 |
Anaphylaxis is an acute, potentially lethal multisystem syndrome. There are two primary anaphylactic reactions. One type, known as immunogenic, is a classic Type 1 hypersensitivity reaction most commonly mediated by IgE. The other, formerly called anaphylactoid, is triggered independently of an immune reaction.1
These two entities are indistinguishable clinically and the World Allergy Association has proposed referring to any severe, life-threatening, systemic hypersensitivity reaction as “anaphylaxis.”1 The World Allergy Association also proposes using “allergic anaphylaxis” when referring to immune-mediated reactions (IgE/immune complex) and “non-allergic anaphylaxis” when referring to immune-independent reactions.1
While the exact prevalence of anaphylaxis is unknown due to widespread underreporting, it is estimated between 1% and 2% of people worldwide are at risk for anaphylactic reactions.2-3 Furthermore, the incidence of anaphylactic reactions appear to be increasing in the industrialized world.1 Several known triggers for allergic anaphylaxis are shown in the literature, but any agent could potentially trigger an event and as many as 50% to 60% of cases are idiopathic.1,4 The most common triggers are foods, particularly nuts/peanuts, fish/shellfish and mammalian dairy.4 The second most common trigger is certain drugs, with beta-lactam antibiotics (penicillin and cephalosporin) and nonsteroidal anti-inflammatory drugs (NSAIDs) implicated.1 Other common triggers are insect bite/sting, latex and exercise.1,4-5
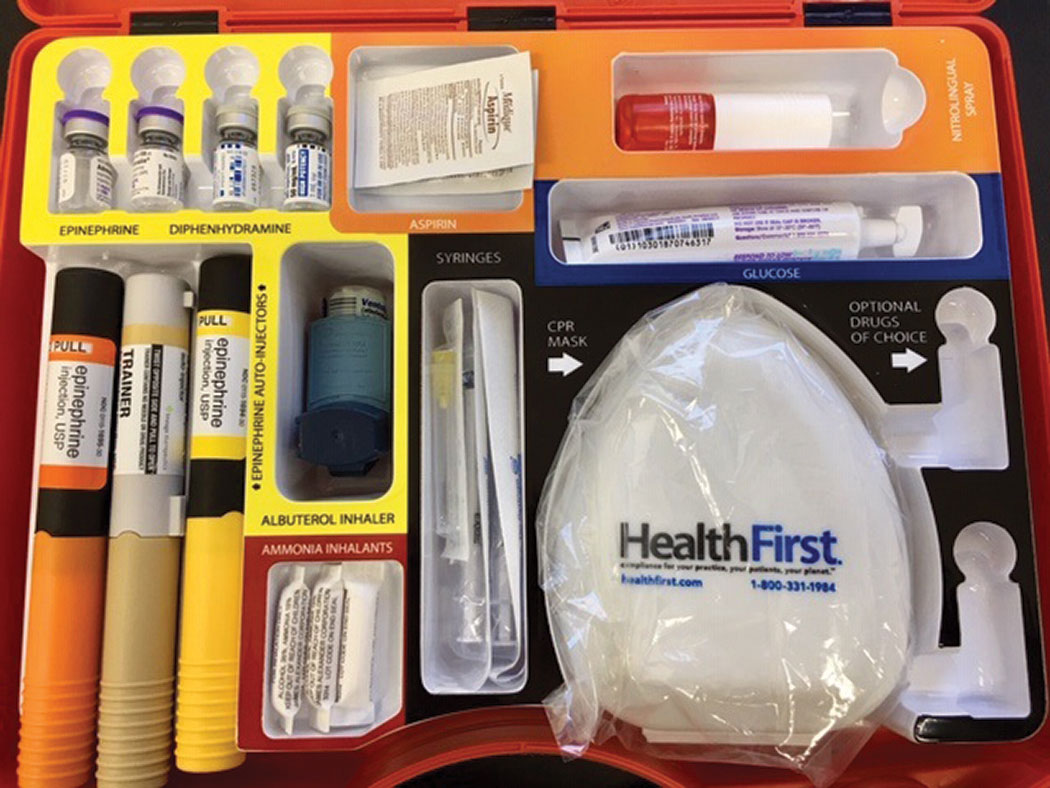 |
| This is the inside of an emergency kit used at Northeastern State University Oklahoma College of Optometry. |
With 1% to 2% of the population at risk, the variety and ubiquity of triggering agents, the rising prevalence and lethal potential of allergic anaphylaxis it is critical for all health care workers, including optometrists, to understand how to recognize and triage a patient in anaphylaxis.
