
To determine a cylinder axis to compensate for any misalignment of the toric haptic, subtract the axis location of the flat meridian from the over-refraction axis. If the resulting value is positive, that is the correct cylinder axis to order; if negative, subtract that number from 180 to find which axis to order. For example, the toric hash marks were positioned at axis 15 (Figure 1), the SCOR over the -2.00DS diagnostic lens was +2.50 -1.00x175. Since 175-15=160, the final power should be +0.50 -1.00x160.
 |
|
Fig. 5. A well fit bitoric GP on a toric cornea will have an alignment fluorescein pattern comparable to a spherical GP. Click image to enlarge. |
Similar to soft toric CLs, the axis of the toric haptics should always rotate into the same position, just like the toric marking of a soft lens after using LARS to compensate for lens rotation.
Final CL Rx:
OD 8.6/14.5/-4.50-2.25x180 20/25+2
OS 8.05/16.0/PL -1.00x160/4.65 sag/+150 x -150 limbal clearance/flat 11 x steep 10 20/40+2
Case #7: The Astigmat with Spectacle Blur
A new patient, a 53-year-old female, presents wearing corneal GP lenses dispensed a year ago. She complains of worse vision with glasses after removing her lenses. She also feels her acuity with monovision spherical GPs is not as good as it was in the past. Despite wearing her driving glasses over her CLs to enhance her distance vision, she still experiences halos and glare driving at night.
Entering VAs (CLs):
OD 20/25 (fuzzy), J12
OS 20/200, J1
Over-refraction:
OD Plano 20/25
OS -2.00 -0.50x170 20/25
Topography taken over the contact lenses was spherical OD but revealed 0.48D of cylinder OS. Contact lens verification revealed a single base curve and power with no warpage. Refraction and topography were performed after lens removal.
Refraction: OD -3.00 -1.50x010 add +2.50
20/25, J1
OS -5.25 -2.50x175 add +2.50
20/25, J1
Topography Sim Ks:
OD 46.90@94/45.48@4 1+ distortion
OS 47.76@94/45.05@7 1+ distortion
The corneal topography was consistent with corneal warpage from a high-riding GP lens (Figure 3). In addition, the cylinder found on over-refraction and topography measurements taken over the left GP indicated the presence of lens flexure.
A one-week CL holiday was advised after which the patient returned for new measurements. Upon follow-up, an increase in both refractive and corneal astigmatism resulted in improved BCVA and corneal irregularity (Figure 4).
Refraction:
OD -2.50 -2.75x015 add +2.50 20/20, J1+
OS -4.00 -3.00x165 add +2.50 20/20, J1+
Topography Sim Ks :
OD 47.41@70/45.11@160 MCAR
OS 47.83@94/45.04@004 MCAR
The patient can be refit into bitoric GPs to improve centration and overall vision, including night driving (Figure 5). In this case, the superior lens decentration affected her corneal shape, manifesting as decreased vision quality and spectacle blur.
The position of a GP lens plays an important role in inducing corneal warpage, with a high-riding GP lens producing flattening superiorly and steepening inferiorly.²¹ The left eye also had RA due to the spherical GP bending or “flexing” due to the high-riding position and the suboptimal fitting relationship of the spherical GP on a toric cornea.
Refitting this patient into a back-surface toric lens that more closely matched the corneal shape improved centration and comfort, eliminated lens flexure (resulting in less flare and no spectacle blur) and improved VA both with the lens on and post-removal. Other common options for addressing flexure include increasing lens thickness or using a stiffer material. The most comprehensive solution to correct both corneal warpage and lens flexure is to fit a GP with a toric back surface when indicated.
 |
| Fig. 6. This front toric GP shows no rotation with the marking located at 6:00. Click image to enlarge. |
Case #8: The Post-Cataract Astigmat with a Toric IOL Implant
A 65-year-old female presents for contact lens fitting after having cataract surgery OU. She was previously a highly myopic astigmat and now wears corneal GPs for 15 to 20 hours a week for distance correction and will wear readers over. She finds GPs to be uncomfortable and is eager to remove them after just a few hours. She previously elected to be corrected for near during cataract surgery and had a toric IOL implanted in her OD and a monofocal IOL with limbal relaxing incisions in her left eye.
