Get a Head Start on Specialty Contact LensesIn the August 2024 issue of Review of Optometry—our 48th annual Contact Lens report—experts provide the tips and tools you need to start offering specialty lenses at your practice. In two more features, the authors deep-dive into soft lens optics and CL complications. Check out the other articles featured in this issue:
|
Soft contact lenses have certainly come a long way from the original HEMA materials of the 1950s based on Lim and Wichterle’s work.1 One of the biggest transformations we have seen is the variety of options now available in the optics of these lenses. Patients were once told they couldn’t wear contacts because of astigmatism and presbyopes were advised to rely on reading glasses. Today, soft lenses come in various add powers of center-distance and center-near designs, correct up to 6.00D of cylinder, use prism-ballasting methods and are even being recommended for pediatric myopia management.
Contact lenses are a cornerstone of many eyecare practices. Therefore, it is essential that patients’ needs are met with the lenses we prescribe to improve satisfaction and reduce risk of dropout. A major focus for patient lens satisfaction is comfort, influenced by issues with ocular surface dryness and the effect of contact lens wear on the tear film. Many new soft lens options feature improved wetting agents and lens surface treatments to satisfy this need.2
However, some patients are more likely to be dissatisfied with their vision in contact lenses than others; these can include presbyopes, patients with high or uncommon prescriptions and individuals with astigmatism. A good starting manifest refraction is an essential first step to ensure the best visual outcome in contact lenses. Vertex distance should also be considered, especially in cases of higher refractive errors. After an initial lens is selected and applied to the eye, the next essential part of lens evaluation is checking for centration.
Some patients, particularly those with large pupils, can experience symptoms of glare and ghosting in lower levels of light. Soft lens designs usually have around a 9mm optic zone, but if the lens decenters, this can affect visual quality even in single vision designs. Centration can be improved by adjusting the sagittal depth of the lens as a function of both base curve and diameter. One study has measured sagittal depth of various soft daily and monthly lenses, and these variables can be adjusted to improve fit and centration.3
Parameters are far more modifiable when entering the realm of custom lenses; in general, these are unique in that there is a wide range of powers, diameters and base curves available. These are chosen based on the material, keratometric values and horizontal visible iris diameter. This is particularly useful if the patient has a large corneal diameter. The optic zones can also be customized between 6mm and 12mm. Examples include but are not limited to Intelliwave (Art Optical), Revive (Bausch + Lomb), NaturaSoft (Advanced Vision Technologies), MetroSoft (Metro Optics) and SpecialEyes.4
A newer concept in soft lens optics, represented by products like MyDay and Biofinity Energys (CooperVision), is to help patients struggling with digital eye fatigue. One report found seven out of 10 patients have experienced symptoms of digital eye strain and about four out of 10 patients experience these symptoms multiple times a week. This may be a result of 79% of these patients spending over three hours per day on their smartphones. There are now single vision soft lenses using a +0.30D add, which is designed to help with eye strain.5 A report found eight out of 10 patients felt an improvement in eye tiredness with these lenses with nine out of 10 reporting clear vision.6
In the remainder of this article, let’s review the optics of modern toric and multifocal soft contact lenses and how each may affect visual performance and comfort of wear.
