 |
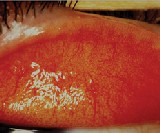
| Dry eye and ocular inflammation can prevent successful contact lens wear. Courtesy: Mark Andre. |
The 29-year-old accountant, a new patient in optometrist Douglas Benoits Concord, N.H., practice was ready to give up on contact lens wear. He experienced dryness and decreased vision with his daily wear soft lenses as the day progressed. Rewetting did not help. He was considering returning to spectacles or undergoing LASIK.
Another new patient, a 31-year-old female office worker, did discontinue contact lens wear. She wore soft contact lenses, but stopped due to discomfort as the day wore on.
These are just two of the 2.7 million patients who discontinue contact lens wear each year. Indeed, the problem facing contact lens practice isnt getting new patients to try contact lenses but how to keep them in lenses. We would be doing fantastically if we could stop or slow the rate of dropouts, says optometrist Peter Bergenske of
|
Case Report: LASIK Evaluation Uncovers Degeneration |
|
By HEATHER COWDEN, O.D.
A 50-year-old white male presented for a pre-op LASIK evaluation. He complained of blur with his best spectacle correction and indicated that he had been unsuccessful with soft contact lenses several years earlier because the lenses didnt fit right. The patient denied any significant medical history, medications or drug allergies.
Best-corrected spectacle visual acuity was 3.50 O.U., 20/25- O.D. and +1.50 4.25 x 097 20/30- O.S. Slit lamp biomicroscopy, intraocular pressures and dilated fundus examination were all unremarkable. Automated keratometry readings were 42.61 x 42.83 O.D. at 007 and 39.38 x 43.77 at 092 O.S.
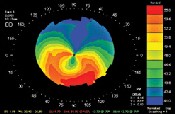
Corneal topography revealed the classic crab-claw appearance of pellucid marginal degeneration in the left eye and similar, though less severe, changes in the right eye.
We diagnosed the patient with pellucid marginal degeneration that was greater in the left eye than the right. So, this patient was not a candidate for laser refractive surgery.
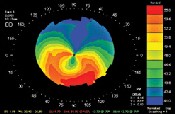 |
| Corneal topography of another patient reveals the classic crab-claw appearance of pellucid marginal degeneration. Courtesy: Arthur B. Epstein, O.D. | Although bitoric gas permeable contact lenses are a common treatment option for pellucid marginal degeneration, the patient preferred to try soft torics one more time.
We trial fit the patient with a Frequency 55 (CooperVision) spherical soft contact lens in his right eye using 3.50D power, a median base curve and a 14.4mm diameter. Distance vision through the right lens was 20/20, with full coverage and 1.00mm movement on blink.
We successfully fit the patient with a Frequency 55 Toric XR soft contact lens O.S. with power of +1.50D 4.25 x 100, a base curve of 8.7 and a 14.4mm diameter. Visual acuity was 20/30 with the lens rotated 5 to the left, full coverage and 1.00mm of movement on blink. We changed the base curve to 8.4, which resulted in 20/25+ acuity and better stability. The Frequency 55 Toric XR is available in 5 steps, so we did not adjust the axis of the left lens.
The patient was very happy with the modest improvement in visual acuity we achieved, but even more pleased with the qualitative image improvement he gained with the soft torics. We continue to monitor the patient in our clinic, and he is mindful that a future GP fit may dramatically improve the vision in his left eye.
Clinical Pearls
Pellucid marginal degeneration (PMD) is a condition that results in inferior corneal ectasia and steepening inferiorly, producing significant corneal with-the-rule and irregular astigmatism. PMD usually presents between ages 20 and 40. The topographical appearance is one of a butterfly or crab-claw.
Early in its course, PMD may be mistaken for early keratoconus. However, pachymetry reveals normal central corneal thickness. Once you have ruled out keratoconus, be careful not to overlook the PMD and recommend refractive surgery.
Look for distorted mires or scissors reflex on retinoscopy. You may also see inferior corneal thinning that spans 1-2mm in width between 4 and 8 oclock on topography or on slit lamp examination.
Rule out GP contact lens-induced warpage, particularly from lid-attachment lenses. Such warpage may mimic PMD. However, a change in GP fit, or temporary refit into soft contact lenses, may result in a return to normal topography and make the patient a possible refractive surgery candidate.