Refraction: OD -2.75 -0.75x160 add +2.50
20/20, J1+
OS -2.00 -1.50x165 add +2.50
20/20, J1+
Topography Sim Ks:
OD 46.48@98/44.30@008 2.18D WTRA
OS 46.20@82/46.68@172 1.52D WTRA
A soft toric CL makes the most sense, given the patient’s goal of part-time wear, desire for better comfort and self-reported history of GP intolerance with modest refractive astigmatism. But due to her familiarity with corneal GPs, the patient was unwilling to try a soft lens. Ordinarily, with the refractive cyl being less than or equal to the corneal cyl and ≤2.50D, this patient would’ve been a good corneal GP candidate; however, the refractive and corneal cylinder no longer match due to internal astigmatism created by the toric IOL. The only option available to adequately correct her vision and meet her needs would be a front-toric GP OD, while the OS is a perfect candidate for a spherical GP.
Although GPs can be designed empirically, it’s difficult to know just how much RA from the toric IOL exists without a series of complex calculations vertexing the IOL to the corneal plane. Two possible clinical approaches are to: (1) empirically order a spherical GP based on the Ks and refraction, perform a sphero-cylindrical over-refraction once the lens arrives and reorder the lens with the correct amount and location of toricity, or (2) apply a diagnostic spherical GP and over-refract before ordering.
The patient was informed that she will notice that the right lens “feels” different than her left and that the vision in her right eye may fluctuate with blinking due to the rotational forces generated by her eyelids when blinking. She was also reminded she could reconsider a soft lens if symptoms aren’t able to be minimized.
Taking time to discuss appropriate expectations assists in building a better doctor-patient relationship. Patients will have more awareness with front-toric GPs in the beginning because the majority incorporate a prism ballast design for stabilization. This adds weight to the lens and can cause some decentration. Typically, 0.75D prism to 1D is recommended for moderate to high minus lenses and 1.25D to 1.5D for low minus and plus lenses.²²
The patient did notice some initial awareness differences, which resolved within a week. As expected, the initial right lens did exhibit some rotation but was stable and had a SCOR. By using the same guidelines for soft lenses, the power was adjusted using a cross-cylinder calculator. The patient successfully achieved stable 20/20 vision.
When ordering a front toric GP, it’s important that you request the base of the prism be marked to help evaluate the fit (Figure 6). Occasionally, a patient’s lid forces and anatomy may result in rotational instability even with an adequate amount of prism ballasting. In these cases, prescribing a truncated design can help. When all else fails, if the patient has tight lids or a forceful blink, prescribing a pair of glasses over the CLs is another alternative and works especially well for presbyopes, who can incorporate it as a progressive or bifocal for optimal correction at all distances.
Final CL Rx:
OD 7.60/9.2/-2.00-1.50x110/1.5D prism 20/20
OS 7.50/9.2/-2.75D 20/20
Takeaways
There really has never been a better time to be a contact lens wearer who has astigmatism. As clinicians, we have so many options to choose from; it would be a shame not to give our patients the crispest vision possible. Keys to success include listening to the patient, assessing their visual needs and lifestyle and carefully comparing the refractive and corneal astigmatism. Considering all of these factors will help in devising an individualized solution that best address the patient’s contact lens needs. Keep in mind that the common 0.75D cut-off of residual astigmatism isn’t a hard and fast rule.
Dr. Andrzejewski works at Chicago Cornea Consultants with special areas of interest in the management of dry eye, keratoconus and other cornea and contact lens–related issues, as well as scleral contact lenses. She also is an adjunct clinical faculty member of the Illinois College of Optometry and the Chicago College of Optometry. She is a key opinion leader for Synergeyes and on the speakers bureau for Bausch + Lomb Specialty Vision Products.
Dr. Malooley is director of optometric services at Chicago Cornea Consultants. She is a Diplomate in the CCLRT section of the American Academy of Optometry with professional focus on specialty contact lenses for keratoconus, irregular cornea and prosthetic patients. She is adjunct faculty at both the Illinois College of Optometry and Chicago College of Optometry. She has no financial interests to disclose.
