 |
Fostering viable comanagement relationships requires time and effort from all parties. There must be a desire to collaborate as well as mutual trust and respect. As the primary providers of eye care, ODs are perfectly positioned to take a leadership role when working with ophthalmologic subspecialists and other medical specialists.
Effective comanagement is beneficial for a number of reasons. It gives patients easier access to care than waiting for an opening with an ophthalmologist and lessens travel and cost burdens, to name a few. From the standpoint of the surgical provider, sharing post-op responsibilities allows them to allocate more time to surgical care. For ODs, it is a way to enhance your practice and professional development.
Comanagement ConnectionsCheck out other articles in this series: The Many Layers of Cornea Comanagement Keep Glaucoma Care Close to Home |
ODs often have strong relationships with their patients developed over years or even decades of care. They not only understand their visual demands and needs, but also their personalities and what approach will work best. The specialist, on the other hand, does not have this baseline knowledge.
“They don’t know whether the patient who is noncompliant with treatment needs a little bit of tough love, or perhaps they are scared and need more of a nurturing environment,” notes Jessica Haynes, OD, of the Charles Retina Institute in Memphis. “Then on the other side, the patient walking into a specialist’s office has never seen this doctor before. They may not know what to expect, and when certain treatments are recommended, they may be distrustful of that advice,” she notes. The procedures of a retina practice—anti-VEGF injections, panretinal photocoagulation and the array of complex surgeries—all require strong buy-in from the patient for things to go smoothly. Having an existing connection with a trusted doctor can help immensely.
Optometrists must use the relationships they build with patients to walk with them through any journey of referral and treatment, Dr. Haynes emphasizes. “By building good comanagement strategies, patients will have better outcomes. And what more can a physician strive for than better care and outcomes for their patients?”
 |
|
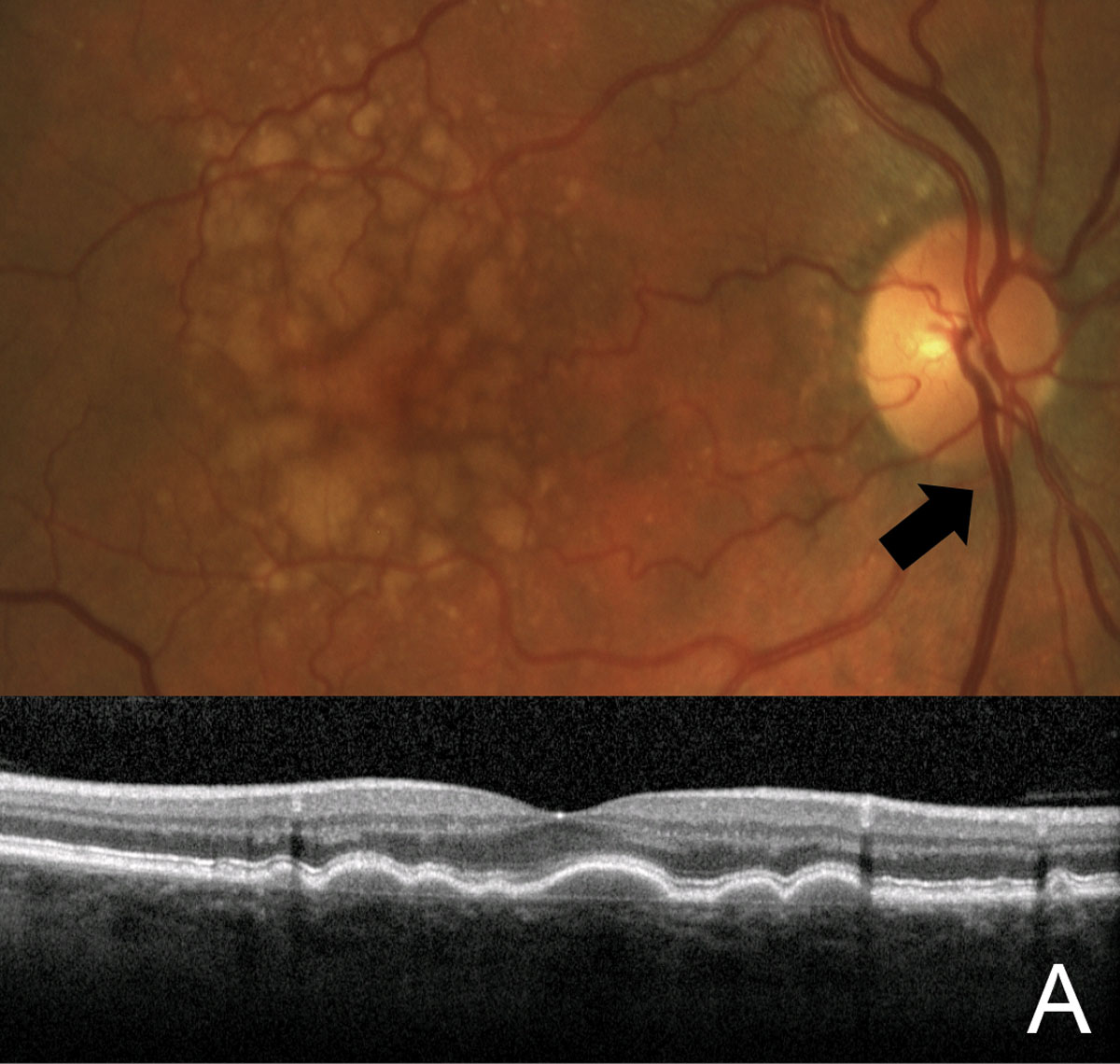
Monitoring dry AMD patients for risk factors for conversion to the wet form (such as the large, soft drusen shown here) is an ideal role for optometric skills in the continuum of retina care. Photo: Jessica Haynes, OD. Click image to enlarge. |
Building Connections
Successful comanagement requires strong relationships and open lines of communication. This begins by building connections with ophthalmologists and other specialists in your area.
“First, we have to realize that these relationships and trust have to work both ways. So, at times the ophthalmologists are the ones reaching out to develop referral relationships,” says Mohammad Rafieetary, OD, also of the Charles Retina Institute in Memphis. “Often, ODs learn who to refer to by word of mouth from other area colleagues, either through personal connections or local society meetings.”
If ophthalmologists host seminars or social events, Dr. Rafieetary encourages ODs to attend. This is an opportunity to get to know doctors and staff on both a personal and professional level.