 |
|
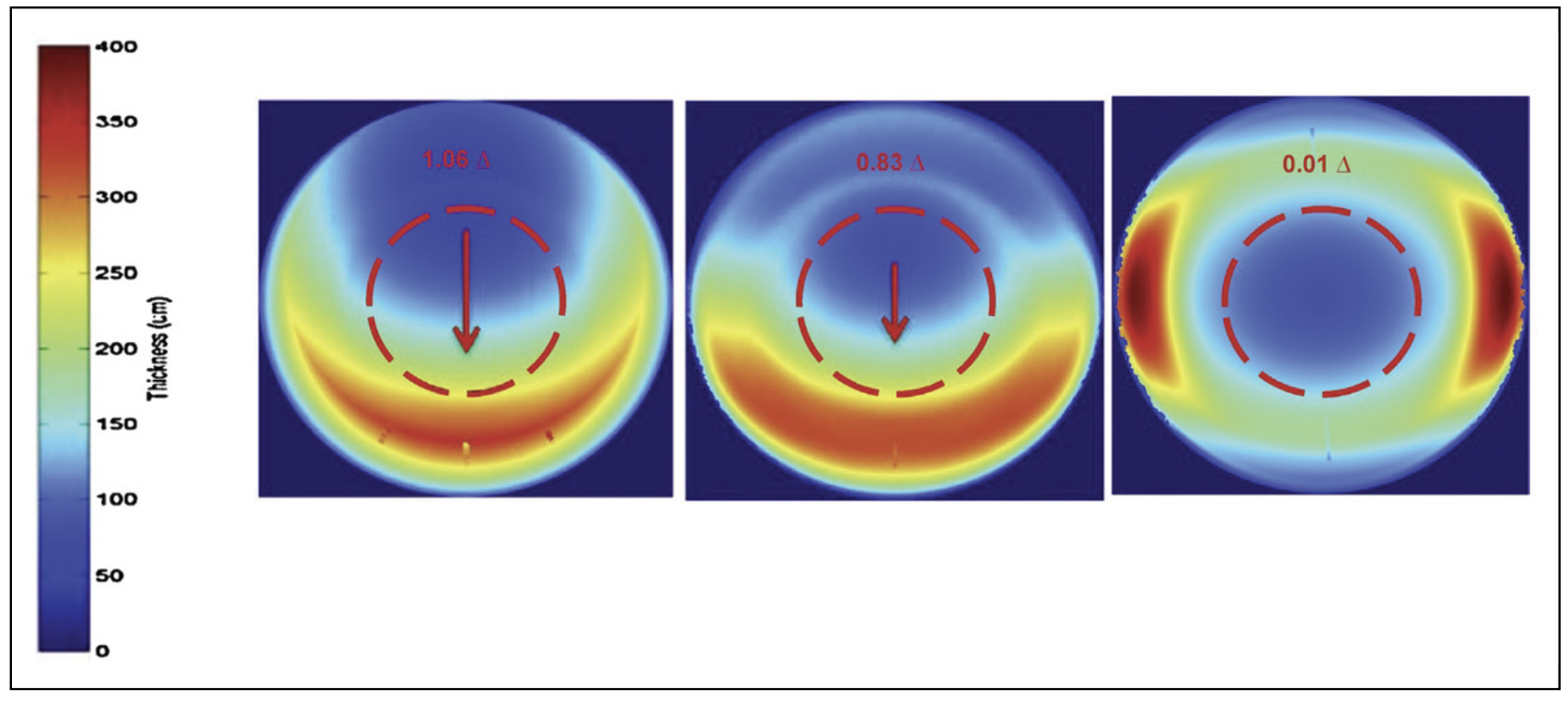
Fig. 1. Thickening of lens zones in three various types of toric stabilization: prism-ballast (left), peri-ballast (center), thin zone (right).7 Photo: Sulley A, et al. Click image to enlarge. |
Toric Lenses
There are now more soft lens designs than ever for the astigmatic patient, with daily disposable lens cylinder ranges up to 2.75D correction and monthly lens ranges up to 5.75D. Modern toric designs stabilize the lens on-eye through the options of prism-ballast, peri-ballast and thin zone designs (also referred to as double slab-off or dynamic stabilization). Peri-ballast designs such as the Biofinity Toric (CooperVision) and prism-ballast designs like Air Optix for Astigmatism (Alcon), both used in studies, are similar in that they both thin the superior portion of the lens to create a stabilization effect. The thin-zone design uses the thickness of the contact lens and four thinned zones of stability to create minimal thickness under the lids.
One study found a difference in the vertical prism measured in the optic zone of toric lenses with different stabilization methods. Figure 1 shows the three different designs with a map of the lens thickness in different zones. The prism-ballast technique on the left creates a denser thin zone superior with a thin zone of prism that extends from the inferior quadrant up along the lateral aspects of the lens. The study found these designs typically have the most vertical prism within the optic zone. The middle map is of the peri-ballast design. Here, the superior thinned zone is more spread out along the top half of the lens, while a thick area is condensed to the bottom. These designs had a moderate amount of optical prism with a mean value between 0.75 and 0.77 prism diopters between the two designs in the study. The final option on the right of Figure 1—the thin-zone design—showed little to no measurable prism within the optic zone with a mean value of 0.01 prism diopters.7
This optical prism data could be clinically impactful, especially when fitting toric lenses monocularly. Fitting a ballasted design in one eye could create vertical imbalance for a patient; studies have found that over 0.5 prism diopters of vertical disparity could cause symptoms of eye strain, visual discomfort, decreased stereopsis and even nausea and motion sickness in some patients.8-10 Labs that manufacture custom soft torics can also allow for customization in the amount of prism in the lens. Increasing this parameter can provide better stability of the cylinder correction.
