 |
YAG laser capsulotomy is becoming a bigger part of optometric care as more states advance optometric scope of practice. Studies have shown, when doctors of optometry provide these procedures, they are delivering safe and effective outcomes, as well as increasing access to this valued care.1 Most cases involve a single vision intraocular lens (IOL) well-positioned within the capsular bag. This article addresses cases that involve specialty IOLs, malpositioned IOLs and atypical capsular fibrosis and contraction.
Prep
Careful evaluation of the IOL type and its position, the integrity of the lens capsule and the degree of capsular opacification is necessary before making the decision to perform a capsulotomy. These findings may influence the techniques used to perform the capsulotomy, and a meticulous evaluation prior to the capsulotomy will help ensure optimal results are achieved.
With some specialty IOLs, subtle capsular opacification will often create visual symptoms and YAG laser capsulotomy may need to be considered sooner than with single vision IOLs. Diffractive multifocal and some extended depth-of-focus (EDOF) IOLs create more reflections than single vision IOLs. These reflections may be seen by the patient as dysphotopsia but are also seen by the physician during YAG laser capsulotomy. The additional reflections can make it more difficult to visualize the posterior capsule, requiring extra caution when performing the capsulotomy to prevent IOL pits. Yellow-tinted IOLs and those that have excessive lens glistenings can also create similar difficulty in lens capsule visualization.
 |
|
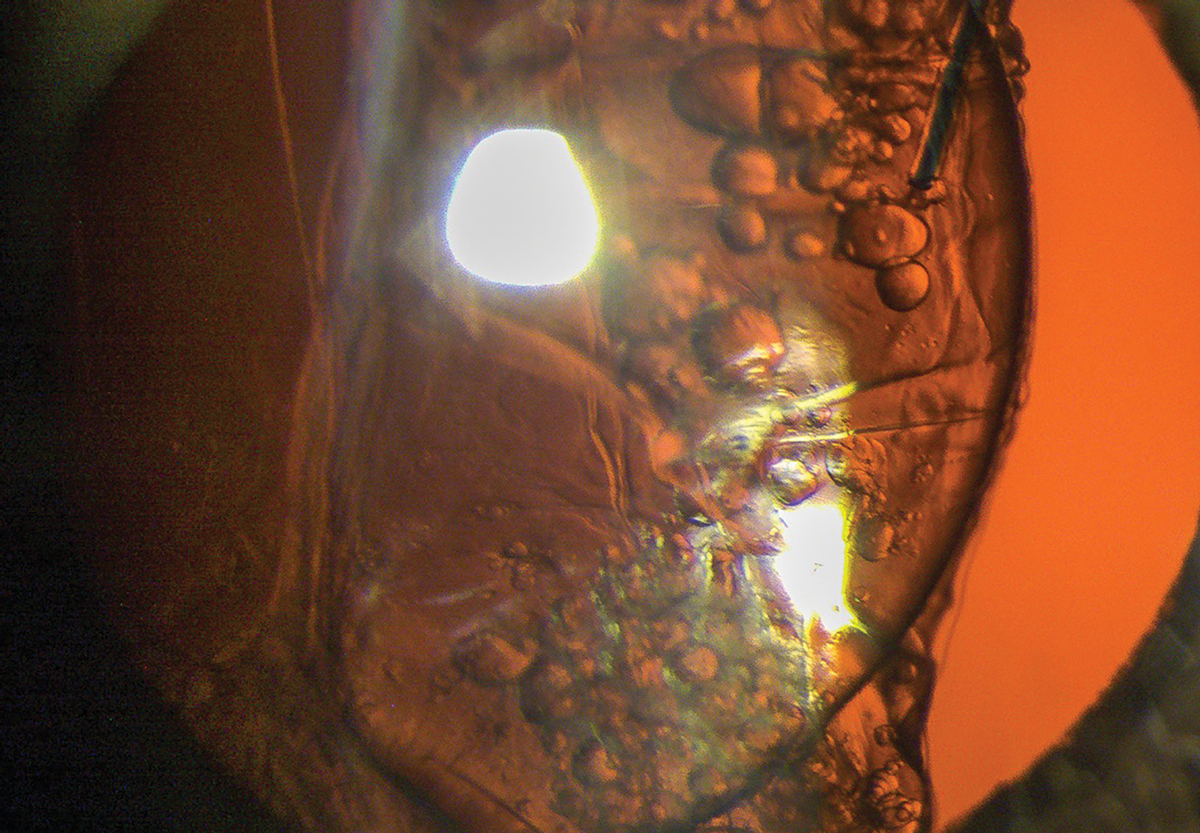
Fig. 1. The IOL was successfully placed within the capsular bag in a patient who had “loose zonules.” Click image to enlarge. |
Procedural Technique
Placing the first laser shots in the peripheral capsule superiorly is a prudent approach. If lens pits do occur, the pits will be peripheral to the line of sight. Lens pits from the laser rarely cause visual problems, but a practitioner should try to avoid lens pits near the line of sight. The use of a laser capsulotomy lens will also help stabilize the eye and lids, give better capsule visualization, and allow higher illumination use without patient photophobia and blepharospasm interfering with performing the capsulotomy. Once a few successful shots have been placed and a capsular opening is created, the capsule becomes easier to visualize despite IOL reflections, tints and glistenings.
