Face mask wear has become a norm since the onset of the pandemic in 2020 and is often considered a first line of protection against the spread of COVID-19. While masks have now been integrated into many daily routines—from logging eight-hour days at the office to quick trips to the grocery store—eyecare practitioners are seeing a notable rise in dry eye disease (DED) and other ocular surface disease (OSD) issues they attribute to improper mask wear, and possibly even extended mask wear.
Overall, poorly worn masks can cause significant problems for the ocular surface and may even affect lower lid motility, alter blink rate and blink efficacy to add a different dimension to what has been offered as causes for ocular surface disease, says Joseph Shovlin, OD, of Scranton, PA. “When patients come into the office, they sometimes have the upper portion of their mask close to or even riding above their lower lid,” he says.
These mask-induced OSD issues that doctors are seeing in their chairs are mirrored in the literature. A recent study that looked at the effects of daily face mask wear on the ocular surface found that improper use may lead to increased ocular irritation and DED symptoms.1 Additionally, a case report published in Eye & Contact Lens found a heightened number of DED symptoms in regular mask-wearing patients with no previous history of ocular surface issues.2
“When there isn’t an appropriate seal between the skin and the mask, it creates an artificially challenging microenvironment on the surface of the eye,” explains Mile Brujic, OD, of Bowling Green, OH.
The challenge here is twofold: the inappropriate mask seal causes additional airflow that is directed toward the eyes, and it increases microbe exposure to the ocular surface. “With this in mind, it’s incumbent on eyecare practitioners to educate patients on appropriate mask wear and provide them with the best treatments for what is now commonly referred to as ‘mask-induced dry eye’,” Dr. Brujic says.An Uptick in Symptoms
Mask wear has become the tipping point for DED development in many previously healthy patients, while it has worsened symptoms in others who already had the condition, says Kambiz Silani, OD, chief clinical director of Beverly Hills Optometry and founder of its Advanced Dry Eye Center in Beverly Hills, CA. “In the latter group, some individuals are having a hard time with productivity at work, while others have debilitating symptoms that make them unable to drive or cause them to rely on sunglasses to help with sensitivity,” he says.However, the disruption of the ocular surface caused by mask wear doesn’t appear to be limited to just dry eye alone, as DED has been linked to blepharitis and the development of chalazion.3
A team of Australian researchers found improper face mask wear led to inadvertent corneal abrasions and subsequent, recurrent corneal erosion syndrome and infections.2
Lid margin diseases, such as hordeola, chalazia and blepharitis, are the most prevalent mask-related OS conditions seen by optometrist Paul Karpecki, chief medical director for Keplr Vision and the Dry Eye Institutes of Kentucky and Indiana. Additionally, Dr. Karpecki is treating more individuals with a history of recurrent corneal erosion—who had previous well controlled conditions—only to have them resurface due to mask wear.
“We are seeing ocular surface issues well beyond dry eye,” he says.
During the early days of the pandemic, Dr. Shovlin noticed an alarming increase in patients with chalazia with both upper and lower lid involvement, which he says reflects what is being reported in the literature.4
“I would estimate a two-to-three times increased rate of chalazion over years prior to COVID-19 mask wear, along with an increase in patients with dryness symptoms,” he says.
Dr. Brujic cites an upward trend of patients presenting with internal and external hordeolum caused by mask wear. In addition to styes, optometrist Scott Hauswirth, assistant professor at the University of Colorado School of Medicine, is also encountering more cases of blepharitis, which he attributes to improper mask wear.