 |
|
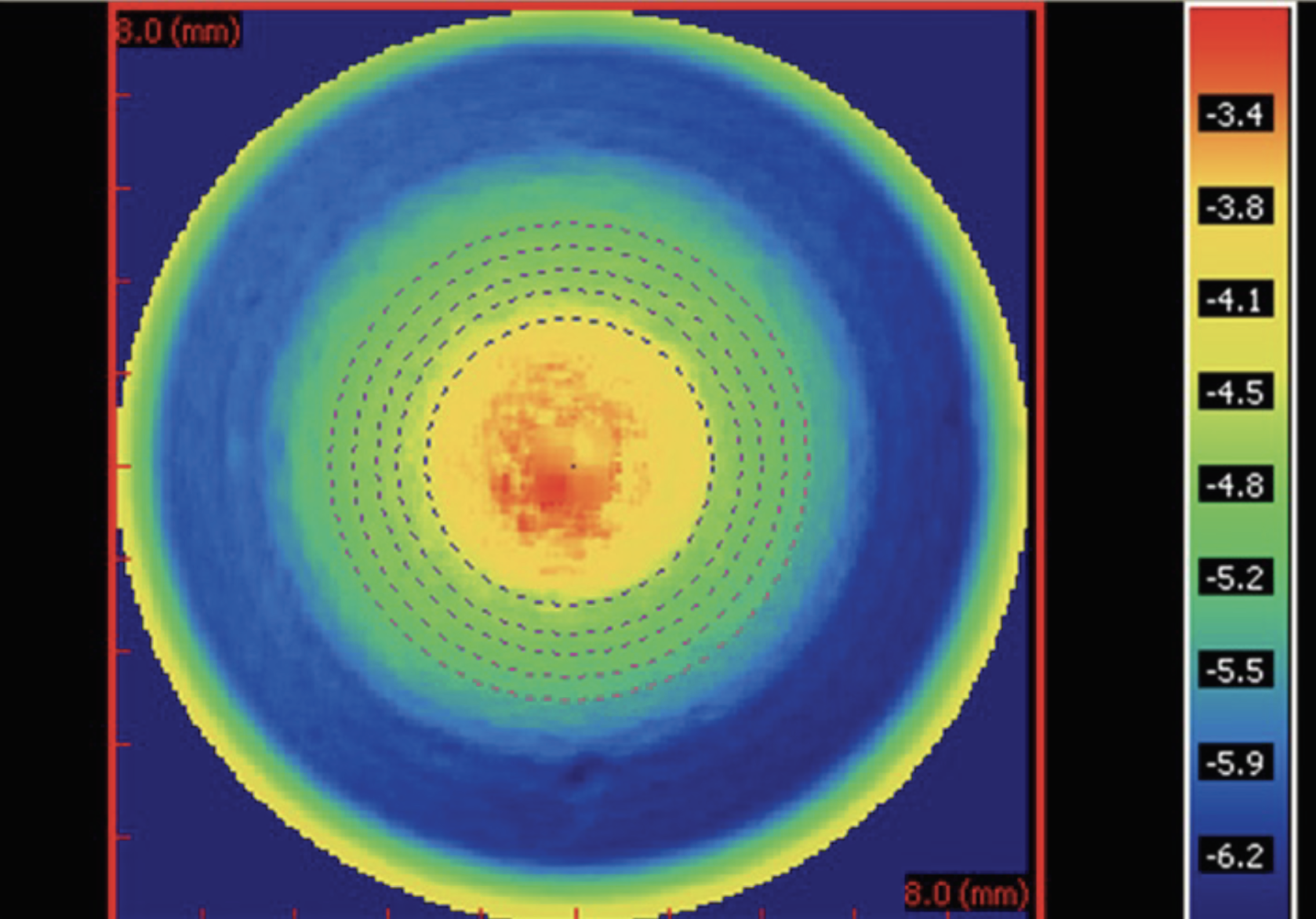
Fig. 2. A center-near soft multifocal lens with the power map measured by the NIMO TR1504.11 Click image to enlarge. |
Multifocals
Presbyopic patients have a plethora of soft lens options in daily, biweekly and monthly replacement modalities. Most use aspheric, center-near optics due to pupil constriction at near to deliver improved visual acuity up close. Fit guides vary across companies and designs, given the variance between multifocal lenses in add power, zone size and the rate at which this power changes across the zone. This has been demonstrated through instrumentation that can measure the power across the optic zone of different contact lenses. One such device, the NIMO TR1504 (Lambda-X), has demonstrated these design differences across multiple studies.