IOL position also may play a role in capsulotomy technique and should be carefully evaluated prior to YAG laser capsulotomy. Ideally, the IOL optic and haptics are placed in the capsular bag at the time of cataract surgery. With IOL placement in the capsular bag, significant displacement of the IOL is not common. Mild IOL displacement that has the optic and haptics clearly in the capsular bag should not be of concern when performing a YAG laser capsulotomy.
 |
|
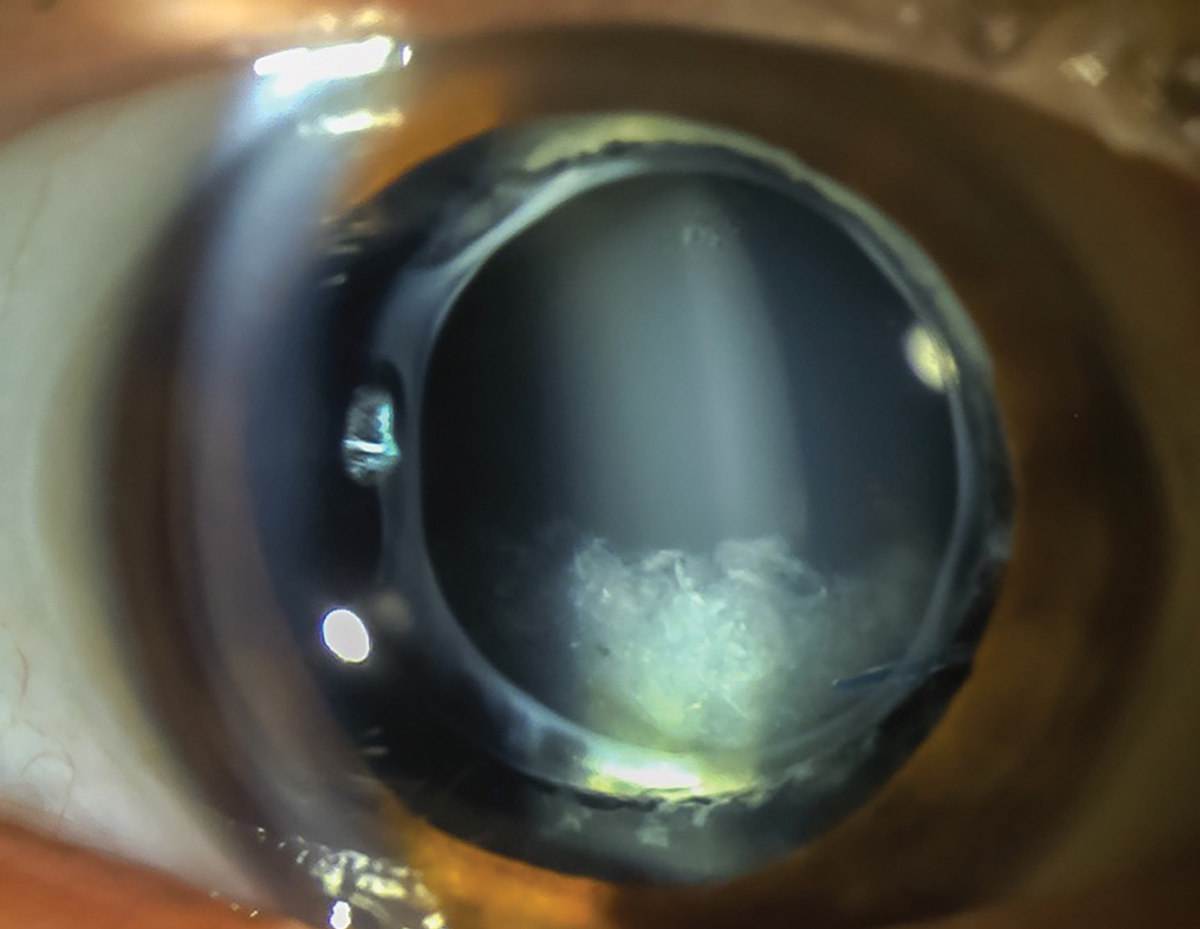
Fig. 2. Opaque, turbid fluid between the IOL and the posterior capsule is present in late capsular bag distention syndrome. Click image to enlarge. |
If the IOL is significantly decentered, careful evaluation should determine the cause of the displacement. If a capsular break or radial capsular tear occurred at the time of surgery, it may be difficult for the surgeon to place the haptics in the capsular bag, and the IOL may be fixated in the ciliary sulcus. Sulcus-fixated IOLs are less stable than IOLs fixated within the capsular bag and have a greater incidence of dislocating. Dislocation of sulcus-fixated IOLs is usually very gradual, but the energy released and capsular disruption that occurs with a YAG laser capsulotomy can cause a rapid dislocation of the IOL.