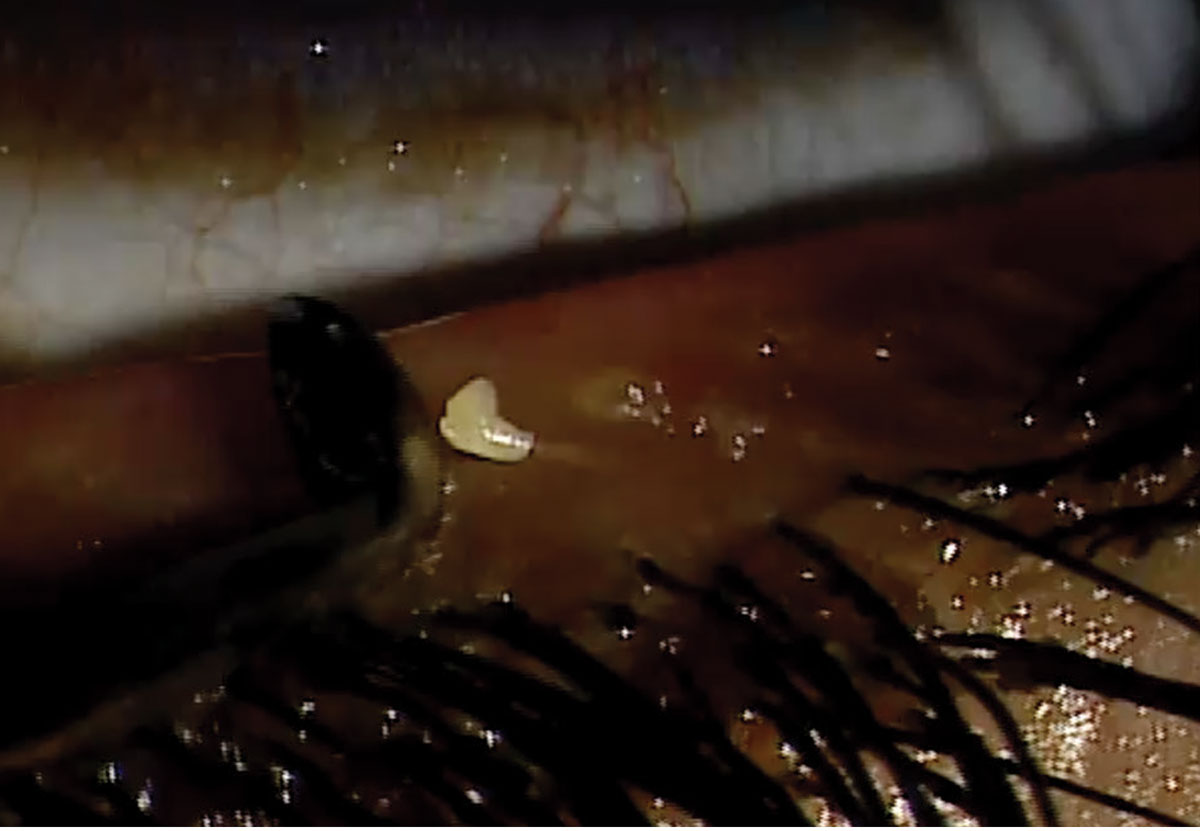 |
Debriding clogged meibomian gland. Photo: Mile Brujic, OD. Click image to enlarge. |
The Bacteria Funnel
Looking at the mechanism behind why the ocular surface is altered, experts say it essentially comes down to too much air being directed into the eyes over an extended period and bacteria infiltrating the OS.
Specifically, poor face mask fits result in increased airflow over the ocular surface, which in turn increases the evaporation of the tear film and compromises its protective barrier, resulting in dry eyes.2 In individuals who already have a compromised epithelial surface, this can increase their susceptibility to infection.2
Additionally, the ocular surface becomes dryer due to the accelerated evaporation, and patients are touching their faces more often, Dr. Shovlin explains. Some researchers have even proposed a conduction theory whereby there may be a “funnel” of bacteria that is aimed directly at the lid area, he adds.
“Ocular flora may be altered significantly, according to a few investigators,” Dr. Shovlin says. “This in turn affects the ocular surface in several ways, resulting in blepharitis and meibomian secretion ‘hardening’.”
In addition, oral flora is easily incorporated into expired droplets for transmission to the eye, he adds.