Treatment for PMD typically requires a rigid contact lens fit for best visual function, although soft aspheric and soft toric contact lenses are sometimes viable options for providing functional visual acuity. Penetrating keratoplasty may be required, although results are frequently poor.
Dont forget to try additional custom made soft toric lenses, even in those who have degenerations and dystrophies or who may have failed with previous versions of soft lenses. Dr. Cowden practices at Bergstrom Eye and Laser Clinic in Fargo, N.D., with interests in ocular disease and pre- and post-operative eye care. |
Pacific University College of Optometry.
Thats why our 28th Annual Contact Lens Report focuses on how to prevent dropouts. Well look at how the S.O.A.P. (subjective, objective, assessment and plan) exam format can troubleshoot problems. That way, you may prevent dropouts and perhaps refit previously unsuccessful wearers.
Subjective: The Case History
When patients complain of dryness or discomfort, take a careful history to determine the cause of the problem. A lot of times, I found that if I had only gone in and questioned the patient a little more thoroughly, I could have prevented a dropout, says Jane S. Buckland, a contact lens technician and consultant with Unilens.
Some questions to ask:
When does the discomfort occur? If a patient revealed they were experiencing end-of-day discomfort/dryness, I would try to find the source of the problem, says optometrist Nicola Pritchard, a research optometrist with Visioncare Research Ltd., a research company that specializes in eye care research. A detailed history of the patients everyday environment is necessary. This may dictate whether you replace the lens material or find other ways to rehydrate the lens.
How often do you replace your lenses? In other words, does the patient follow the replacement schedule? Some 35 to 40% of patients wear lenses longer than the recommended schedule, says optometrist Lyndon Jones, Ph.D., of the Centre for Contact Lens Research, Waterloo. For example, theyll wear two-week disposables for four weeks.
What care system do you use? Dont assume that patients are using the care products you recommended. Other care products may not be cleaning their lenses well enough, thus leaving behind deposits. Or the patient may be experiencing a reaction to the preservatives. Instead, instruct patients to bring their contact lens solutions to their follow-up exams. Our motto is the solution is guilty until proven innocent, says Mark Andre, director of the contact lens service at Casey Eye Institute in Portland, Ore.
What medications do you take? Common prescription medicationsantidepressants, antihistamines, birth-control pills, hormone replacement therapy and acne medicines, to name a fewcan cause dryness.
Do you use any hand creams, face creams, hair spray or makeup? These things will cause problems with most contact lens wearers, Ms. Buckland says. Specifically, these agents can remain in the skin. When the patient inserts contact lenses, the lenses absorb them.
Even if patients dont present with complaints about their contact lenses, you might still ask open-ended questions. Some examples:
Is there anything that you would like to improve?
How do your eyes feel at the end of the day? Do you do anything during the day to try to make them feel better?
How is your vision at night?
|
Material Does Matter |
|
A 50-year-old white female wearing five-year old gas permeable lenses (material unknown) presented to our office to obtain different contact lenses. She said she experienced dry, irritated eyes in the morning, and her lenses filmed up at the end of the day. Also, her monovision correction was not working as well as it did initially.
The patients current prescription was 6.25D with a 7.92mm base curve and 8.2mm diameter O.D. and 5.50D with an 8.0mm base curve and 8.2mm diameter O.S. She had stopped wearing her contact lenses several days before this visit.
Refraction at this visit measured 7.00D with best-corrected visual acuity 20/20 O.S. and 6.00D with best-corrected acuity 20/25+ O.D. Keratometry readings were 43.00 x 45.00 @ 090 O.D. and 42.75 x 44.75 @ 089 O.S. Biomicroscopy revealed clear lids and lashes, no corneal staining upon fluorescein instillation and slight conjunctival injection O.U. The tear volume and break-up time were within normal limits. The rest of her examination was also normal.
The patient initially rejected our suggestion of a superpermeable material, mainly due to cost and durability considerations. She also wanted to continue wearing monovision, even though we explained the compromises to distance vision and depth perception. We discussed the availability of auxiliary prescription spectacles over the contact lenses to improve function for driving or reading, if desired.