Pathophysiology
Allergic anaphylaxis is a classic IgE-mediated Type 1 hypersensitivity. An antigen triggers B-cells to produce antigen-specific IgE, the IgE coats mast cells and basophils, and these cells become activated. Additional antigen exposure crosslinks the bound IgE and triggers massive degranulation of mast cell and basophil cell contents. The systemwide effect of this massive degranulation causes the morbidity associated with anaphylaxis.
Two of the most important factors released are histamine and products of arachidonic acid metabolism (prostaglandins, leukotrienes and platelet-activating factor). These chemicals cause smooth-muscle contraction, vasodilation and increased vascular permeability.1 Numerous neural proteases, proteoglycans and chemo-attractants are also released, causing large-scale immune cell recruitment, further degranulation and magnification of the immune response and reduced cardiac function.1,5-6
While allergic anaphylaxis is a multisystem disorder, the primary organs affected during a reaction are those of the cardiovascular and respiratory systems. The principal causes of death from anaphylactic shock are circulatory collapse and respiratory distress.1 The extensive smooth-muscle contraction can affect any level of the airway and lead to bronchiole constriction of the lower airway and laryngeal edema of the upper airway, both of which can cause asphyxiation.1 Extensive vasodilation and increased vascular permeability lead to massive extravasation of fluid out of the circulatory system, leading to a decrease in venous return, drop in blood pressure and clinical features consistent with hypovolemic shock.1,3
Anaphylaxis GuidelinesAnaphylaxis is highly likely when any one of the following three criteria is fulfilled: 1. Acute onset of an illness (minutes to several hours) with involvement of the skin, mucosal tissues or both (e.g., generalized hives, pruritus or flushing, swollen lips-tongue-uvula) And at least one of the following: a. Respiratory compromise (e.g., dyspnea, wheeze-bronchospasm, stridor, reduced peak expiratory flow [PEF], hypoxemia). b. Reduced blood pressure or associated symptoms of end-organ dysfunction (e.g., hypotonia [collapse], syncope, incontinence). 2. Two or more of the following that occur rapidly after exposure to a likely allergen for that patient (minutes to several hours): a. Involvement of skin-mucosal tissue (e.g., generalized hives, itch-flush, swollen lips-tongue-uvula). b. Respiratory compromise (e.g., dyspnea, wheeze-bronchospasm, stridor, reduced PEF, hypoxemia). c. Reduced blood pressure or associated symptoms of end-organ dysfunction (e.g., hypotonia [collapse], syncope, incontinence). d. Persistent gastrointestinal symptoms (e.g., cramp/abdominal pain, vomiting). 3. Reduced blood pressure after exposure to known allergen for that patient (minutes to several hours): a. Infants and children: low systolic blood pressure (age specific) or greater than 30% decrease in systolic blood pressure. Low systolic blood pressure for children is defined as less than 70mm Hg from one month to one year, less than (70mm Hg + [2 × age]) from 1 to 10 years, and less than 90mm Hg from 11 to 17 years. b. Adults: systolic blood pressure less than 90mm Hg or greater than 30% decrease from their baseline. |
Diagnosis
Due to the multisystem nature of the reaction, symptoms may vary, and not all patients will present the same symptoms.
