 |
An 87-year-old Black woman was referred to the eye clinic for a cataract evaluation. She wanted a second opinion regarding the necessity of cataract removal, OU. Her systemic history was remarkable for hypertension, which was well controlled with oral medication daily. She denied allergies of any kind.
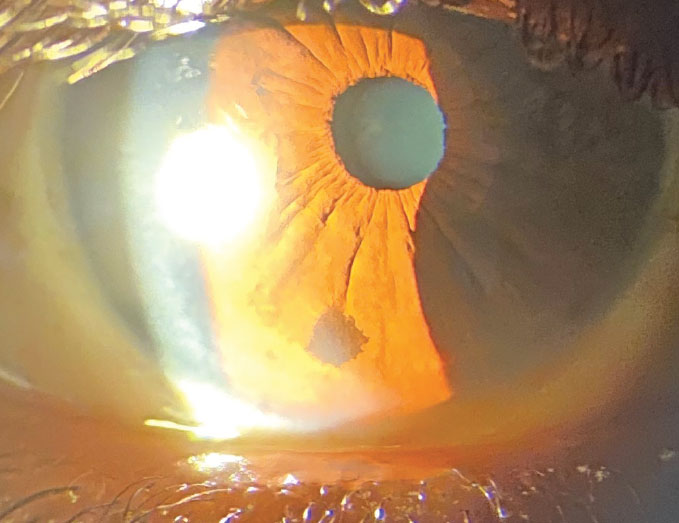
Her best-corrected entering visual acuities were 20/30 OU at distance and near. Her external examination was normal and there was no afferent pupil defect. The pertinent finding OD, discovered during the biomicroscopic exam of the anterior segment, is demonstrated in the photo. Goldmann applanation tonometry measured 15mm Hg OU. The dilated fundus exam findings were normal.
Additional studies included photodocumentation and referral to an ocular oncologist to ensure no additional testing such as ultrasonography or biopsy was required.
 |
|
Slit lamp exam of the patient revealed these findings. What might be the prognosis? Click image to enlarge. |
Differential Diagnosis
The condition described in this issue is iris nevus. The choroid, ciliary body and iris make up the uveal tunic of the eye. Uveal melanoma (UM) is the most common primary intraocular malignancy in adults.1 Uveal melanoma (UM) has an incidence of seven per 1,000,000 in the western hemisphere.1 Iris melanoma comprises 4% to 10% of all UM cases and has a lower mortality rate.1 Iris nevus is a common finding, with 6% of patients suspected of iris melanoma having a lesion that is an iris nevus.2 In fact, when an iris melanoma is misdiagnosed, up to 36% of them are nevi.2 While a nevus lesion itself is benign, they have the potential to turn into melanoma with a rate of approximately 8% at a mean of 15 years.2
Shields et al. studied 200 patients referred for suspected iris melanoma and most (76%) were found to be lesions not consistent with iris melanoma.3 They termed these lesions pseudomelanomas.3 The most common pseudomelanomas included iris cyst (38%) and iris nevus (31%).2,3
There are some predictive clinical factors that may indicate risk for growth and or malignant transformation. In a paper by Shields they were labeled “A-F” and include the following:2,4
A. detection at a young age
B. the presence of blood (hyphema)
C. clock hours of coverage that include inferior portions of the iris
D. diffuse presentation (larger lesions)
E. ectropion uveae observed at initial presentation
F. feathery margins rather than symmetric, well-defined borders.
Nevus/lesion diameter and thickness can be measured in millimeters by slit lamp biomicroscopy, ultrasound biomicroscopy or anterior segment OCT.2-4 Likewise, these clinical modalities can be used to monitor discovered lesions for stability and progression.