After diagnostic fitting, we ordered her lenses in the Boston XO material with a Polycon design: 6.75D with a 7.85mm base curve and 9.5mm diameter for 20/20+3 O.D. and 4.25D with a 7.90mm base curve and 9.5mm diameter and 20/30 O.S. at near. Upon dispensing, the patient was very happy with the visual acuity her contact lenses provided. The increased diameter did cause an initial difference in edge feel, but she adapted quickly.
Corneal health remained intact, but as she adapted to the lenses, her comfort decreased due to significant coating of the lenses as the day progressed. Follow-up examination demonstrated very coated lenses at the end of the day, with a lipid-protein combination. We tried alternative GP lens care systems along with enzymatic cleaners, with no improvement. We decided to try another GP material.
We trial fit her with the Menicon Z alpha 1 material and the Paragon HDS 100 design. Both demonstrated a distinct improvement in comfort and wettability for this patient. We also discussed care products; we wanted no gritty cleaners, and our goal was to prevent total lens dehydration to maximize lens life. The powers and base curves of her new prescription were the same, but we changed the lens diameter to 9.6mm in both eyes.
Lens coating did not occur with the new lenses. An earlier trial using Systane drops during lens wear was not effective. We tried Refresh Endura bid and Refresh Liquigel, before and after lens wear. This patient experienced marked comfort improvement with the Refresh Liquigel.
Clinical Pearls
We can still keep middle-aged women in contact lenses despite drier eyes and reduction in their daily comfort levels. Patients may report reduced wearing time, reduced visual clarity and dryness. By refitting them into alternative materials, reviewing and modifying their care system, and even adding an auxiliary treatment, we can usually offer them better comfort and increased wearing time.
For the middle-aged dry eye patient, reviewing medications, vitamin usage, water consumption, make-up removal products (avoid anything oily or greasyno baby oil or petroleum jelly!), the lens care system and handling of the lenses as well as topical lubrication options are important.
Persistence is key. The payoff is great for you and your patient.
Keep the soft lenses moving even when using a high flux lens such as Focus Night and Day. Try using steeper peripheral curves on the RGP to assure adequate flushing of debris from beneath the lens.
Dr. Keech is in private practice in Shoreline, Wash. |
A lot of studies have shown that a number of patients are getting by or just tolerating [lenses], but theyre not really successfully wearing them if you ask them to define what they consider success, Dr. Benoit says.
A lot of [patients] will have symptoms that you overlook, adds optometrist S. Barry Eiden, of North Shore, Ill. Theyre at a higher probability of dropping out.
Furthermore, if the patient is a previous contact lens wearer, you might want to ask about what type of lens he wore, why he was not successful, what he liked or didnt like about the lens, and if he experienced any ocular allergies or injury. What Im trying to do here is uncover why the patient is not a good candidate for a particular lens, Ms. Buckland says.
Objective: The Exam
Your history will dictate the exam portion of the visit. If a patient complains of dryness, youll want to do a standard exam for dry eye. You want to make sure that the eye can produce a healthy tear film. Dont jump in and try changing solutions or lenses, because the eye itself is not healthy enough to be wearing that lens, says Dr. Jones.
Ideally, you will have done a thorough evaluation before you fit the patient in contact lenses. This includes checking for blepharitis and meibomian gland dysfunction, evaluating the tear meniscus and tear breakup time (TBUT) and checking for debris in the tears. Another important area: Check for superficial punctate keratitis or neovascularization, and check the bulbar and tarsal conjuctiva for abnormalities. If there are any abnormalities, these need to be addressed beforehand, Dr. Benoit says.
Again, youll want to check the tear film and pay careful attention to the lids and lashes. Treat any meibomianitis and blepharitis. Dr. Jones advice: Have patients continue wearing their contact lenses to see if treatment of meibomianitis and blepharitis makes a difference. For significant cases, a course of oral antibiotics followed by a careful monitoring may be necessary prior to any lens wear.
The slit lamp exam is especially important for diagnosing the cause of the patients problem. Some specific elements to look for:
Lens fit. The practitioner has to be able to look at the lens on the eye and see how it is working, says Huntington Beach, Calif., optometrist Glenda B. Secor. A lens that doesnt center properly or fits too tightly or too loosely will affect comfort. Look for subtle changes, and document everything so that you can determine whether it is pre-existing or the result of wearing contact lenses.
