|
Ernst Nicolitz, M.D.; and David Mills, M.D. |
Of all the advances in vision care in the last 25 years, wavefront analysis perhaps has the broadest potential applications. Although it was spawned from the refractive surgery revolution of the past 10 to 15 years, wavefront technology is based on the principles of adaptive optics used in astrophysics since the 1960s. Here, well discuss how wavefront technology is rapidly changing our fundamental understanding of vision, and improving our ability to diagnose and treat ocular and vision conditions.
Higher-Order Aberrations
The evolution of refractive surgery technology and procedures introduced us to the quantitative and qualitative effects of higher-order aberrations on vision.
And, the accuracy of the excimer laser has made one thing apparent: The weakest link in refractive surgery perhaps is the standard refraction. Specifically, a standard refraction measures lower-order aberrations (second-order sphere or defocus, and cylinder), generally in 0.25D steps. However, the total aberrations of the eye produced by the cornea, aqueous, lens, vitreous and the numerous changes in indices of refraction of light rays include up to 20% higher-order aberrations such as coma and trefoil (third order); spherical aberrations and quadrafoil (fourth order); and increasing levels of irregular astigmatism (fifth through eighth order). Because these aberrations represent refractive abnormalities well below the 0.25D unit (equivalent to about 3m of tissue change), the higher-order aberrations require measuring systems and instrumentation well beyond contemporary, standard refractive technologies.
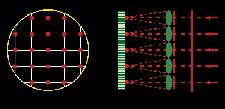
If the light leaving the eye has no aberrations, all the rays of light will be parallel. Each ray of light will be perpendicular to an imaginary plane called the wavefront, or in this case a perfect wavefront.
If you have aberrations in the eye, the light rays leaving will not be parallel to each other and will look something like this. And again those rays of light are all perpendicular to an imaginary plane called the wavefront. Courtesy: Steven H. Linn, O.D.
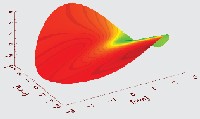
The science of adaptive optics provides such measuring capabilities through its use of root mean square deviations, or RMS units. These measure light deviations and aberrations down to 0.01m, which is equivalent to about 0.001D. Computerized measuring sensors constructed with deformable lenslet systems and other measuring sensors can calculate RMS coefficients and convert them into a polynomial pyramid (the Zernike pyramid) of 3-D models or 2-D color maps that represent lower- and higher-order aberrations of an optical system.
These Zernike polynomials, measured up to the 11th order, can provide analysis of virtually 100% of the aberrations of an eye. Recent research, however, has found that the aberrations at the periphery of this pyramid are inconsequential in human vision and that Zernike coefficients above the 6th order actually begin to create nonproductive noise when used in calculations of human vision.1
Thus, we now rely on other systems, particularly point spread function, to measure and assess higher-order aberrations in human vision. Point spread function (PSF) simply is the quantification (and qualification in subjective assessments) of a spot of bright light on a dark background (e.g., a bright star in a dark sky). The retinal image of a Snellen letter could be considered the negative of PSF. In other words, suppose the patient reads the 20/20 line on the Snellen chart with or without lower-order correction but reports distortions, haloes, tails and/or double (overlapping) images. This patient, in effect, is qualifying his higher-order aberrations in terms of PSF.
Wavefront Technology
The next step in the quest to identify, measure and eventually correct the higher-order aberrations in human vision is to quantify them in Zernike, PSF and RMS terms. This, in fact, is the new vision science of wavefront analysis and the new role of wavefront aberrometry.
Thanks to such optical researchers as David Williams, Ph.D.; Ray Applegate, O.D., Ph.D.; Larry Thibos, Ph.D.; and others, we can now utilize adaptive optics in wavefront aberrometry to measure the higher-order aberrations of human vision. This new capability allows us to measure the remaining 20% of the human visual system and seek the full potential of a patients vision. That potential visual acuity can reach as high as 20/8 with maximal retinal and cortical function.1
We now have numerous sensing and measuring methods for wavefront analysis (also called aberrometry). These include:
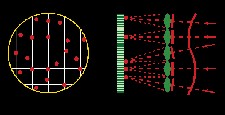
This wavefront map showing astigmatism is the result of aberrations shown above.
Hartmann-Shack, such as LadarWave (Alcon), Zyoptix (Bausch & Lomb) and WaveScan (Visx).
Tscherning, such as the Wavelight Allegretto Wave excimer laser system system (WaveLight).
Ray tracing, such as the Tracey Visual Function Analyzer (Tracey Technologies).
