 |
Q:
A 51-year-old presented as an emergency during the shelter-at-home period. She had complaints of a streak in front of her right eye, but her acuity was 20/20. A swollen nerve was noted without an afferent pupillary defect (APD). What is my differential diagnosis here?
A:
“When looking at the nerve—any unilateral swollen optic nerve—you have to consider optic neuritis,” says Nate Lighthizer, OD, an associate professor at the Oklahoma College of Optometry. One of the most common causes of a unilateral swollen nerve is optic neuritis. And one of the most common underlying causes of optic neuritis is multiple sclerosis (MS).
“Usually, if you’re asking for the typical demographics of optic neuritis that you see in all the textbooks and in the clinical trenches, those patients are in their 20s to 40s with a unilateral presentation of sudden vision loss,” Dr. Lighthizer notes. While this patient was not within this age range, he didn’t think she was too old for optic neuritis.
Ask Questions
“When you see unilateral nerve swelling in a patient no older than 50, have optic neuritis near the top of your differential,” Dr. Lighthizer says. Optometrists should look carefully for an APD using a very bright light source, such as a binocular indirect ophthalmoscope. Also, ask about pain on eye movements. This patient was an exception on all counts: older age, and no APD or pain on eye movements.
“When a unilateral swollen optic nerve presents, ask if the patient has been diagnosed with MS,” Dr. Lighthizer says. If the answer is no, they may be presenting to you with one of the classic signs of multiple sclerosis. To rule out multiple sclerosis, you will need to have neuroimaging done, according to Dr. Lighthizer. You can either order the scan yourself, or send the patient to a neuro-ophthalmologist or a neurologist,” Dr. Lighthizer notes. In our case, the MRI helped confirm the suspicion of MS.
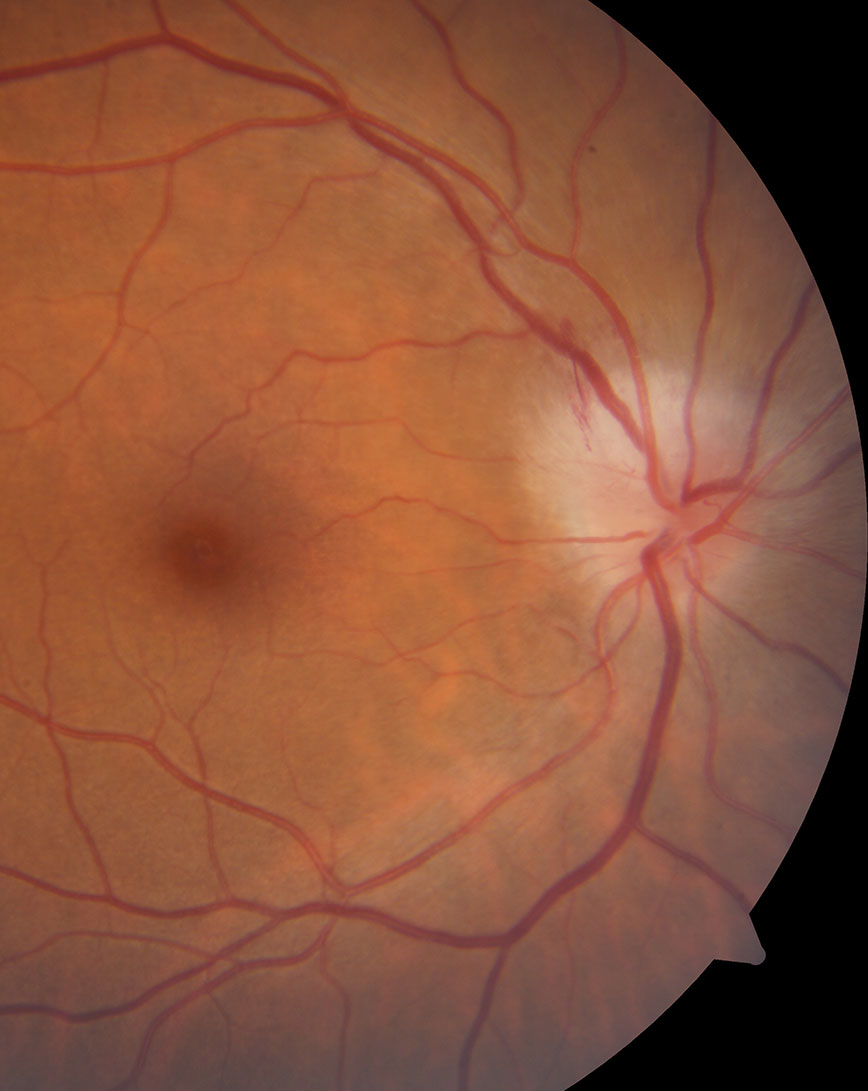 |
| While not the case with this patient, an APD, decreased vision and pain on eye movement often accompany optic neuritis. Click image to enlarge. |
Check History
Dr. Lighthizer reminds us to review the med the patient is on, along with conducting a detailed medical history, to eliminate other potential causes of the swollen optic nerve. Hypertension can reach such elevated stages that it can cause bilateral swollen optic nerves, also known as malignant hypertension.
“If an older patient presents with a history of obesity, high blood pressure for an extended period of time or uncontrolled diabetes, then non-arteritic ischemic optic neuropathy (NAION) is a much more likely diagnosis because of their vascular history,” Dr. Lighthizer says.
Treat Accordingly
The good news with optic neuritis is that it usually resolves even without treatment. However, high dose IV methylprednisolone for three days can accelerate healing and visual recovery. This is sometimes followed by oral steroids for about two weeks with a slow taper. “Usually the neurologist or the neuro-ophthalmologist will make the call to order the IV steroids,” notes Dr. Lighthizer.
He recommends that optometrists follow their patients every other week once they are out of the hospital. It is especially important to monitor their vision, pupils, visual field and nerve status in these cases. Be sure to communicate your findings clearly and regularly with the specialist.
Optic neuritis and MS can happen at any time to anyone of any age. Keep it on your radar, and remember to advocate for the patient and get them into the neurology system in a timely fashion. Be mindful this is not always an easy task.