Dr. Brujic likens the mechanism to being in a room where you have a non-stop breeze blowing in your eyes.
“Your breath is constantly being re-directed towards the eyes, which aren’t equipped to receive that much air over an extended period of time,” Dr. Brujic says.
In addition to bacterial infiltration, Dr. Karpecki cites another reason for OSD-related issues caused by mask wear: the desiccation of the ocular surface, which he says is a similar process to what can happen to the eye during continuous positive airway pressure (CPAP) overnight treatments.
“It’s similar to wearing a mask all day, since there is continuous airflow that is causing many of the same issues, like blepharitis and dry eye. Though the air isn’t bacteria-filled, CPAPs can cause desiccating stress or desiccation of the cornea, and meibomian glands don’t get to recover when they are supposed to during that downtime,” he says.
Testing Offers Clues
While some patients have DED or other ocular surface problems independent of mask wear, a few telltale signs during the exam may tip off clinicians to a mask-related OSD problem.
A study in Cornea found patients with moderate-to-severe dry eye had a decrease in their tear film stability based on lower tear break-up time (TBUT) readings after mask wear.5 In the investigation, participants’ first noninvasive TBUT reading with a face mask was 6.2 seconds, which increased to 7.8 seconds without one—a difference of 1.6 seconds.5 The average noninvasive TBUT measurement with a face mask was 12.3 seconds and increased to 13.8 seconds without the use of a mask—a difference of 1.5 seconds.5
Another investigation found long-term use of face masks not only shortened TBUT time but also reduced Schirmer-1 measurements.1 The research paper cited a significant increase in OSDI scores and ocular surface staining according to the Oxford scale after eight hours of continuous face mask use.1 Furthermore, it was observed that taping down the open upper portion of the mask improved test parameters by preventing exhaled dry air from contacting the eyes.1
Dr. Hauswirth says he’s more frequently noticing younger patients with no history of dry eye complaining of symptoms, and often these individuals don’t have corneal staining.
“It’s very situational and is a reminder that taking a careful history is important in helping with the diagnosis,” says Dr. Hauswirth, who will be launching an upcoming NEI-NIH funded investigation on mask wear related OS issues in a group of healthcare workers.
During the exam, Dr. Silani checks the patient’s meibomian glands using meibography, evaluates tear film consistency, quality and stability, in addition to performing staining such as lissamine green or fluorescein. Practitioners can check for staining of the cornea and conjunctivae, looking for lid wiper epitheliopathy, punctate epithelial defects, superficial punctate keratitis and how quickly the tear film is evaporating. Additionally, meibography images can tell a big picture story about the structure and function of the glands, he says.
“We know that 86% of patients have dry eye because their glands structurally aren’t there, healthy or functioning properly,” Dr. Silani says.6
Dr. Silani also uses the Oculus Keratograph 5M to examine the meibomian glands, provide non-invasive tear film break-up time readings and tear meniscus height measurements, in addition to an evaluation of the lipid layer.
Dr. Karpecki is seeing more patients with inadequate lid closures with these mask-related OSD issues. This condition should not be confused with lagophthalmos, the inability to close the eyelids, he suggests.
In order to determine if lid seal issues are causing the problem, Dr. Karpecki recommends the Korb-Blackie light test. Any light escaping from the lid margin will become evident, indicating incomplete or inadequate lid seal, he says.
If a patient comes into the office and complains of a third consecutive stye in a month, Dr. Karpecki will always check the lid seal and usually will find this is the source of the problem.
Regarding fluorescein staining, Dr. Karpecki recommends looking for dryness in the lower part of the cornea and conjunctivae, which tend to show linear staining patterns in these patients.
 |
Rethink Treatment Protocols
Although the eye conditions are familiar, you may want to rethink your typical treatment protocol when addressing mask wear–related ocular surface problems, experts suggest.
In these cases, Dr. Brujic first assures that the lid margin is absent of any inflammation or blepharitis, and that InflammaDry (Quidel) testing is negative prior to punctal occlusion.