Dynamic spatial skiascopy, such as 3-DWave (Marco Ophthalmic).
Holographic imaging, such as Z-View Aberrometer (Ophthonix).
Each commercial wavefront aberrometer has strengths and weaknesses. So, too, does the general science of wavefront. These strengths and weaknesses will have a profound impact on the scope and precision of diagnostic refractive care, on current and evolving forms of refractive treatments (surgical and non-surgical) to correct lower- and higher-order aberrations, and on everyday clinical practice.
Diagnostic Applications Wavefront Systems Available Today Refractive surgery has come a long way since the 1970s, when Russian ophthalmologist Svyatoslav Fyodorov had lines of people waiting outside his clinic to undergo surgery that would rid them of glasses.
While photoablation and conventional LASIK can adequately correct the lower-order aberrations (sphere and cylinder), they aggravate and induce higher-order aberrations in the eye. The original goal of using wavefront-guided custom ablation was to correct higher-order aberrations. Now, the more realistic goal is for the surgeon to induce fewer aberrations, which are associated with the corneal biological and biomechanical insult resulting from refractive surgery.
Also, wavefront may be equal or more valuable in diagnostic applications. Actual or potential diagnostic applications include:
Refraction. Today, refraction captures about 80% of the eyes aberrations (lower-order). Wavefront analysis will allow us to expand that to 100% accuracy. So, when a patient asks about correction thats better than 20/20, you will be able to maximize the patients full eyeball focusing potential. Through an aberrometers vector analysis software, a blended astigmatic correction of lower and higher order cylinders without the need for which is better one or two? refinements will make refractions faster and more accurate. The patients retinal/ neural limitations then become the deciding factor of their best-correctable visual acuity.
But will the visual cortex be able to handle that full potential? Careful consideration and studies into the perceptual aspects of higher-order corrections will be an evolving science of the future.
By J. Christopher Freeman, O.D.; and Steven J. Dell, M.D.
Since Dr. Fyodorov first performed radial keratotomy, the field of refractive surgery has seen a transformation to lasers with small optical zones and then to lasers with large optical zones, blend zones and now custom, wavefront-guided ablations.
There are currently three FDA-approved custom, wavefront-guided laser systems available in the United States:
The Alcon LadarVision 4000 laser. This is coupled with the LadarWave wavefront analyzer to make up Alcons wavefront-guided ablation platform, known as CustomCornea. This system became the first FDA-approved laser system for wavefront-guided excimer laser ablation in October 2002. The Alcon laser is also a flying spot laser with spot size of 0.8mm. It has an optical zone size up to 6.5mm with a blend out to 9.0mm.
In June 2004, the FDA expanded the treatment range for the CustomCornea wavefront platform; surgeons can now use it to treat up to 8.00D of myopia and up to 4.00D of astigmatism.
The Ladarwave system is another Hartmann-Shack aberrometer with Zernicke polynomial-based conversion to the laser. It can measure up to a 7.0mm area of higher-order aberrations. The Alcon systems FDA clinical trials show 80% of patients had 20/20 vision six months post-operatively.
The VISX Star S4 CustomVue platform. This system has a treatment range of up to 6.00D of myopia and up to 3.00D of astigmatism. The VISX system was FDA approved in May 2003 and 94% of patients achieved results of 20/20 six months post-operatively in the FDA clinical trial, and 74% achieved 20/16 or better. The VISX system uses what is called variable spot scanning with a spot size that varies from 1mm to 6mm. The optical zone size is FDA approved for up to 6mm and can treat up to 6.5mm with a blend out to 8mm.
The S4 uses the ActiveTrak, 60Hz, infrared video-based eye tracker, which measures eye movement in the x, y and z axes. The wavefront analyzer for the VISX platform is called the WaveScan. Its a Shack-Hartmann aberrometer that uses Zernike polynomials to represent each aberration. This systems software will be converted from Zernike to a higher-resolution, Fourier Transfor analy sis of the aberrometry. This, in turn, should lead to more precise laser ablations and improved visual outcomes.
Bausch and Lombs Zyoptix. This was approved by the FDA in October 2003. It combines the Zywave Hartmann-Shack wavefront analyzer and Orbscan IIz topographer with the Technolas 217z flying spot laser. The Zywave aberrometer can measure aberrations beyond a 7.0mm pupil, while the Orbscan provides full corneal pachymetry and elevation. The 217z laser system features varying spot sizes of 1 to 2mm with an FDA-approved fully corrected optical zone size as large as 7.0mm blending to 9.0mm for custom treatment.