Being proactive is key. Dr. Rafieetary also recommends optometrists take the initiative and invite specialists to events. “This is not only beneficial to establish personal relationships but create referrals for services an ophthalmologist does not offer in their practice,” he notes. “It always works better if both sides of the referral relationship know each other on a personal level.”
Spending time shadowing local providers is another way to build connections as well as learn more about their practice and how they interact with patients. “This type of approach is very likely to open up the lines of communication,” notes Dr. Haynes. “You may even get the doctor’s personal cell phone number, so the next time you have a patient who needs to be seen emergently, you don’t have to rely on their receptionist getting your patient in. You can go directly to the source.”
Inviting specialists into the optometric community can lay the foundation for comanagement. For instance, many state and local optometry chapters ask ophthalmologists to speak at their meetings. “A good turnout and discussion shows ophthalmologists our bond as a community and builds respect,” says Dr. Haynes. “So, if you aren’t active in your state and local chapters, that’s another good place to start.”
It’s also important to note that true comanagement depends on a level of respect that goes beyond education and mutual referrals. “If a retina specialist is truly respectful of the optometric level of care, they will support optometry not just in patient care but also in the political arena,” explains James Fanelli, OD, of Wilmington, NC. “A retinologist who opposes scope expansion by optometry but is happy to receive your referrals is not really a respectful referral partner.”
REFER, BUT DON'T RELINQUISH, YOUR PATIENTS• Don’t tell patients that you are referring them because you don’t have the right equipment, know-how or legal privileges. It undermines your position as a provider. • Never tell the patient you will see them “when the specialist is done with you.” Some of these patients will require ongoing care from a specialist. Such phrasing also takes you out of the chain of decision-making. Instead, communicate that you will continue to see them whenever appropriate, even if it’s just for routine eye exams and vision correction plus a “check in” on their progress with the specialist’s regimen during such a visit. • Set a follow-up appointment for patients to return to your office regardless of referral. This follow-up can always be changed if needed; however, you have a better safety net to make sure the patient is receiving appropriate treatment and more importantly is not lost to follow-up. • Make sure to follow through on the referral and all recommended follow-up with the retina specialist. |
Optimizing Retina Care
Unlike cataract and refractive surgery, there is no standard or protocol for retina comanagement; however, it is still an important aspect of successful patient care.Effective comanagement begins with the basics, notes Dr. Haynes. This includes dilating and properly examining patients as well as a comprehensive understanding of diagnostic imaging in retina care, such as OCT, and staying current on the latest treatment options.