Any time you administer medication, particularly if administering parenterally, monitor patients for symptoms of anaphylaxis. Symptoms will typically begin within minutes, but could potentially take hours to manifest. Common skin/mucosa symptoms include itch, generalized flushing, hives, angioedema (swelling of lips, eyes, tongue). Symptoms of respiratory compromise include coughing, sneezing, runny or congested nose, tightness of throat or chest, dyspnea, changes in voice, hoarseness, stridor, wheezing and hypoxemia.1,7 Symptoms of cardiovascular compromise include fainting, dizziness, sudden weakness, incontinence, chest pains, tunnel vision, difficulty hearing and tachycardia (heart racing) or bradycardia.1,7 Other symptoms include cramping, nausea, difficulty swallowing, mood changes and headache.1,7
The key to successful treatment of allergic anaphylaxis is rapid diagnosis. The faster treatment is administered the better. In 2006, researchers developed guidelines to help simplify the diagnosing process (See “Anaphylaxis Guidelines”).7
 |
| A convenient medical kit should include an epinephrine pen for anaphylaxis emergencies. |
Management
The goal of in-office treatment for allergic anaphylaxis is to maintain cardiovascular and respiratory function. Prompt treatment is vital. Treatment should be catered to the severity of the reaction. If anaphylaxis is suspected, the first step is to have a staff member call 9-1-1. While calling, the patient should be given 0.2cc to 0.5cc 1:1000 epinephrine IM. This is most commonly administered with a preloaded injection pen on the lateral thigh. Epinephrine (adrenaline) causes venous dilation and increased cardiac contractility countering the effects of cardiac insufficiency. Additionally, it causes smooth-muscle relaxation countering airway constriction. Epinephrine injection can be repeated every 10 minutes to 30 minutes as needed.
In the face of anaphylaxis, there is no absolute contraindication for using epinephrine.1 Following injection, immediately assess the patient’s airway, breathing and cardiac function (known as the “ABCs”). Administer CPR/BLS, including the use of an AED, if needed.
Assuming the patient is breathing and their heart is beating, continue in-office treatment. Place the patient in the Trendelberg position (lay on back with feet 15 to 30 degrees above the heart) to combat hypotension and maintain perfusion of vital organs. If the anaphylaxis stems from a medication injected into a limb, apply a tourniquet to that limb. Administer a combination of H1- and H2-blocking antihistamines. Diphenhydramine (Benadryl) 25mg to 50mg by mouth for H1 receptors. If the patient is unable to swallow, administer the drug subcutaneously or intramuscularly. Ranitidine (1mg/kg/dose) or cimetidine (adult 5mg to 10mg/dose) can be given by mouth, or parenterally if the patient cannot swallow.
If significant bronchospasm occurs, treat with two puffs of inhaled β-2 agonist (albuterol). While treatments are administered, monitor the patient’s vitals at least every five minutes until emergency medical help arrive. Due to the widespread systemic response and the large amount of chemotaxis of immune cells, relapse of symptoms is not uncommon. The patient may require additional monitoring and possible treatment in the emergency department. Such efforts may include IV fluids to reduce hypovolemia, IV epinephrine 1:10,000, vasopressive agents and systemic steroids to reduce inflammatory relapse.
Allergic anaphylaxis is a serious and life-threatening condition. With the prevalence at 1% to 2% of the population and the flow of patients through our practices, it is likely you will encounter it. As health care professionals, Optometrists are responsible for not just visual well-being but the health and wellness of the entire patient. For this reason, we need to be prepared to recognize and confront anaphylactic shock efficiently and effectively to save more than just the patient’s eyesight.
Drs. Krein and Krein are assistant professors at Northeastern State University in Oklahoma.
|
1. Lieberman P. Anaphylaxis. In Adkinson N, Bochner B, and Busse W (eds): Middleton’s allergy: principles and practice. 7th ed. St Louis: Mosby-Elsevier: 2009. 2. Gupta R, Sheikh A, Strachan D, et al. Increasing hospital admissions for systemic allergic disorders in England: analysis of national admission data. BMJ. 2003;327(7424):1142-1143 3. Decker W, Campbell R, Manivannan V, et al: The etiology and incidence of anaphylaxis in Rochester, Minnesota: a report from the Rochester Epidemiology Project. J Allergy Clin Immunol. 2008;122(6):1161-5. 4. Sicherer SH, Leung D. Advances in allergic skin disease, anaphylaxis, and hypersensitivity reactions to foods, drugs, and insect stings. J Allergy Clin Immunol 2004;114(1):118-24. 5. Pumphrey R. Fatal anaphylaxis in the UK, 1992-2001. Anaphylaxis. 2004;257:116-32. 6. Gri G, Piconese S, Frossi B, et al. CD4+CD25+ regulatory T cells suppress mast cell degranulation and allergic responses through OX40-OX40L interaction. Immunity 2008;29(5):771-81. 7. Sampson H, Munoz-Furlong A, Campbell R, et al. Second symposium on the definition and management of anaphylaxis. J Allergy Clin Immunol 2006;117(2):391-7. |