Zyoptixs FDA clinical trial data showed 78.3% of eyes had uncorrected visual acuity greater or equal to pre-op best-corrected visual acuity, while dim light contrast sensitivity either improved or remained the same as pre-op in 97.9% of patients. No patient expressed dissatisfaction with the procedure.
Meanwhile, Carl Zeiss Meditec plans to begin U.S. clinical trials of its MEL 80excimer laser system. Our laser center was selected to be one of the study sites. The Zeiss laser, also a flying spot system, is an extremely fast laser that operates at 250Hz and uses a 250Hz video-based tracker.1 The spot size is very small at 0.7mm. The CZM MEL 80 ablation profile is aspheric, rather than spherical, to match the strongly curved cornea.
In a 2002 study, conducted in Belgium and presented at the 2003 ESCRS meeting, one-year postoperative results with this laser showed that 88% of patients achieved 20/20 without custom, wavefront treatment.
We can expect that custom, wavefront-guided LASIK will continue to be our procedure of choice for the majority of our patientsthe low and moderate myopes. Expanded ranges of custom, wavefront treatments are on the horizon. We live in an exciting time of vision correction surgery, one that will only get better for our patients as technology quickly advances.
Dr. Freeman is fellow trained in cornea and refractive surgery and is optometric director at Dell Laser Consultants in Austin, Texas. Dr. Dell is a surgeon, author, and lecturer on refractive surgery and is medical director of Dell Laser Consultants.
1 Goes F. One year LASIK experience treating Myopia with the Carl Zeiss Meditec MEL 80 LASER. Presented at the ESCRS Munich, September 2003.
We will be able to analyze eyes not correctable to 20/20 so accurately that we will have the ability to segregate out each of the visual systems components (eyeball aberrations, retinal/neural function and cortical perception). This will allow us to distinguish normal functions from physiological and/or pathological factors causing reduced vision.
Differentiation of corneal and crystalline lens aberrations. This will be an important part of determining what type of refractive procedure, if any, is best for a patient. We can achieve this by combining wavefront readings and corneal topography. While topography can interpret corneal aberrations, we must subtract corneal topography from the total wavefont aberrations to quantify the aberrations caused by the internal eye and lens. This allows precise assessment of lens effects, including residual astigmatisms and aging changes well before cataract formation.
Near corrections. Dynamic accommodation changes the profile of higher-order aberrations in the eye. By assessing and comparing aberrations under static and dynamic visual conditions, we can more accurately determine, diagnose and prescribe near corrections both in young and aging patients.
Pre-testing refractive surgery candidates. By determining the patients precise lower- and higher-order aberration profile, eye care practitioners will be able to identify patients for whom certain procedures may not adequately correct or may even aggravate their principal visual problem(s). For example, patients who have significant or advancing lens aberrations may not be appropriate candidates for corneal-based procedures considering immediate and certainly long-term results.
Diagnosis of post-refractive procedural or corrective device complaints. We will be able to precisely diagnose visual complaints and compare them to pre-procedure or device correction. This will enable the surgeon and the optometrist to precisely assess what variables may have been introduced from the target correction in the virgin eye (e.g., induced aberrations in corneal refractive surgery). Early diagnosis of problems such as lens tilt, decentration and posterior capsule opacification associated with intraocular lenses will help solve the patients visual symptoms and provide earlier corrective interventions.
Retreatment considerations and decisions. We will be able to consider whether to retreat any form of surgical or non-surgical correction through wavefront analysis with the greatest accuracy and assessment of potential outcomes for such post procedure or device interventions.
Ocular surface assessments. We will be able to assess the ocular surface in a manner not previously obtainable at the micron level, including pathologic and physiologic conditions of the tear film (e.g., dry eye, post-blink tear instability), influences of the upper lid (e.g., vertical coma secondary to blepharoptosis), anterior basement membrane disorders and other surface abnormalities. Such assessments will identify related visual disturbances that we previously could not diagnose.
Also, diagnostic instrumentation with wavefront analysis and the use of adaptive optics will change how we examine and diagnose the human eye. In the very near future, we will examine ocular tissues and structures using slit lamp biomicroscopes and ophthalmoscopes equipped with adaptive optics. This will provide viewing capabilities at the micron level. This degree of clinical accuracy will enhance diagnostic precision relative to the degree, location, intensity and progress of pathological and physiological tissue change.