The conversations you have with your patients before they even see a retina specialist are a crucial component of care and comanagement. ODs must feel confident in their ability to educate patients and help them through this process. And, depending on the patient, it may take multiple discussions to help them truly understand their condition and the need for a referral as well as the role of their optometrist.
As with other forms of comanagement, the optometrist should take the lead to ensure they maintain their position as the patient’s primary eye care provider. “If you believe in the importance of continuity of care, stay in control of your patient’s care,” emphasizes Dr. Rafieetary. “Schedule a follow-up appointment for your patient regardless of why you are referring them.”
Even if the condition does not require a set follow-up, scheduling another appointment perhaps three months out helps you maintain your connection with that patient. The appointment can always be adjusted if the specialist asks you to see them sooner, suggests Dr. Rafieetary.
Taking the lead also means clearly defining your role with the retina specialist. For instance, a common reason for retina comanagement is neovascular AMD. Today’s standard of care is intravitreal anti-VEGF injections.
“This is a recipe for the patient being lost to an ophthalmology retina practice,” notes Dr. Fanelli. “However, ODs can take this as an opportunity to maintain control and even determine the injection schedule.”
While you don’t know if the patient will need six monthly injections for six months or monthly injections for the rest of their life, you can schedule the patients for a series of injections, explains Dr. Fanelli. “The OD then is seeing the patient between injections, evaluating the effect of the injections using their OCT, and forwarding that info to the retina specialist prior to the next visit. By doing this, the OD stays actively involved with the management and acre of the AMD patient.”
Optometrists must stay current on the latest advancements in anti-VEGF therapies as well as how to manage and follow patients long-term. This includes recognizing potential adverse events and any other safety concerns. ODs need to be aware of what the injected eye should look like 24 hours after the injection, as well as what signs and symptoms can develop shortly thereafter that indicate, for example, early endophthalmitis.
Externally, injection sites should look relatively benign, save for the occasional subconjunctival hemorrhage, notes Dr. Fanelli. Immediately post injection, visual acuity will be reduced, but that should return to pre-injection levels within 24 to 48 hours. Decreased vision and increased discomfort are red flags for complications.
Creating a dynamic where the optometrist takes the lead goes back to finding the right ophthalmologist and fostering a relationship of mutual trust and respect. “Not only must the OD have confidence in their own skills, but the retina specialist must also believe in your abilities,” Dr. Fanelli says. “If they do, they will be comfortable following your lead and this also helps them eliminate unnecessary visits to their practice.
“There are retina specialists out there who will work with you at a level where you are the one making the determinations,” he emphasizes. “They will see your patient and say, ‘Dr. OD will let you know if you need to see me again.’ And that, I think, is the perfect, two-way referral relationship.”
REFERRAL LETTER DOS AND DON'TSA key component of any comanagement relationship is the referral letter. This an important line of communication with the specialist and helps lay the foundation for clinical management. While you want to be as specific as possible, don’t provide a diagnosis if you are unsure. “Call it as you see it,” notes Dr. Rafieetary. “Do not make up a diagnosis. ‘Retinal detachment’ is a frequently mispresented diagnosis, to justify or expedite a referral. Better to describe your findings generally than give a wrong, specific diagnosis.” The referral letter is an opportunity to clearly outline your expectations. Do you simply want the retina specialist to evaluate your patient and send them back if treatment is not indicated? Or is this something you want the specialist to monitor long-term? Let the specialist know if and when you have scheduled a follow-up with your patient. “Be specific in what you are referring a patient for and provide any necessary background information that may be needed in the form of recent patient records or a short summary,” Dr. Haynes advises. Use this letter as a tool to reiterate the comanagement relationship, suggests Dr. Chous. “Emphasize to the specialist that you want to comanage this patient and look forward to working together.” It’s also a good idea to note if specific patients are more likely to be lost-to-follow-up (LTFU) based on known risk factors like poverty, presence of other vascular comorbidities, and educational and cognitive status, so that both doctors can work to mitigate this, Dr. Chous notes. “Studies suggest that more than 25% of patients referred to retina specialists are LTFU, resulting in worse outcomes, so it’s a big deal.” |
Challenges and Gaps
Recognizing when and when not to refer to a retina specialist is an important, yet challenging, aspect of optometric practice.