Intravenous fluorescein angiography (IVFA) of the iris and OCT angiography (OCT-A) can add information about the vascular architecture of suspicious iris lesions.2-4 Disadvantages of IVFA include its invasive nature, lengthy procedure time, serious adverse reactions and potential for blockage of dye leakage by dense pigment.2,3 In contrast, while incapable of demonstrating leakage (as there is no dye used), OCT-A often defines the texture of the iris vasculature better; in cases where iris pigment blocks IVFA findings, it provides a better and more complete visualization of a feeder network.2,3
Iris tumors are broadly classified into cystic or solid lesions.5 The former arise from the iris pigment epithelium or iris stroma.5 Cysts traditionally remain stable without any need for intervention.5 Stromal iris cysts, especially those discovered in newborns, may require aspiration or surgical resection.5
Solid iris tumors include melanocytic and nonmelanocytic lesions.5 The melanocytic iris tumors include nevus (e.g., melanocytoma), Lisch nodules, Busacca/Koeppe nodules and melanoma.5-7
Lisch nodules are hamartomas of the iris (of the same tissue) found in association with neurofibromatosis type 1.6 These nodules are present in 92% of postpubertal patients with neurofibromatosis type 1 and are typically found inferiorly on the iris.6
Koeppe and Busacca nodules are focal accumulations of granulomatous inflammatory debris that appear on the iris in anterior uveitis.7 They are designated as Koeppe nodules when located at the iris margin and Busacca nodules when located away from it.7
Intervention and Prognosis
Management of iris nevi mainly involves documentation of size and location, ideally with anterior segment photography. New lesions should be re-evaluated in three to six months to monitor for growth; however, patients should return to the office immediately should they recognize any change in size, shape, color or elevation. Established lesions may be monitored annually for changes with photography or anterior segment OCT-A if available.
Since published information documents transformation of suspicious iris nevi into iris melanoma at 4% over 10 years and 11% by 20 years, timely, expert evaluation is critical with at least an initial evaluation, if not yearly input.
Treatment options include surgical resection, enucleation, brachytherapy and proton beam irradiation.1,9,10 Currently, no studies on targeted adjuvant therapies in primary or metastatic iris melanoma exist. The choice of treatment depends on tumor size, localization and patient preference. Diffuse iris melanomas are difficult to recognize, causing a delay in diagnosis.1,9,10
This patient was referred to Dr. Shields for an initial evaluation and found to have a benign iris nevus. They will be appointed to see the specialty group yearly unless other changes facilitate moving up the evaluation.
Dr. Gurwood thanks Dr. Nick Karbach for his contributions to this case.
Dr. Gurwood is a professor of clinical sciences at The Eye Institute of the Pennsylvania College of Optometry at Salus University. He is a co-chief of Primary Care Suite 3. He is attending medical staff in the department of ophthalmology at Albert Einstein Medical Center, Philadelphia. He has no financial interests to disclose.
1. van Poppelen NM, Vaarwater J, Mudhar HS, et al. Genetic background of iris melanomas and iris melanocytic tumors of uncertain malignant potential. Ophthalmology. 2018;125(6):904-12. 2. Allegrini D, Montesano G, Pece A. Optical coherence tomography angiography of iris nevus: a case report. Case Rep Ophthalmol. 2016;7(3):172-8. 3. Shields JA, Sanborn GE, Augsburger JJ. The differential diagnosis of malignant melanoma of the iris. A clinical study of 200 patients. Ophthalmology. 1983;90(6):716-20. 4. Shields CL, Kaliki S, Hutchinson A, et al. Iris nevus growth into melanoma: analysis of 1611 consecutive eyes: the ABCDEF guide. Ophthalmology. 2013;120(4):766-72. 5. Shields CL, Shields PW, Manalac J, Jumroendararasame C, Shields JA. Review of cystic and solid tumors of the iris. Oman J Ophthalmol. 2013;6(3):159-64. 6. Nichols JC, Amato JE, Chung SM. Characteristics of Lisch nodules in patients with neurofibromatosis type 1. J Pediatr Ophthalmol Strabismus. 2003;40(5):293-6. 7. Shaikh N, Kumar V, Venkatesh P. Iris nodules in Fuchs heterochromic iridocyclitis. Indian J Ophthalmol. 2019;67(8):1339. 8. Postolache L, Parsa CF. Brushfield spots and Wölfflin nodules unveiled in dark irides using near-infrared light. Sci Rep. 2018;8(12):18040. 9. Mensink HW, Vaarwater J, de Keizer RJW, et al. Chromosomal aberrations in iris melanomas. Br J Ophthalmol. 2011;95(3):424-8. 10. Sandinha MT, Kacperek A, Errington RD, Coupland SE, Damato B. Recurrence of iris melanoma after proton beam therapy. Br J Ophthalmol. 2014;98(4):484-7. |

