 |
A middle-aged woman suffers trauma to her left eye resulting in multiple symptoms and arranges for the next available appointment in a large ophthalmic practice several days later. Review of the electronic medical record (EMR) history of present illness (HPI) taken by a technician documents, “A 53-year-old female presents for an evaluation of pain in her right eye. Patient bumped into significant other’s collarbone five days ago. She complains about stinging pain and spasms every 10 minutes in the eye. She uses ice four times a day with little relief and Motrin (ibuprofen, Johnson & Johnson) to help with the pain. She states she is light sensitive.” Her general health history and previous eye history were both unremarkable.
In the EMR, visual acuity (VA) is recorded as 20/25 in each eye, the external exam listed an eyelid contusion OD, but location, size or sketch were not included. Slit lamp exam noted 1+ cells in the left eye only. A dilated fundus exam was recorded as normal, including the statement “flat x 360º, no retinal detachment, no holes.” The ophthalmic clinician (Dr. X) arrived at a diagnosis of “traumatic iritis in the left eye” and prescribed steroid eye drops, Pred Forte (prednisolone acetate ophthalmic suspension 1%, Allergan), to be used four times a day in the left eye. The patient was advised to return in a week, and the record does not reveal any indication of what to do if the condition worsened.
 |
|
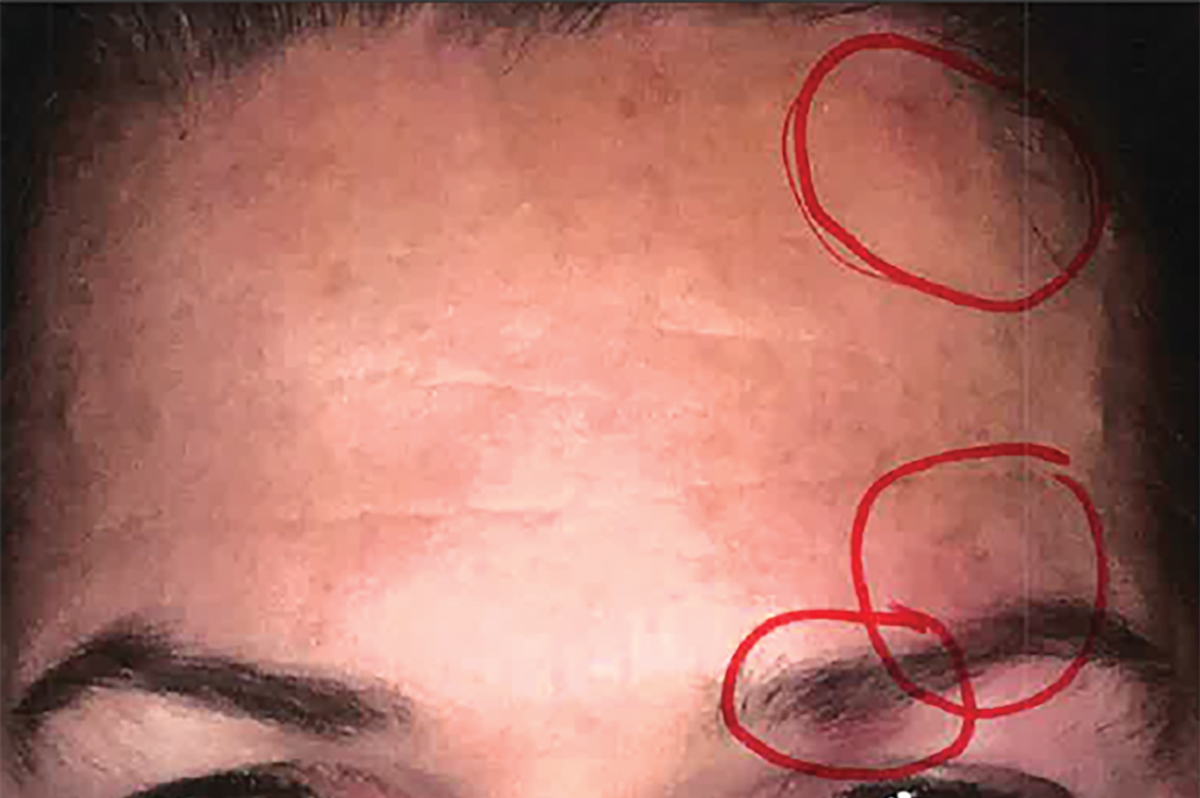
Fig. 1. The patient has acne lesions on both halves of the face but HZO on only the left side, with the circles highlighting rash/blisters. The three red circles were drawn by the neuro-ophthalmologist on the iPhone image taken a day prior to the exam in question. Click image to enlarge. |