Sulcus-fixated IOLs are not a contraindication for YAG laser capsulotomy, but, because sulcus-fixated IOLs are less stable, IOL dislocation is more common. Higher laser energy levels used during capsulotomy increase the risk for IOL dislocation.
IOL decentration can also occur when the IOL is fixated within the capsular bag and there is zonular compromise causing a dislocation of the IOL-capsular complex. With significant zonular compromise, pseudophacodonesis may also be present. Depending on the degree of decentration and pseudophacodonesis, YAG laser capsulotomy may be contraindicated until the IOL and capsule can be surgically stabilized.
The patient shown in Figure 1 had “loose zonules” noted by the surgeon at the time of surgery, but the IOL was successfully placed within the capsular bag. During follow-up for the cataract surgery, the IOL was found to be well-centered and stable. The patient presented two years later with posterior capsular opacification (PCO), a decentered IOL, zonular dehiscence and pseudophacodonesis.
Due to the degree of decentration and pseudophacodonesis, YAG laser capsulotomy was delayed until the IOL and capsule could be surgically stabilized. The IOL was surgically repositioned, and the haptics were fixated to the sclera. After the patient had recovered from the IOL repositioning, a YAG laser capsulotomy was safely and successfully performed.
Other Considerations
Capsular distention and anterior capsular contraction (phimosis) are conditions that also require special consideration when laser capsulotomy is necessary. Capsular bag distention syndrome occurs when there is accumulation of fluid between the IOL and posterior capsule. This can occur early after cataract surgery, within days or weeks, or can occur late, months to years after cataract surgery.
Early capsular bag distention syndrome is associated with incomplete removal of viscoelastic material during cataract surgery. It frequently results in an anterior displacement of the IOL with a myopic refractive shift, shallowing of the anterior chamber, and elevation of the IOP. Treatment of early capsular bag distention syndrome includes surgical removal of the viscoelastic material vs. YAG laser capsulotomy. Surgical removal of the viscoelastic is usually the preferred treatment if there has been a significant anterior displacement of the IOL, since it will also allow for repositioning. If there is no IOL displacement, YAG laser capsulotomy will allow release of the accumulated fluid and alleviate the distention.
Late capsular bag distention syndrome occurs when lens epithelial cells produce collagen and extracellular material, which accumulates as an opaque, turbid fluid between the IOL and the posterior capsule (Figure 2). The turbidity of the accumulated fluid causes light scatter, producing symptoms of glare and decreased vision. It’s not uncommon for the posterior capsule to be relatively clear despite symptoms consistent with PCO. Treatment of late capsular bag distention syndrome is YAG laser capsulotomy.
 |
|
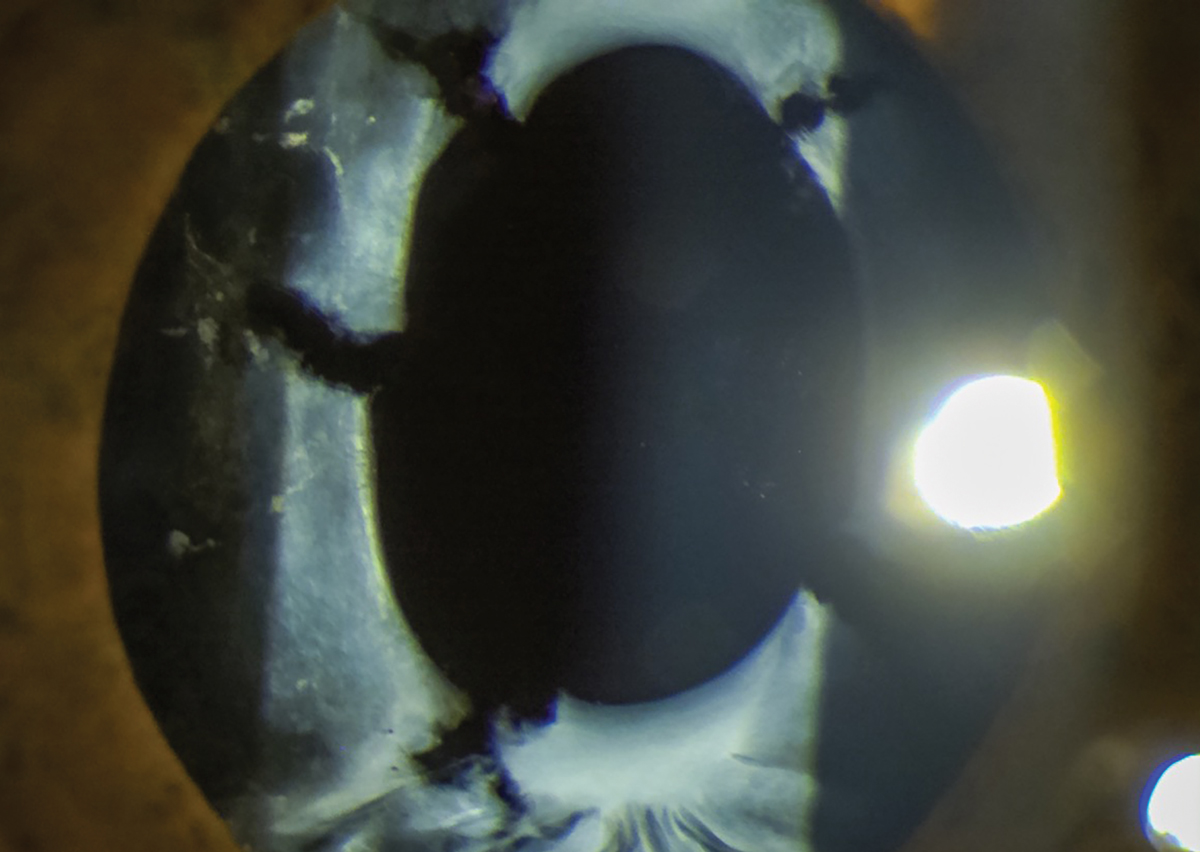
Fig. 3. Radial slits in the anterior capsule will stop the contraction from progressing and widen the diameter of the capsular opening. Click image to enlarge. |