Also, remove the patients lenses and stain them with fluorescein; this may yield additional clues as to whats causing the patients discomfort, Dr. Secor says.
Corneal staining when the patient removes his lenses. Corneal staining could indicate a soiled lens or a chemical reaction. If the cornea is clear but the patient has dry eye symptoms, Mr. Andre says, evert the upper lid to check for inflammation. That usually means reaction to care products, or a dirty lens. Then you usually need to go over the care and handling with patients.
Also check for giant papillary conjunctivitis, which would indicate undiagnosed allergic disease. Inflammation of the upper lid also tends to be present with allergies, and requires treatment.
|
Case Report: A Useful Approach for Keratoconus |
|
By Susan Resnick, O.D.
A 25 year-old white male was referred by a corneal specialist for a final attempt at a contact lens fitting. He had discontinued lens wear six months ago.
The patient was diagnosed with keratoconus five years earlier and had several unsuccessful contact lens trials. Soft lenses proved to be visually inadequate, and the patient reported a marginal tolerance of gas permeable lenses with a maximum wearing time of six hours. The patient wished to wear lenses comfortably while working a 10-hour day, with rest on the weekends if necessary. After a clinically acceptable, bilateral fit was achieved with the Rose K keratoconus design, the patient still experienced an unacceptable level of discomfort.
 |
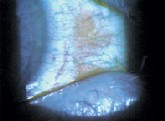
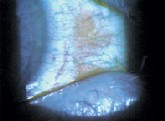
| A piggy-back modality of improved comfort in this keratoconus patient. |
The patients best-corrected acuity was 20/30-1 O.D. with a spectacle correction of 0.75 2.00 x 010, and 20/40-2 O.S. with spectacle correction of 3.00 4.25 x 108. Keratometry readings were 43.75@046/ 48.75@136 O.D. and 47.75@026/55.00@ 116 O.S. Axial topography depicted inferiorly displaced oval cones that were more advanced in the left eye than the right. Slit lamp examination revealed only mild apical thinning in both eyes, without scarring, Vogts striae or Fleischers rings. All other anterior and posterior segment findings were within normal limits. Medical and ocular history was otherwise non-contributory.
We trial fit the patient in Rose K lenses made from the Boston ES material. Lens parameters were 3.25D, 8.3mm diameter and 7.4mm base curve O.D. and 7.00D,
8.3mm diameter, 6.7 base curve and 1.0mm flatter peripheral curves O.S. The lens centered well, and achieved acceptable movement and fluorescein patterns (feather touch to minimal apical clearance). Best-corrected acuity upon dispensing was 20/25+1 O.D. and 20/30+2 O.S. We prescribed an initial wearing schedule of four hours, building by two hours each day.
The patient returned a week later and reported acceptable vision but moderate, persistent lens awareness O.U. Maximum comfortable wearing time was five hours.
The patients prior unsuccessful attempts with multiple GP design and parameter modifications suggested that his lens tolerance issues were likely due to lid sensitivity. So, we tried a piggy-back modality with Focus Night and Day lenses 0.50D in an 8.4mm base curve. The advantage to these lenses was their high Dk value. The patient reported an immediate improvement in comfort and has had no difficulties wearing his lenses for 12 hours a day, seven days a week. Follow-up visits over the past year revealed stable vision and refraction and no adverse corneal changes.
Clinical Pearls
Piggy-backing can be an excellent option in cases of patients with high degrees of physical sensitivity. It may also be considered if you cannot achieve adequate GP lens centration with the rigid lenses alone, or for patients who have elevated apical scarring (nodules) or recurrent epithelial breakdown.
Select lenses with high oxygen permeability, and monitor patients carefully for signs of corneal swelling or neovascularization, particularly if used on a post graft patient.
First, evaluate the fit and fluorescein pattern of the rigid lens on the cornea, and then make any necessary adjustments to accommodate the flatter curvature of the overlying soft lens. This is an excellent tool in your arsenal for preventing a potential contact lens dropout and perhaps, as in this case, saving the patient from possible surgery.