Blisters and acne lesions are not noted anywhere in the EMR on this single exam with this ophthalmic clinician. The patient later produced iPhone images of her face dated a day before her exam and two days after her exam. She shared these images early one morning with her sister, a nurse practitioner who practiced more than a thousand miles away. Her sister opined that shingles was highly likely and that treatment with antivirals must begin immediately. An in-person exam several hours later with her primary care practitioner confirmed the diagnosis and the oral antiviral valacyclovir was initiated.
Later that same day, the patient was evaluated by a different eye clinician in the same group practice. The history on this visit revealed blisters around the left eye two days prior to the last visit when the first eye clinician arrived at a diagnosis of traumatic iritis. This second eye clinician noted vesicular lesions along the brow left eye, diagnosed herpes zoster keratitis and recommended to continue with Pred Forte eye drops QID and the valacyclovir as prescribed by the PCP.
Follow-up was at a major eye hospital a week later. The patient now reported extreme changes in vision OS: “very blurry and double vision.” The specialists here confirmed zoster keratitis and glaucoma OS, based upon IOPs of 28mm Hg in that same eye. The patient and her partner relocated to where her sister lived, and a anterior segment specialist took over care. A cataract developed OS, which was surgically removed, and treatment for glaucoma OS continued. Permanent corneal scarring OS resulted in best-corrected VA of 20/50-1 in the left eye with persistence of the “doubling.” Along with the visual issues, the patient developed post-herpetic neuralgia (PHN), which continued to be treated by a specialist.
You Be the Judge
- Based upon the information available thus far, what is your opinion?
- Did the patient have subtle vesicles on the first visit that were missed because of a rushed exam?