Patients predisposed to blepharitis should be reminded about the importance of lid hygiene, he says.
Additionally, mask wear has caused some patients to switch to contact lenses to avoid foggy glasses. In these cases, prescribe the best contact lens technologies possible, Dr. Brujic says.
Of course, treatments also depend on patient demographics, Dr. Hauswirth adds. At his practice, many of the patients with dry eye are not contact lens wearers, tend to be older and many have autoimmune disorders. Based on these factors, Dr. Hauswirth frequently prescribes anti-inflammatory treatments and serum tears, and has noticed an increase in his use of antibiotics due to more cases of blepharitis and hordeola since the start of the pandemic.
If mask-related DED is detected during the exam, Dr. Silani will customize a treatment plan for the patient. This could include home remedies, such as warm compresses and eyelid hygiene and a high quality, science-based omega-3 supplement. He may also recommend lipid-based lubricating drops for evaporative dry eye cases. Depending on the patient’s condition, he may also suggest in-office treatments such as intense pulsed light (IPL) therapy, thermal expression treatments and microblepharoexfoliation.
A recent case report published in the American Journal of Ophthalmology found an increased incidence of chalazion with mask use.4 The authors suggest a multi-pronged preventative approach:
• a commercially approved antiseptic mouthwash containing hydrogen peroxide, alcohol or povidone iodine to reduce bacterial load and decrease the likelihood of masked breathing patterns altering the normal flora of the eyelids and periorbital region
• frequent hot water washing of cloth face masks
• good hand hygiene practices; avoidance of face touching and excessive mask adjustment
• the use of adhesive tape over a mask on the bridge of the nose to minimize the upward direction of air towards the eyes.4
Additionally, the authors suggest the use of a 1% hypochlorous acid solution eyelid scrub as part of daily eyelid hygiene to act as both an antiviral and antibacterial blepharitis deterrent.4
Due to airflow and inadequate lid closure issues, Dr. Karpecki is recommending thicker lubricating agents for these patients. “I’m more likely to use a gel that has some staying power and will stay on the eye instead of going away more quickly,” Dr. Karpecki says.
In addition to thicker tear ointments, Dr. Karpecki points to a new product he helped developed that will be coming soon for those individuals with lid seal problems: SleepTite (Ophthalmic Resources Partners), which is a single-use device intended to hold the eye closed to prevent it from unintended exposure to fluids, airborne contaminants or excessive drying due to incomplete lid closure.
Dr. Karpecki is also finding many patients do well with hydrating compresses, especially if they are getting hordeolum, and he’s turning to in-office procedures such as blepharoexfoliation, IPL, low level light therapy and in-office thermal expression.
“It seems many of these patients are having a lot more issues with their eyelid margins drying and accumulating keratin plugs or biofilm. For example, I’m finding that if I don’t do a quick lid debridement, the patients tend not to get a good response, and they may get multiple hordeola otherwise,” he says.
Patient Education is Key
In addition to reaching for your Rx pad, patient education on proper mask wear can also help mitigate OSD issues. In choosing a mask, the CDC recommends that it has two or more layers of washable, breathable fabric, completely covers the nose and mouth, fits snugly against the sides of the face and doesn’t have gaps and also is equipped with a nose wire to prevent air from leaking out of the top.7 Reusable masks should be washed as soon as they become dirty, or at least once a day.7 If you have a disposable face mask, throw it away after wearing it once, the CDC advises.7
Dr. Silani suggests asking patients how long they wear masks throughout the day, as prolonged use can contribute to mask associated dry eye or styes.
“We recommend that patients remove their masks when they are able or alone, to make sure the mask top half is pinned down correctly to minimize upward airflow and to tape down the top half of the mask if the individual is noticing their glasses are fogging up,” he says.
Additionally, some patients are bringing up their masks too high and limiting their lower eyelid from fully making contact with the upper eyelid, so placement or positioning of the mask is important, Dr. Silani adds.