Dr. Resnick is in private practice in Melville, N.Y. |
Again, check the tear meniscus, the tear quality, staining (while lenses are off) and TBUT, says Dr. Benoit. The surface of the lens is especially important. If its getting dry, theyll have decreased vision, and the surface wont have a smooth appearance, he says. Also, youll notice colored fronds, similar to the rainbow effect you might observe in a puddle of water.
Especially important, Dr. Benoit says, is to note any problems even if the patient doesnt complain. Its a matter of taking the objective findings and subjective findings and putting them together.
Assessment and Plan
Depending on what youve discovered by this point, you can now take proactive steps to keep the patient in contact lenses. Some specific things you can do:
Change the solution. The approach we like to take with these patients is to first eliminate preservatives from their care system, either by putting them in single-use lenses or some [other] preservative-free system, says Dr. Bergenske. If that doesnt take care of the problem, then the issue is more what I call true dryness from the eye.
Prescribe artificial tears. If the patient has medically induced dry eye and cant change medicine, supplement with artificial tears, preferably preservative free, Mr. Andre says.
Consider other dry eye treatments. We need to educate them about wetting agents, artificial tears, lid hygiene, flax oil supplements, silicone hydrogel lenses (which have less dehydration of water and provide more oxygen to the cornea) and, if appropriate, punctal occlusion, says optometrist Joseph P. Shovlin of Scranton, Pa. And, we need to tell patients with allergies about the advantages of daily lens replacement. Simply having patients remove lenses mid-day for 30 minutes or more, store them in sterile solution and re-insert them may provide additional comfort.
Dont forget to recommend that the patient drink six to eight glasses of water daily and avoid foods that can dry eyes out, Dr. Eiden says.
Prescribe rewetting drops. If patients comply with your instructions yet still have problems with dryness, consider drops that lubricate and rewet. Remind patients to use them throughout the day rather than waiting until theyve experienced end-of-day discomfort. Rewetting drops work; they can help, Dr. Bergenske says. The problem is that they have to be used frequently enough to make a difference.
His suggestion: Instill drops at least five times daily.
Consider a new lens material. Once youve made certain that the patient is abiding by the replacement schedule and using rewetting drops, consider changing lens materials.
One study found that by changing from a low-Dk material to a high-Dk silicone hydrogel, you may be able to alleviate discomfort and dryness for some patients.1,2
And, many patients who have worn silicone hydrogel lenses have reported significant improvement at the end of day. The rate of water loss and amount of water loss with silicone hydrogels is less than with conventional, so theres less of a drying effect on tears, Dr. Jones says.
The new Acuvue Advance lens (Vistakon) contains Hydraclear, an internal rewetting agent that wets the lens from inside out. According to clinical trails, 87% of Acuvue Advance wearers said they were still comfortable after eight or nine-hours of lens wear.
|
Case Report: High Dk for Dry Eye |
|
By Susan Resnick, O.D.
A 45-year-old, white male patient had tried many times over the past 16 years to wear contact lenses, but significant dry eye symptoms limited his wear to four hours per day
on the weekends only. He had tried many lens materials and designs since but achieved no improvement in comfort and tolerance, so he resigned himself to contact lens failure.
The patient was in excellent general health with no significant ocular health history. He has been a patient in our office for some 16 years and every two years presents for routine examination and a trial with new contact lenses. He desires soft lenses only, as he is a weekend athlete and plays contact sports.
Anterior segment examination was within normal limits. Tear break-up time measured 7 seconds. I noted no significant corneal staining or meibomian gland dysfunction, but mild diffuse conjunctival staining was present. Tarsal conjunctivae revealed trace diffuse papillae. Tear volume testing (phenol red thread) yielded 15mm in 15 seconds.
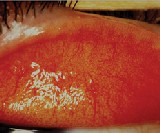
 |
| A silicone hydrogel lens may reduce dryness in this dry eye patient. Courtesy: Review of Contact Lenses | Subjective manifest refraction yielded 2.25D sphere O.U., with best-corrected acuity of 20/20 in each eye. A +1.00D add was acceptable binocularly. Keratometry measurements were 44.50 @ 180/44.25 O.D. and 44.00/44.00 O.S.