Corrective Applications
Still, the proverbial holy grail in clinical wavefront technology for us and our patients will ultimately be the measurement, fabrication, subjective verification (cortical assessment) and correction of higher-order aberrations in human vision. Rapid advancements are being made in these areas as clinical research begins to move beyond just corneal surgical approaches for wavefront correction.
For example, use of biosynthetic materials combined with programmable photosynthesizing, electro-chemical and even nanoconstructed optics will result in stable, permanent intraocular and surface implants, spectacle lenses and contact lenses that can correct higher-order aberrations. All such corrective devicesnotwithstanding challenges of fitting accuracy, stability (any HOA-correcting lens must center perfectly with no movement or rotation for point-to-point pupillary zone correction) and predictabilityare approaching the realm of practical, routine prescribing.
Other Applications
Wavefront-guided and assisted custom corneal ablation uses a narrow-beam excimer laser precisely guided by wavefront computer software. The software is programmed to the lower- and higher-order aberrations of the patients eye.
This procedure will likely become the standard for all corneal photoablation for two reasons: First, outcome data demonstrates that custom corneal ablation minimizes the induction of higher-order aberrations normally associated with laser photoablation. Second, photoablation of prescription powers difficult or impossible to treat with conventional procedures can be achieved with custom corneal ablation.
Another use of wavefront-guided ablation: Fixing previous surgical disasters. Decentered ablations, irregular astigmatism, old corneal refractive procedures (e.g., radial keratotomy) and even induced higher-order aberrations from previous procedures are within the realm of repair with the precision of wavefront guided custom ablation.
Certain corneal abnormalities such as keratoconus and other topographic and surface abnormalities can be effectively treated with wavefront-guided custom ablations. Results may often not be optimal, but alone or with other modalities, such treatments have produced better outcomes than previous alternative approaches.
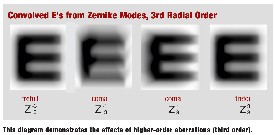
This diagram demonstrates the effects of higher-order aberrations (third order).
Finally, IOLs such as the Tecnis IOL (AMO) are being developed using prolate anterior surfaces to significantly reduce spherical aberrations. Biosynthetic materials that can be fabricated and adjusted down to greater than 1m accuracy are now being used in IOL design. These capabilities provide for a potential process to preoperatively measure higher-order aberration, fabricate an IOL correction; implant it precisely; and then verify and even fine tune the correction (e.g., the light adaptive lens by Calhoun) postoperatively.
Non-surgical applications include:
Corneal onlays. Biosynthetic materials applied to the surface of the cornea to correct refractive errors already are available. These maintain precise optics, mimic the human cornea and can be lasered and permanently (or reversibly) fixed with bioadhesives. Examples include PermaLens (Anamed) and ReFrax (MedRx).
Contact lens corrections. We already have aspheric soft contact lenses designed to reduce spherical aberrations such as the Frequency 55 Aspheric (CooperVision), Definition AC (Optical Connection) and Choice AB (CIBA Vision).
Now, custom-made contact lenses that can correct higher-order aberrations while maintaining precise centration with no movement or rotation are being developed. This is being accomplished through high permeable, large scleral hydrogel skirts combined with gas permeable, central programmable optics. One product in clinical trials is SynergEyes (Quarter Lambda Technologies).
Spectacle lens options. Also known as intelligent spectacles, these incorporate a central portion of their optics (or even throughout the entire distance to near channel) programmed with invisible lenslet-like segments that are wavefront-designed and can correct higher- order aberrations. One such product is the Z-Lens (Ophthonix). Again, precise frame measurements and stable fitting and adjustment for point-to-point correction will be critical in all such corrective devices.
Genetic engineering methods. These methods, aimed at manipulating corneal cells, tissues and proteins (e.g., glycosaminoglycan or ground substance) are being developed. The idea is to provide controlled healing and micron-level adjustments of corneal curvatures and surface characteristics. This, in turn, would produce wavefront accuracy (potentially greater than 0.5m) for refractive correction.
Wavefront technology represents a major advance in the science of vision care and its clinical value for eye care practitioners and their patients. Its immediate and long-term diagnostic and corrective applications will significantly change the way we diagnose and treat ocular conditions and refractive errors. Your patients, your practice and the optometric profession need it and will benefit significantly from it.
Drs. Catania, Henson, Nicolitz and Mills practice at Nicolitz Eye Consultants in Jacksonville, Fla. Dr. Catania frequent lectures on evolving refractive surgery technologies.
1. Krueger R, Applegate R, MacRae S, eds. Wavefront Customized Visual Correction: The Quest for Super Vision II. Thorofare, N.J.: Slack Inc., 2004.