One example is diabetic retinopathy. In these cases, the OD should first determine the severity. And then, no matter the stage, the optometrist must identify if diabetic macular edema (DME) is present, notes Paul Chous, OD, an expert in diabetes and diabetic eye disease from Tacoma, WA. “Retina specialists don’t need to see patients with mild, nonproliferative diabetic retinopathy without any diabetic macular edema,” he explains, noting that in those cases ODs should monitor patients for progression and counsel on the importance of individually optimized metabolic control, which is far more important in early rather than later-stage diabetic retinal disease.
As the disease progresses and moves beyond moderate severity in nonproliferative cases, the likelihood of patients developing a vision-threatening complication like proliferative diabetic retinopathy or center-involved DME increases dramatically, according to Dr. Chous. Therefore, it is critical that ODs are well-versed in the staging criteria and have the knowledge to monitor and refer these patients appropriately.
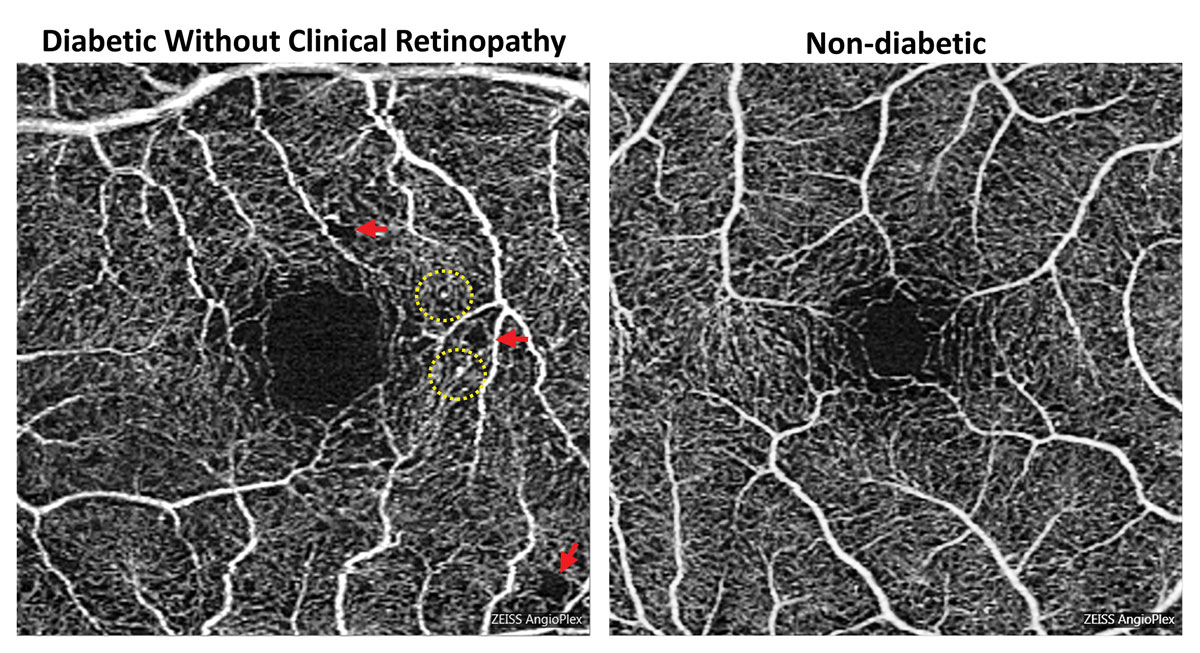
For DME, it is recommended that ODs send the patient to a retina specialist; however, Dr. Chous notes, there is a role for the optometrist, especially among patients who require observation and not immediate treatment, such as non–center involved DME or center involved DME with normal visual acuity. To make this determination and diagnose accurately, Dr. Chous says an OD must have access to an OCT.