“If a patient is complaining of mask-related dry eye, consider suggesting different mask options—specifically ones that have a reinforced barrier across the bridge of the nose and across the upper cheek that allow for an air-tight fit,” Dr. Hauswirth says.
Researchers from Wills Eye Hospital who looked into bacterial dispersion with patient face mask use during simulated intravitreal injections found alterations of bacterial dispersion around the eye during treatment based on the type of mask worn.10 The authors noted significantly more bacterial dispersion when wearing a tight-fitting face mask without tape vs. a tight-fitting one with tape. Additionally, their study found no difference in bacterial dispersion between tight-fitting surgical masks with tape and N95 masks.8
In addition to recommending patients tape their mask on the bridge of the nose to minimize an upward draft toward the eye and take care not to affect the normal blink dynamics or eyelid closure, Dr. Shovlin also suggests reminding the patient to avoid touching their face or adjusting their mask as much as possible.
Patients with pre-existing DED and other ocular surfaces issues such as recurrent corneal erosion syndrome may need additional care with proper mask fitting.2
Despite the OSD issues occurring, mask wear is a necessity for health and safety, Dr. Silani adds.
“We are very pro-health and safety. Yes, mask-associated dry eye does exist, and taking steps to avoid and treat it is important. But doctors should recommend patients wear masks to protect themselves and others. Patients should tape down the top of their masks, and when they aren’t around people or in a safe place, they can take it off or use lubricating drops at work if they can’t remove their mask,” Dr. Silani says.
Another recent study found most individuals didn’t experience a change in ocular symptoms, but a significant portion still reported an increase in ocular discomfort while wearing a mask.9 The investigation suggests not to underestimate all the symptoms that could discourage the population from using masks, and that ODs should verify the presence of clinical signs in those complaining about mask-induced eye discomfort and recommend ways to mitigate these issues.
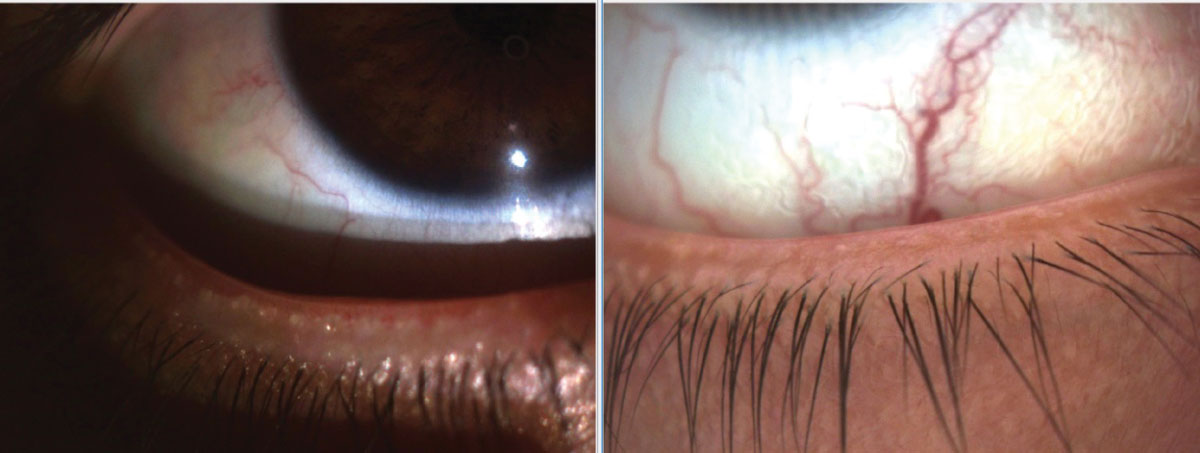 |
Lid margin integrity and meibum function improving due to office-based treatments in a 27-year-old female patient with DED secondary to MGD. She works in a healthcare facility and prolonged face mask wear has exacerbated her dry eye condition. Photo: Kambiz Silani, OD. Click image to enlarge. |
Mask-related OSD Trends
Normally, one would expect that people who work at jobs that involve heavy computer use would have more mask-related OSD issues, but Dr. Brujic says he’s not seeing this occurring. “At the beginning of the pandemic, a majority of these people were working from home and didn’t have to wear a mask,” he explains.