Opening the posterior capsule in late capsular bag distention syndrome releases the turbid fluid into the vitreous where it will be absorbed. Since the fluid is opaque, it can make visualization of the posterior capsule difficult while performing YAG laser capsulotomy. Making the initial capsular opening in the inferior capsule will allow gravity to pull the fluid into the inferior vitreous allowing for better visualization of the posterior capsule. It may also be necessary to wait a minute or two after the initial opening is made, to allow the fluid to drain into the inferior vitreous. Once released, the fluid can sometimes cause mild inflammation and an increase in IOP, consequently it is prudent to place patients with capsular distention syndrome on 1% prednisolone acetate QID for one to two weeks following YAG laser capsulotomy.
Phimosis occurs when there is fibrosis of the anterior capsule and contraction of the capsulorhexis. Although phimosis usually occurs slowly, it can occur rapidly, within weeks of cataract surgery, especially in cases with excessive postoperative inflammation. Treatment for phimosis is YAG laser anterior capsulotomy and should ideally be performed before the contraction encroaches into the line of sight.
The treatment strategy is to make radial slits in the anterior capsule to break the contraction and widen the diameter of the capsulorhexis. If the fibrosis has not encroached into the line of sight, completely amputating the anterior capsule will not be necessary. Amputating pieces of the anterior capsule will result in those pieces dropping into the anterior chamber angle, whereas simply making radial slits in the anterior capsule will not leave capsular remnants in the anterior chamber angle.
Many physicians use a posterior offset when doing a YAG laser posterior capsulotomy. A posterior offset when doing an anterior capsulotomy will result in laser pits in the IOL. If you prefer to use a laser offset when doing a capsulotomy, it is important to change to an anterior offset before performing an anterior capsulotomy.
The anterior capsule is anatomically thicker than the posterior capsule and frequently requires more laser energy to break through the capsule. My typical starting laser settings for a YAG laser anterior capsulotomy are a 100µm to 200µm anterior offset and 2.5mJ to 3.0mJ. I place four to six radial slits in the anterior capsule, which will stop the contraction from progressing and will widen the diameter of the anterior capsular opening (Figure 3).
These simple strategies on atypical capsulotomy cases will make the procedure easier and will ensure better outcomes.
Dr. Barney is center director for Pacific Cataract & Laser Institute (PCLI) in Anchorage, AK. He is an adjunct faculty member of two US optometry schools and one international school of optometry.
Dr. Lighthizer is the associate dean, director of continuing education and chief of specialty care clinics at the NSU Oklahoma College of Optometry. He is a founding member and immediate past president of the Intrepid Eye Society. Dr. Lighthizer’s full disclosure list can be found here.1. Lighthizer N, Johnson S, Holthaus J, et al. Nd:YAG laser capsulotomy: efficacy and outcomes performed by optometrists. Optom Vis Sci. 2023;100(10):665-9. |