Figure 2 shows a center-near aspheric multifocal soft lens and where the near addition power is concentrated. In this figure, the outer blue zone represents the distance power, around -6.00D. There is then a progressive blending inward to generate the +2.50D add, the red color measuring -3.50D in the central zone. Here, it can be appreciated that the full add is reached across only about 2mm of the lens center. This is a fairly typical near-zone size across many multifocal designs.11
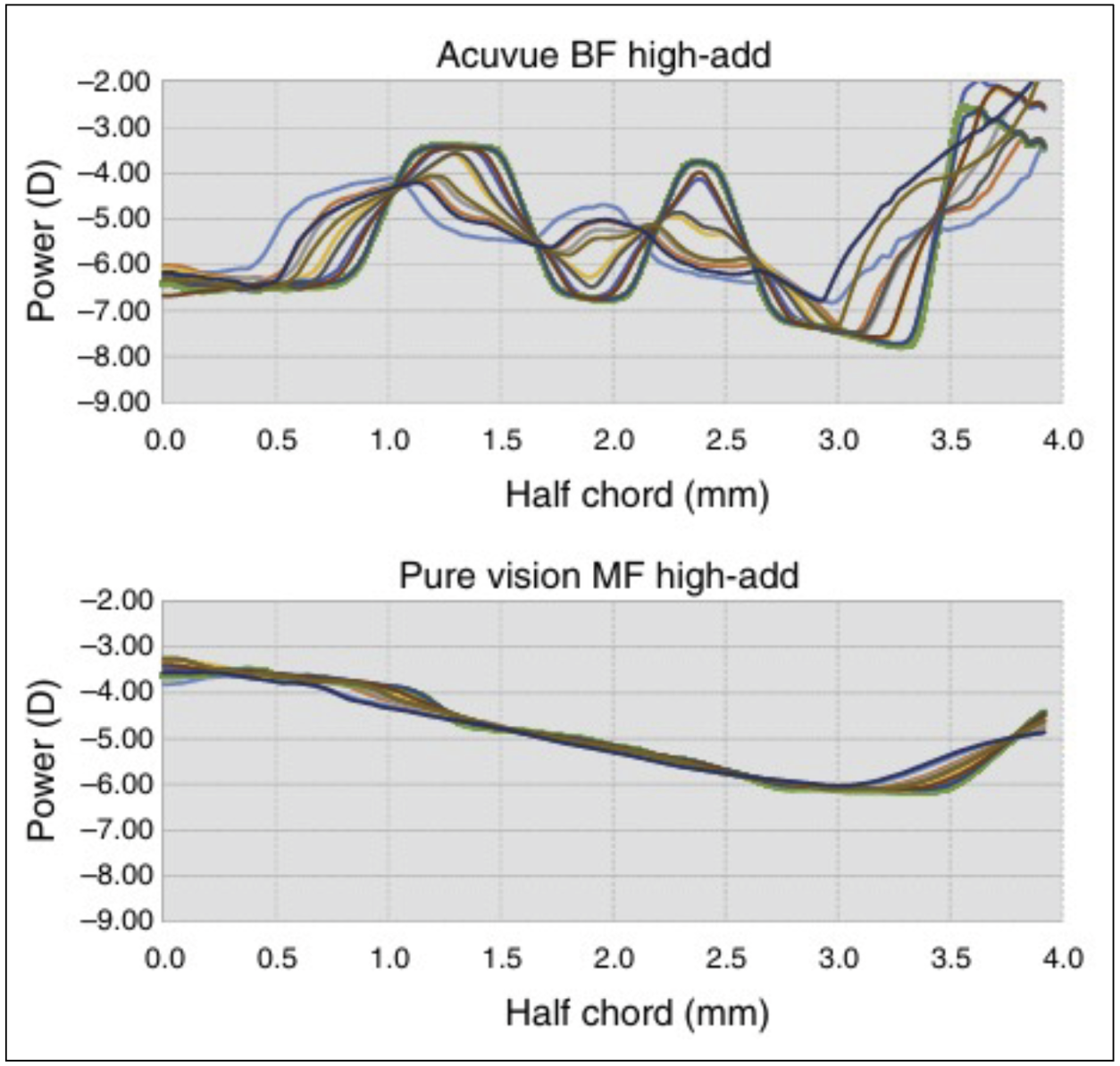
These power profiles can also be viewed graphically to show the measured power at different positions across the lens. The chord is a bisection of the center of the lens where the left side of the plot at 0mm is the geometric center of the lens. The graphs measure 4mm from the center to show the changing power across the multifocal’s profile.