On the other hand, Dr. Brujic was treating more OSD cases in individuals who worked at venues that required staff in masks to be on site in stores, plants and factories.
As far as age posing a potential risk factor, Dr. Hauswirth says most of his symptomatic patients over the last year-and-a-half are younger, healthy individuals who never had ocular surface issues before, despite the fact they are computer users. “We are seeing a lot of people naïve to the disorder, who weren’t really dry eye patients beforehand,” Dr. Hauswirth says.
“Other patients with existing issues, such as rosacea and blepharitis, are also increasingly presenting with OSD issues due to mask wear,” Dr. Karpecki says. Additionally, he is noticing an uptick in contact lens-wearing patients with mask-related complications.
Even before the pandemic, the Tear Film & Ocular Surface Society (TFOS) had already reported that discomfort while wearing contact lenses were associated with a reduction in the compatibility between CLs and the ocular environment.10
Exploring the impact of contact lenses and mask wear, a team of researchers from Portugal found mask use increased dry eye symptoms in contact lens wearers and negatively impacted their visual quality.11 Additionally, lens wear significantly decreased after the onset of COVID, and the sensation of dry eye was found to be worse in those using monthly replacement contact lenses.11
Looking Ahead
With face mask use likely extending into at least the near future, eye dryness, irritation and keratopathy from mask wear may become a problem for a large percentage of the population.14 If present, this mask-associated ocular irritation raises concerns about eye health and increased risk of disease transmission with prolonged wear.12
Considering this forecast, additional investigations may be warranted. One consideration for future studies could be an analysis of geographical differences from one region to another and a comparison of ocular surface prevalence issues in areas that are more compliant in mask-wearing practices or in areas with higher rates of COVID-19, Dr. Shovlin suggests.
Along with mask-induced dry eye, Dr. Silani also stresses that it is important to consider potential comorbidities, such as lagophthalmos, ocular allergies and anterior blepharitis, as multiple, contributing factors could be at play.
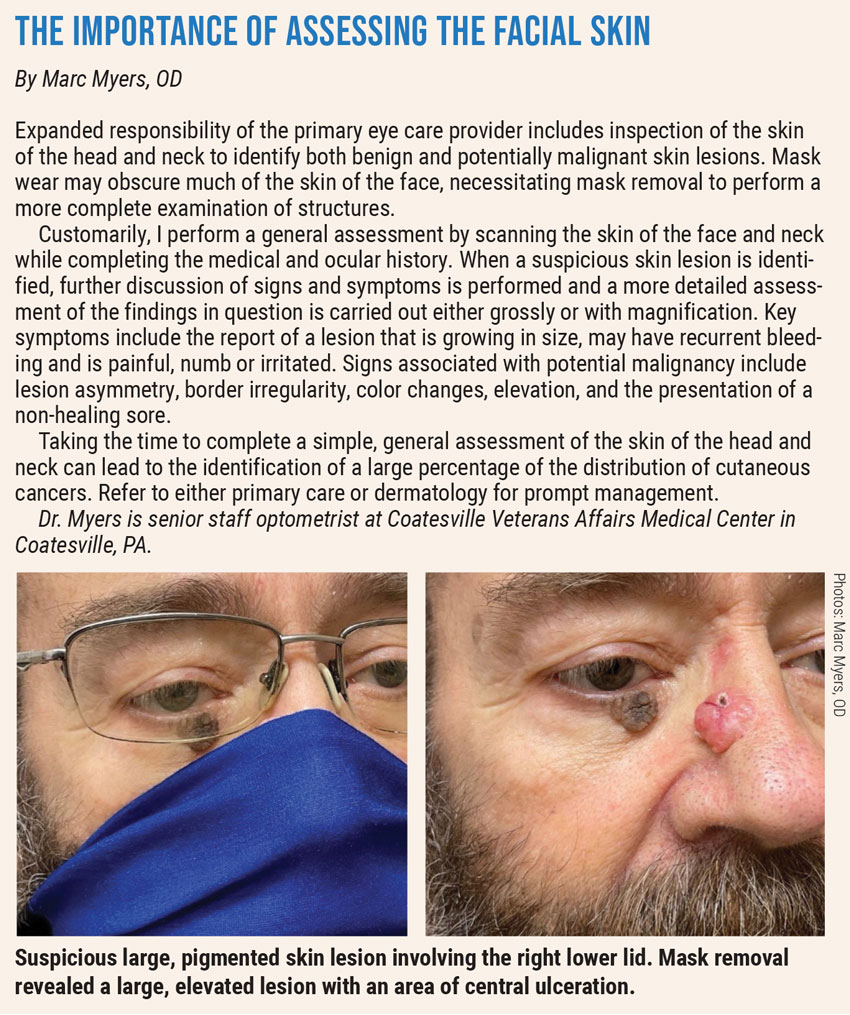