- Did acne lesions on both sides of the face mask the herpes zoster ophthalmicus (HZO) lesions?
- Could the trauma have precipitated the reactivation of the dormant chickenpox virus?
- Did the first eye clinician miss the window of opportunity to treat HZO?
- Is it likely that the patient presented on the first visit with both traumatic iritis and HZO?
Opinions Galore
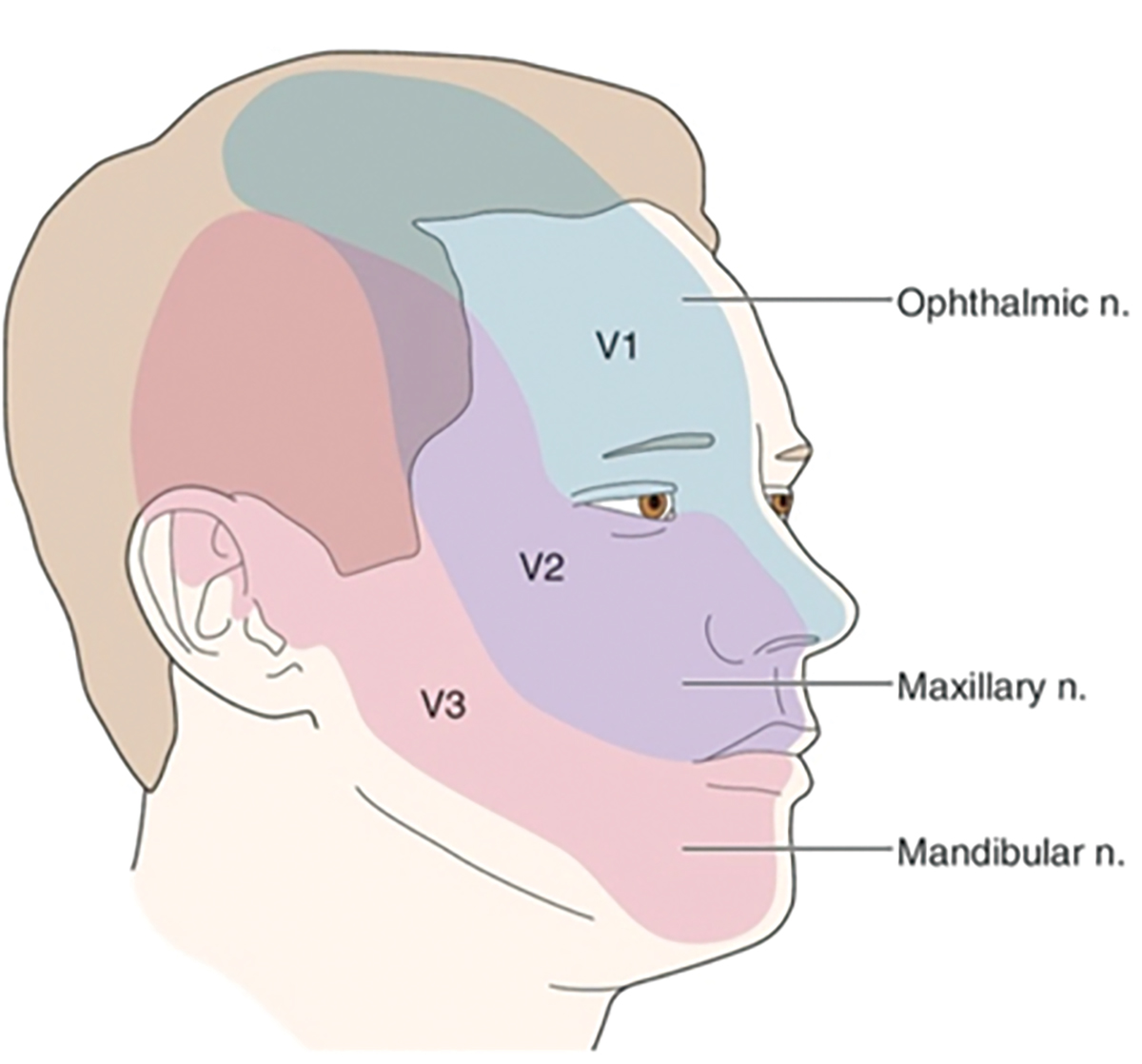
One of us (JS) was requested to review the case including the iPhone images provided by the patient. A renowned expert in neuro-ophthalmology also reviewed the case for the plaintiff and opined that iPhone images prior to and subsequent to the exam by Dr. X documented three zones of papillomacular rash/blistering on the left side of the face corresponding to the course of the ophthalmic division of the trigeminal nerve (Figures 1 and 2).
One expert identified by the plaintiff’s attorney was an MD who never practiced medicine but was “an IT professional rendering EMR-related opinions.” During his deposition, the man said that “The audit trail shows Dr. X spent seven to eight seconds interacting with the audit trail template, enough time to read the HPI paragraph but not enough time to have typed it.” This expert concluded that Dr. X spent seven to eight seconds reading the HPI entered into the EMR by the technician and then closed it, and hence did not add to it or change it. He further testified that there is no evidence that Dr. X documented an independent history and that, in that state’s Administrative Code, recording of details should be performed by a medical professional. When the technician testified, she admitted she was poorly trained at the time of the exam and was not instructed to ask follow-up questions such as “Is the pain worsening since the trauma?” She also admitted that she confused the eyes and this error was never corrected by the eye clinician.
