 |
Q:
A 32-year-old mother of three came in for a routine exam with no complaints. Vision was 20/20, but confrontation fields were dramatically constricted. The fundus exam confirmed retinitis pigmentosa (RP). How do I deliver the news, and what are the next steps?
A:
“Breaking this news to patients is often more of a challenge than reaching the proper diagnosis,” says Chelsea Miller, OD, of Athens Family Vision Clinic in Athens, GA. In many RP patients there is a known history, and family members have a clear understanding of the condition and its inheritance pattern. However, in a patient like ours, who presented for a routine eye exam, this conversation can be a lot more difficult.
After discussing a potentially devastating diagnosis like RP with a patient, Dr. Miller believes ongoing support is important. They will have more questions after they do their own research. “In my experience, let the patient know that you are available to answer any further questions via phone, email or future appointments,” she recommends. “Patients who know their eye care provider is reliable and accessible will be very appreciative.”
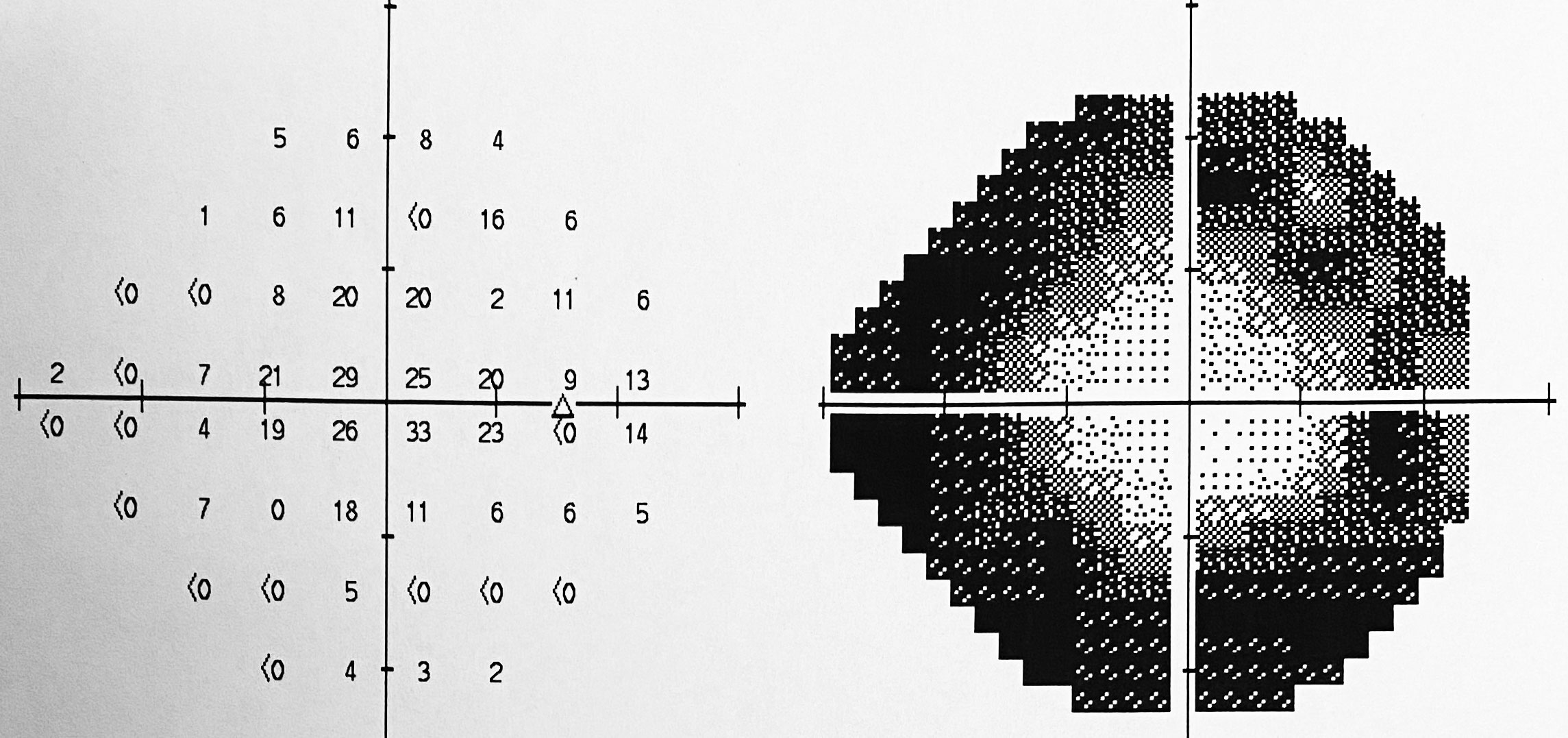 |
| Fig. 1. VF reveals peripheral vision loss. Click image to enlarge. |
RP Refresher
Retinitis pigmentosa is a progressive condition that causes retinal degeneration at the photoreceptor level. It affects rods initially and more severely than cones. Vision loss will begin in the periphery and gradually progress into the central vision, where rods are less dense. Because rods are more affected, complaints of difficulty seeing in dim/dark lighting are common. In its end stages, RP can also causes a loss of cones and affect central vision and best-corrected visual acuity. The inheritance pattern can be autosomal dominant (30% to 40%), autosomal recessive (50% to 60%) or X-linked recessive (5% to 15%). RP can also be associated with Leber’s congenital amaurosis and Usher syndrome.1
A thorough, dilated retinal examination can determine if there is any alteration in pigmentation and also detect the presence of bone spicules, a common finding in RP patients. Considering the degree of field
loss (Figure 1), there were few bone spicules noted in this case (Figure 2).
Comanaging with a retina specialist is not always necessary. However, documenting the degree of vision and visual field loss as a baseline is critical to monitor progression. Fundus photos, visual field testing and electrodiagnostic testing if available are other essential components of diagnosis, according to Dr. Miller.
Electroretinograms (ERGs) measure the electrical response of the photoreceptors and can help detect early disease as well as distinguish between retinal disease and optic nerve disease. The multifocal ERG can measure responses in the fovea, which is more beneficial in later stages of RP.
 |
| Fig. 2. Bone spicules are a common finding of most RP patients. Click image to enlarge. |
Testing Responsibilities
Referring a patient and their family members for genetic testing is important. “The genetics of RP can vary, and testing by a trained counselor may offer information in terms of inheritance patterns and gene mutations as well as a prognosis,” Dr. Miller says.
There are risks and benefits to predicting the future of RP in asymptomatic family members without clinical signs—either a false sense of security that they will never get it or a lifetime of fear that they will. One pro to genetic testing in children of RP patients is that it may qualify them for clinical trials. Gene therapy research for certain types of RP is currently underway, giving hope to patients in the future.2
In this specific case, genetic testing was performed using the patient’s saliva, which confirmed RP and will also help determine the risk factors for her children.
Dr. Ajamian is the center director of Omni Eye Services of Atlanta. He currently serves as general chairman of the education committee for SECO International. He has no financial interests to disclose.
| 1. Natarajan S. Retinitis pigmentosa: a brief overview. Indian J Ophthalmol. 2011;59(5):343-6. 2. Huang H, Chen Y, Chen H, et al. Systematic evaluation of a targeted gene capture sequencing panel for molecular diagnosis of retinitis pigmentosa. PLoS One. 2018;13(4):e0185237. |