The patient had no objection to wearing reading glasses at work, but preferred contact lenses for his sports activities. His chief complaint with multiple lens designs over the years was significant lens awareness after one hour of wear, which he described as dryness. The lenses that had given him the best comfort and longest wear time (four hours) were Acuvue 2 with an 8.4mm base curve.
Given his relative comfort with Acuvue 2 lenses, we offered the patient a trial with the new Acuvue Advance design. We completed a trial fit with the lenses using 2.00D 8mm base curve O.U. The lenses centered well and exhibited 0.5mm movement with blink and on upgaze. The lenses exhibited excellent on-eye hydration.
The patient initially reported excellent comfort. We dispensed the new lenses with appropriate multipurpose solution and prescribed an initial wear schedule of four hours per day, building by two hours each day, up to a total of 10 hours.
The patient returned a week later and reported comfortable wear at the 10-hour level. He even felt he could wear the lenses longer, if appropriate. Slit lamp examination with and without the lenses was entirely within normal limits. We advised the patient to build to a 14-hour wear time. Three months later, he wears the lenses comfortably on a full, daily wear basis.
Clinical Pearls
Acuvue Advance lenses are based on the design of the Acuvue 2 lens, with the same lower-edge profile and enhanced midperiphery. The material, galyfilcon A is a silicone polymer with a Dk/t of 85. Silicone hydrogels, besides having higher oxygen benefits, may also decrease dryness for some patients.
Dry eye patients present the biggest challenge to the contact lens practitioner and probably comprise the largest segment of the contact lens dropout population. Higher Dk/t materials are the newest option in our armamentarium for dry eye patients. With excellent motivation on the part of both the patient and practitioner, success may still be within reach, even for patients who have previously been unsuccessful. |
Dont just think of silicone hydrogels for continuous wear. I think its a real travesty that were pocketing silicone hydrogels into the continuous wear category, Dr. Jones says. I think they have a significant part to play in daily wear and managing patients.
In fact, the Acuvue Advance lenses are approved for two-week daily wear, not 30-day continuous wear.
Changing the lens material may also help eliminate two other reasons patients discontinue contact lens wear: redness and deposits. Most cases of redness are driven by hypoxia, Dr. Jones says. Silicone hydrogel materials can result in white eyes, usually within three to four weeks of wear. For patients who are heavy depositors, consider a frequent replacement option and perhaps even a daily disposable.
Also consider lenses such as Proclear lens (omafilcon A, CooperVision) and Extreme H2O (hioxifilcon A, Hydrogel Vision Corporation). The manufacturer says Extreme H2O retains its saturated water content on the eye, even under extreme conditions. Also, studies show that Proclear has been successful in a dry eye population, providing some patients with better comfort, fewer symptoms, less on-eye dehydration and less corneal staining than other lenses.2,3
Address the patients astigmatism. By giving the patient full correction, you may have a better chance of keeping them in contact lenses. Mr. Andres advice: Correct them like you would with spectacles. Dont compromise their vision with lesser powers or a spherical equivalent for the sake of saving the patient money or time.
|
Case Report: From Monovision to Multifocal |
|
By Susan Resnick, O.D.
A 53 year-old white female physical therapist and avid tennis player presented one year ago with interest in resuming contact lens wear. She had stopped wearing contact lenses two years earlier, but before that had successfully worn PMMA and gas permeable lenses for more than 30 years. As she became increasingly presbyopic, she found that monovision no longer suited her visual needs. She did not want to be dependent upon reading glasses for all her near tasks.
The patient reported no significant ocular history. Current medications included Paxil (paroxetine, GlaxoSmithKline) and Ritalin (methylphenidate hydrochloride, Novartis) for mild depression and anxiety, and Vioxx (rofecoxib, Merck) as needed for tendonitis. Contact lens history was significant for good vision and comfort with rigid lenses until two years earlier, when she became intolerant of an increase in her monovision prescription. She found the further loss in binocularity unacceptable, especially while playing tennis, and reported only a marginal improvement in reading vision.