 |
|
Fig. 2. Mapping of the course of the ophthalmic division of the trigeminal nerve, according to the neuro-ophthalmologist. Click image to enlarge. |
Three experts for the defense argued that the first iPhone image the day before the exam does not reveal evidence of HZO and that any lesions identified by the neuro-ophthalmologist expert could certainly be common acne. HZO, also known as ophthalmic shingles, is caused by the localized reactivation of the varicella zoster virus in the ophthalmic division of the trigeminal nerve. Previous systemic infection, typically childhood varicella, i.e., chickenpox, results in the virus lying dormant for decades in dorsal root and cranial nerve ganglia. The neuro-ophthalmologist presented literature that trauma can reactivate the dormant virus.
Permanent sequelae of HZO may include chronic inflammation, loss of vision and PHN. Antiviral medications such as acyclovir, valacyclovir and famciclovir are the mainstay of therapy and are most effective in preventing ocular involvement and PHN when begun within 72 hours after the onset of the rash.
She Said, She Said
The patient testified that she told the eye clinician that she began to develop blisters two days before the exam. When asked about the time that eye clinician spent with her during the exam, she testified that the exam was very brief and lasted “only a handful of minutes.” She also stated “and then I leaned into her and I said I have these weird blisters developing on my eyelid, and then I pointed ‘I have a small one on my forehead… she leaned into me and said, ‘Yeah, I see that.’” Comments were also made about sensations on her scalp. “I told her… shock-like sensations on my scalp… firecracker sensations” and then she noted, referring to the eye clinician, “she said that sounds like your nerve endings.” The patient also stated that she did not obtain the vaccine Shingrix (GlaxoSmithKline).
In contrast, the eye clinician testified that the patient never mentioned the blisters and never mentioned the shock-like sensations on her scalp. Who do you believe? The eye clinician also testified that she obtained an independent history, but it was the same as obtained by the technician and did not add to or change the HPI. This clinician also testified that she had previously diagnosed and treated more than 25 patients with HZO and missing a case would be unlikely.
This case did not settle, and a jury trial was scheduled in the jurisdiction of where the malpractice allegedly occurred. Several days prior to the jury trial, the plaintiff decided to withdraw from the case. Learning that the chances of winning a trial were not favorable and the expenses of both the patient and her significant other to travel to the location of the trial via airplane and hotel accommodations for at least several days, she decided to drop the case.1 We will never know the verdict of a jury and whether the vaccine Shingrix would have prevented this case of HZO.
PHN can be minimized by timely intervention. The standard of care for HZO is that antiviral therapy should be initiated within 72 hours after the onset of blisters to prevent or minimize injury and long-term sequela from the virus.
| NOTE: This article is one of a series based on actual lawsuits in which the author served as an expert witness or rendered an expert opinion. These cases are factual, but some details have been altered to preserve confidentiality. The article represents the authors’ opinion of acceptable standards of care and do not give legal or medical advice. Laws, standards and the outcome of cases can vary from place to place. Others’ opinions may differ; we welcome yours. |
Dr. Sherman is a Distinguished Teaching Professor at the SUNY State College of Optometry and editor-in-chief of Retina Revealed at www.retinarevealed.com. During his 52 years at SUNY, Dr. Sherman has published about 750 various manuscripts. He has also served as an expert witness in 400 malpractice cases, approximately equally split between plaintiff and defendant. Dr. Sherman has received support for Retina Revealed from Carl Zeiss Meditec, MacuHealth and Konan.
Dr. Bass is a Distinguished Teaching Professor at the SUNY College of Optometry and is an attending in the Retina Clinic of the University Eye Center. She has served as an expert witness in a significant number of malpractice cases, the majority in support of the defendant. She serves as a consultant for ProQR Therapeutics.
1. Levin G. What are the odds of winning a medical lawsuit? The Levin Firm. July 18, 2023. www.levininjuryfirm.com/what-are-the-odds-of-winning-a-medical-malpractice-suit. Accessed July 15, 2024. |