“I would encourage every optometrist seeing patients with diabetes to have an OCT, but if they don’t, working with a nearby optometric colleague who does can be very helpful and spare patients an unnecessary visit to a retina specialist’s office,” he explains, noting this is also an opportunity to get another opinion on whether or not that patient should be referred to a specialist.
One condition that is often referred unnecessarily to ophthalmology is retinal artery occlusions. These patients, in particular those with branch retinal artery occlusions, do not need retinal surgery, Dr. Fanelli says, noting that they will need an internal medicine or vascular work-up.
In these cases, the OD can and should begin the initial workup by assessing the stroke risk of the patient (medical history, medications, carotid auscultation) and make the determination of whether the patient needs immediate referral to a stroke center or the emergency department for carotid and cerebral imaging, explains Dr. Fanelli. If the artery occlusion appears more to be related to fibrin deposits, then cardiology involvement is necessary.
This is also true for retinal vein occlusion without macular edema. Patients with retinal vein occlusions need evaluation of those etiologies that precipitate occlusion, such as poorly controlled hypertension, atherosclerosis and diabetes, or in patients without retinal vascular evidence of the above, perhaps evaluation of coagulability, notes Dr. Fanelli.
“If we’re going to market ourselves as frontline eye care providers, we can’t just cherry-pick the easy cases and manage those,” Dr. Fanelli urges. “We must create a culture of, ‘It’s OK to treat corneal ulcers on the visual axis, it’s OK to manage vein occlusion and so on, because I know what I’m doing and I’m comfortable with that.’”
Optometrists must also step up and be more forthcoming about discussing prevention. “We are the primary eye care providers and it behooves all of us in optometry to talk to our patients about preventing retinal disease,” says Dr. Chous. “We have the chance to educate our patients on the benefits of healthy lifestyle choices and encourage them to make a change.”
“From a comanaging perspective, I inform the retina specialist that I have advised the patient on lifestyle management of the retinal disease, including better diet, exercise, smoking cessation, compliance with sleep therapy and other prudent lifestyle changes,” he explains.
Here again the strength of your relationship with longstanding patients may make you uniquely well-positioned to discuss such things. An ophthalmologist with no prior relationship and level of trust with a new patient may have a harder time of it.
 |
|
Idiopathic intracranial hypertension is fairly commonly diagnosed by optometrists—and it’s incumbent on them to coordinate care, says Dr. Messner. Photo: Carolyn Majcher, OD, Susan Ly Johnson, OD. Click image to enlarge. |
Learning and Development
Effective comanagement depends not only on the relationship between providers, but also an optometrist’s understanding of retinal disease, varying clinical presentations, diagnostic imaging findings and available treatment options.
“Just because optometrists are not performing retinal surgeries, laser procedures or intravitreal injections for these conditions doesn’t give us an out to not understand the diseases and treatment options available to our patients,” Dr. Haynes notes. “A greater understanding of retinal disease is going to allow us to make better referrals.” Dr. Fanelli concurs. “Not only will it facilitate appropriate referrals, it can eliminate the need for unnecessary referrals,” he says.
Key Takeaways
• Build strong connections with specialists. • Be confident in the skills of the specialists you are referring to. • Take the lead when determining a management plan. • Constantly hone your skills and knowledge. • Communicate with patients throughout the referral process. |
As diagnostic technology becomes increasingly more able to detect early retinal disease or at least risk factors for development, the momentum in retina care is inevitably shifting toward optometry, where routine screening and monitoring visits are commonplace for many ocular conditions. Dark adaptation testing, for instance, is capable of picking up the earliest signs of AMD, which manifest at a point in the disease course when the optometrist can discuss lifestyle modifications, recommend AREDS vitamins and initiate a monitoring regimen to give patients a better shot at minimizing the disease’s effects.
With ongoing education—whether through continuing education, conferences or mentorship—ODs can hone their skills and be more equipped to recognize what requires a referral and what can be handled in their own practice. Additionally, optometrists will be able to better educate patients on their condition and what to expect from a referral visit, suggests Dr. Haynes.
“We can make a difference in the visual outcomes of these patients,” she adds. “A patient who comes into a retina clinic with a better baseline understanding of their condition from the get-go is much more likely to be compliant and have a good final outcome.”
Optometrists can and should take the lead in comanagement, using their role as primary eye care providers to drive disease management while also building strong relationships with specialists that allow them to practice to the full extent of their scope and abilities.