1. Nichols J, Fisher D. Contact lenses. Cont Lens Spectrum. 2020;36(1): 24-9; 51. 2. Young G, Sulley A, Hunt C. Prevalence of astigmatism in relation to soft contact lens fitting. Eye Contact Lens. 2011;37(1):20-5. 3. Stephanie MC, Berntsen DA, Bickle KM, et al. Efficacy of toric contact lenses in fitting and patient-reported outcomes in contact lens wearers, Eye and Contact Lens. 2018;44:S296-9. 4. Morgan P, Efron S, Efron N, Hill E. Inefficacy of aspheric soft contact lenses for the correction of low levels of astigmatism. Optom Vision Sci. 2005;82(9): 823-8. 5. Dabkowski JA, Roach MP, Begley CG. Soft toric vs. spherical contact lenses in myopes with low astigmatism. Int Contact Lens Clin. 1992;19(11):252-6. 6. Richdale K, Berntsen D, Mack C, Merchea M, Barr J. Visual acuity with spherical and toric soft contact lenses in low- to moderate astigmatic eyes, Optom Vision Sci. 2007; 84(10): 969-75. 7. Momeni-Moghaddam H, Naroo SA, Askarizadeh F, Tahmasebi F. Comparison of fitting stability of the different soft toric contact lenses. Cont Lens Anterior Eye. 2014;37(5):346-50. 8. Myers RI, Jones DH, Meinell P. Using overrefraction for problem solving in soft toric fitting. Cont Lens Anterior Eye. 1990;17(9):232-5. 9. Caroline PJ, André MP. The effect of corneal diameter on soft lens fitting, part 1. Cont Lens Spectrum. 2002;17(4):56. 10. Young, Graeme. Ocular sagittal height and soft contact lens fit. J Br Cont Lens Assoc. 1992;15(1): 45-9. 11. Davis R, Becherer D. Techniques for improved soft lens fitting. Cont Lens Spectrum. 2005;20(8). Available at: www.clspectrum.com/issues/2005/august-2005/techniques-for-improved-soft-lens-fitting. Accessed June 5, 2021. 12. Rute J. Macedo-de-Araújo, Eef van der Worp, José M. González-Méijome. A one-year prospective study on scleral lens wear success. Contact Lens Ant Eye. 2020; 43(6): 553-61. 13. Abou Samra WA, El-Emam DS, Kasem MA. Clinical performance of a spherical hybrid lens design in high regular astigmatism. Eye Contact Lens. 2018;44(9):S66-S70. 14. Lipson M, Musch D. Synergeyes versus soft toric lenses: vision-related quality of life. Optom Vis Sci. 2007; 84 (7): 593-7. 15. Bennett E, Et Al. Effect of patient personality profile and verbal presentation on successful rigid contact lens adaptation, satisfaction and compliance: Optom Vis Sci. 1998;75(7):500-505. 16. Sindt CW. Tangible Hydra-PEG: A novel custom contact lens coating technology designed to improve patient comfort and satisfaction. Whitepaper.[Google Scholar]. 2016. 17. Michaud L, Barriault C, Dionne A, Karwatsky P. Empirical fitting of soft or rigid gas-permeable contact lenses for the correction of moderate to severe refractive astigmatism: a comparative study. J Am Optom Assoc. 2009;80(7):375-83. 18. DeNaeyer G, Sanders D, van der Worp E, et al. Qualitative assessment of scleral shape patterns using a new wide field ocular surface elevation topographer. J Contact Lens Res Sci. 2017;1(1):12-22. 19. Macedo-de-Araújo RJ, Amorim-de-Sousa A, Queiros A, et al. Relationship of placido corneal topography data with scleral lens fitting parameters. Cont Lens Ant Eye. 2019;42(2):20-27. 20. Consejo A, Rozema JJ. Scleral shape and its correlations with corneal astigmatism. Cornea. 2018;37(8):1047-52. 21. Wilson SE, Lin DT, Klyce SD, et al. Rigid contact lens decentration: a risk factor for corneal warpage. CLAO J. 1990;16:177-82. 22. Borish IM. Vision correction with contact lenses. Clinical Refraction. 3rd ed. Chicago: Professional Press: 1970:971-1005. |