Another point to consider: look for any suspicious lesions under the mask that may warrant testing, experts advise.
“Masks are here to stay,” Dr. Brujic says. “We don’t know what the capacity of masks are going to be, but they’ll be part of our society. Today, it’s not uncommon to see people in masks, but it’s important for optometrists to be asking about it. We see the patient for 15 minutes in our office, but we need to know how much or how little they’re wearing their masks outside of the office and provide them appropriate solutions.”
1. Aksoy M, Simsek M. Evaluation of ocular surface and dry eye symptoms in face mask users. Eye Contact Lens. 2021;47(10):555-8. 2. Tang YF, Chong EWT. Face mask–associated recurrent corneal erosion syndrome and corneal infection. Eye Contact Lens. 2021;47(10):573-4. 3. Nemet AY, Vinker S, Kaiserman I. Associated morbidity of chalazia. Cornea. 2011;30:1376-81. 4. Silkiss RZ, Paap MK, Ugradar S. Increased incidence of chalazion associated with face mask wear during the COVID-19 pandemic. Am J Opthalmol case report. 2021 Jun;22:10103. 5. Arriola-Villalobos P, Burgos-Blasco B, Vidal-Villegas B, et al. Effect of face mask on tear film stability in eyes with moderate-to-severe dry eye disease. Cornea. 2021;40(10):1336-9. 6. Lemp MA, Crews LA, Bron AJ, Foulks GN, Sullivan BD. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea. 2012;31(5):472-478. 7. CDC. Your guide to masks. www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/about-face-coverings.html. Accessed Oct. 23, 2021. 8. Patel SM, Mahmoudzadeh R, Salabati M, et al. Bacterial dispersion associated with various patient face mask designs during simulated intravitreal injections. Am J Ophthalmol. 2021;223:178-3. 9. Boccardo L. Self-reported symptoms of mask-associated dry eye: a survey study of 3,605 people. Contact Lens Ant Eye. January 20, 2021. [Epub ahead of print]. 10. Nichols JJ, Willcox MD, Bron AJ, et al.; members of the TFOS International Workshop on Contact Lens Discomfort. The TFOS international workshop on contact lens discomfort: executive summary. Invest Ophthalmol Vis Sci. 2013;54:TFOS7-TFOS13. 11. Martinez-Perez C, Monterio B, Soares M, et al. Influence of face masks on the use of contact lenses. Int J Environ Res Public Health. 2021;18(14):7407. 12. Moshirfar M, West WB, Marx DP. Face mask-associated ocular irritation and dryness. Ophthalmol Ther. 2020;9(3):397-400. |