Subjective manifest refraction was 6.25D 0.25 x 135 with best-corrected acuity of 20/20 O.D. and 5.25D sphere with best-corrected acuity of 20/20 O.S. She accepted a +2.00D add O.U. Keratometry revealed 44.75@140/45.50 O.D. and 44.75@008/45.75 O.S. Her right eye was the dominant eye. The cornea, lids and lashes were clear. Pupil size measured 5mm in scotopic illumination.
We chose a simultaneous vision lens to accommodate the patients need for good binocular vision in varying angles of gaze, particularly for distance and intermediate tasks. She was less concerned about sustained near tasks and was not opposed to auxiliary reading glasses if necessary. We fit a Tangent Streak no-line back surface aspheric (Fused Kontacs) in the Boston ES material using the following parameters: 6.75D, 9.5mm diameter and a 7.45mm base curve O.D. and 6.25D, 9.5mm diameter and a 7.40mm base curve O.S. in Boston ES material. The lenses centered well, and acuity was now 20/20 O.U.
One year later, the patient continues to be satisfied with acuity and comfort. She finds her near acuity adequate and does not rely upon reading glasses, even for small print, provided that illumination is adequate. Should she require a greater add in the near future, she might be able to tolerate +0.25D to +0.50D in her left eye, the non-dominant eye.
Clinical Pearls
The key to success with presbyopic gas permeable lenses is to work with at least two different designs each of simultaneous vision and translating bifocals/multifocals.
Assess the patients needs and set realistic expectations. This will permit incipient and advancing presbyopes to continue to enjoy contact lens wear well into the future. |
We have a number of patients who are not entirely satisfied with the lenses because of visual complaints. Its often because of uncorrected astigmatism, adds Dr. Jones. Patients with -1.00D cylinders who come in uncorrected complain that visual acuity is not as good as with spectacles.
For some patients, GP lenses might be a more appropriate option for correcting higher amounts of astigmatism (e.g., 2.00D or higher). If its a case of corneal astigmatism, you can correct with spherical gas permeable lenses without the complexity of going to a toric lens, Dr. Jones says.
Provide options to presbyopes. We lose a lot of people every year because historically there havent been a good majority of products to cover near and distance vision, says Lou Applebaum, senior product manager for Bausch & Lomb.
Although monovision is one option, Dr. Benoit says he would try to get the patient in a bifocal lens that meets their needs. It really comes down to what the patients primary goals are with contact lens wear, and we try to meet those goals.
A lot of people stopped wearing contacts because they had to wear reading glasses too, says Dr. Eiden.
Dr. Jones agrees. With a wide variety of RGP aspheric lenses and disposable presbyopic lenses [now available], we have a wealth of opportunity to keep presbyopic patients in contact lenses, he says. (For more on this, see Monovision vs. Multifocal: Which Would You Choose, December 2003.)
|
Practice Management Pearls for Recapturing Dropouts |
When it comes to recapturing contact lens dropouts, communication is key. Patients who have had problems in the past havent realized there are new ways to address them, says optometrist Glenda B. Secor.
S. Barry Eiden, O.D., agrees. In my mind, reclaiming lens dropouts all relates to proper education of patients in terms of contact lens technologies, he says. Thats why he stresses the importance of internal communication with his patients. This includes sending patients newsletters, posting information on your practices Web site and even in recall letters. Let patients know about new developments in contact lens materials.
Besides internal marketing, Dr. Eiden suggests targeting contact lens dropouts outside your patient base. Do this with direct mail and advertising.J.S.E. |
From a patients perspective, its sometimes easier to discontinue contact lens wear than to accept discomfort. But by careful evaluation and problem solving, you can keep these patients in contact lenses and youll recapture patients as well.
Associate Editor Michelle Boyles coordinated the case reports section of this report.
1 Keay LJ, et al. Symptoms experienced with high Dk 30N EW lens wear and their implications in patient discontinuation. Invest Ophthalmol Vis Sci 1999;40(S):S912.
2. Pritchard N. How can I avoid CL dropouts? Optician 2001 Nov 2;222(5825):14-8.
3. Lemp MA, Caffery B, Lebow K, et al. Omafilcon A (Proclear) soft contact lenses in a dry eye population. CLAO J 1999 Jan;25(1):40-7.
Vol. No: 141:04Issue:
4/15/04