 |
|
Fig. 3. The graphical profile of a concentric center-distance soft multifocal (top) compared with a center-near aspheric design (bottom). This graphs the power across the lens from the center out to the edge of the optic zone. Photo: Kim E, et al. Click image to enlarge. |
Figure 3 shows the contrast between a concentric design and a center-near aspheric. The top graph shows greater fluctuation of power where the central zone is the distance power of -6.00D. Repeated measurements show the change of the power, consistently reaching up to -3.50D because of the +2.50D addition to then change back to the distance power as it changes between the rings until reaching the edge of the optic zone. The bottom graph shows the add power is reached in the center of the lens, starting at -3.50D, which then smoothly blends out to 2.5mm to 3.0mm, where the lens achieves a distance power of -6.00D.
Studies like this underscore the importance of zone size and show how multifocal optics are some of the most susceptible to lens decentration. Due to the power changing across different zones, a lens that is not centered over the visual axis will have issues providing the desired visual outcome.11
Power profiles such as those in Figure 3 can show how large distance or near zones are and the transition between them. This information is useful when accounting for the patient’s pupil size, visual demands and illumination of their typical environment. A patient with smaller pupils may have more difficulty at distance if the multifocal design has a large center-near addition zone. This optic may also be problematic for a patient more concerned about their distance vision, such as a truck driver. Conversely, a multifocal with a smaller center-near zone may make it more difficult for patients to see up close if they have particularly large pupils or critical near-vision demands, such as reading medicine bottles in a pharmacy.12
Due to the complexity of multifocal optics and each patient’s unique visual demands, these designs can sometimes be viewed as challenging fits. When providers encounter suboptimal visual performance after following the manufacturer’s fitting guide recommendations, the lens centration should be critically reexamined and pupil size considered.
Custom soft multifocal designs have an advantage of variable base curves and diameters to improve centration. Many also allow the customization of center-distance or center-near zones along with zone size flexibility. This can be extremely helpful during troubleshooting. Even beyond this is the ability for some designs to incorporate decentered optics. By measuring the amount of the central zone’s decentration from the middle of the pupil, some designs can move the optics of the contact lens back into alignment with the visual axis. This process is often aided through topography. After adjusting the topography scale and narrowing it, one can measure the decentration and axis by clicking in the center of the optic—red color for center-near and blue color for center-distance.13
An alternative option in simultaneous vision now exists in the form of extended depth-of-focus (EDOF) optics, such as those in NaturalVue contact lenses (Visioneering Technologies). These power profiles use an aperiodic, non-harmonic change in power. As a result, they are less influenced by pupil size and lens decentration. The EDOF power profile creates an optical “pinhole effect,” thereby allowing a range of clear vision rather than one or two focal points.14
 |
|
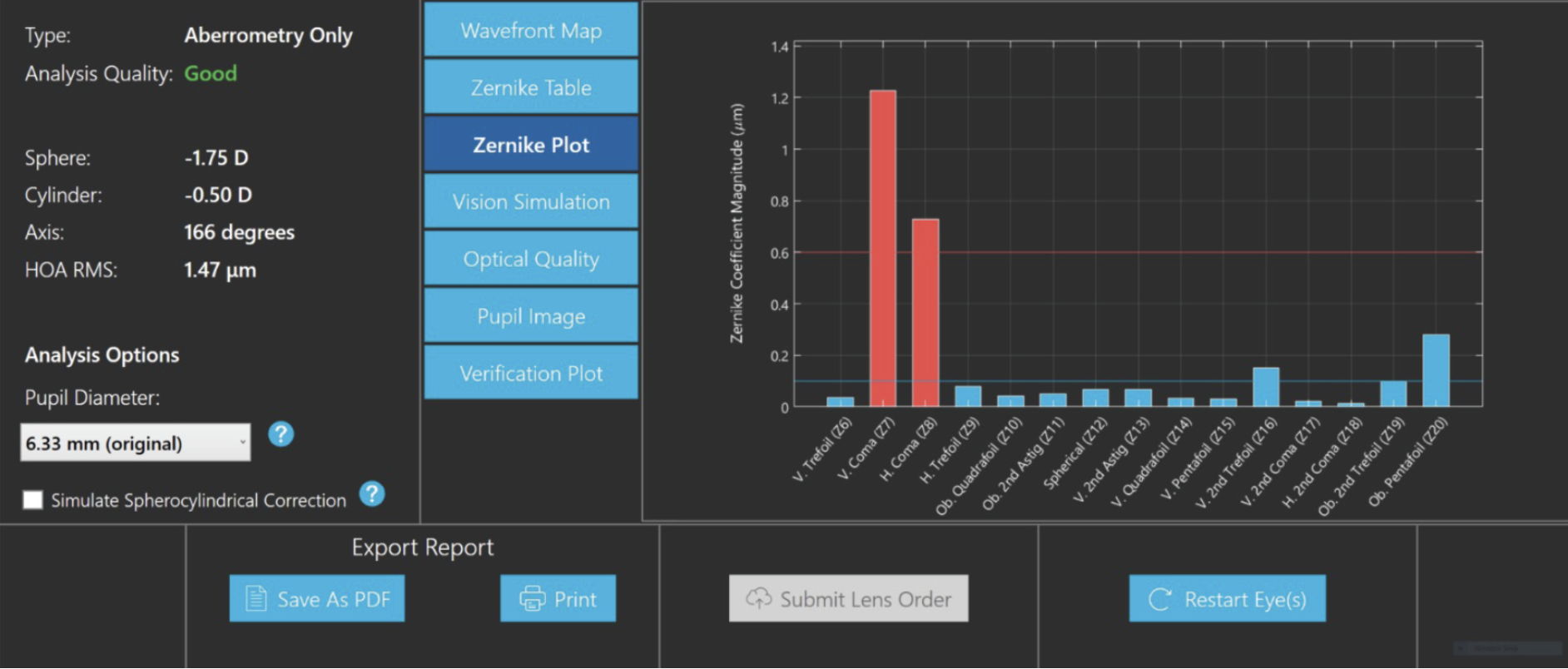
Fig. 4. The Zernike plot, highlighting visually disturbing coma. This Xwave aberrometer (Ovitz) can send the data to labs for custom lens manufacturing to correct higher-order aberrations.15 Photo: Ovitz. Click image to enlarge. |
The Future of Optics
With so many improved contact lens designs over the years, it is apparent that competition breeds innovation. Patients no longer need to hear, “Contacts won’t work for you because of your astigmatism,” and many are given the opportunity to try multifocal lenses instead of resorting to monovision or over-spectacles.
Given the wide array of viable soft lens options on the market now, what’s next? How can things possibly get better? Soft contact lenses may start to see a shift in private practices into a more customized route. Consumers seem to respond positively to things made “just for them,” which can be illustrated through the “Starbucks model.” Services and businesses like this popular coffee chain provide a custom product or experience for that individual (in the case of Starbucks, each customer’s order is named after them).
If a patient has unmet visual needs within your practice, consider the expanding options of custom soft lens designs, particularly for highly astigmatic individuals and presbyopes. There may even be a breakthrough in optical innovations like what is occurring in the scleral lens space with higher-order aberration correction. There are now instruments that can measure visual problems like trefoil and coma to send to a lab for optical customization with that lens (Figure 4). The measurement even accounts for lens decentration and rotation.15
Takeaways
A rewarding challenge of eyecare is delivering the best possible outcomes to our patients. Thankfully, there are many great tools for providing the best visual experience in soft contact lenses for our patients. Consideration of ballasting and prism can help stabilize toric lenses, and remembering to evaluate pupil size and lens centration can improve multifocal performance for presbyopes.
Dr. Gidosh is an associate professor at Pennsylvania College of Optometry (PCO). He serves as chief of the Cornea and Contact Lens Service at The Eye Institute and has presented lectures and workshops in PCO’s Advanced Studies Program and International Program on topics including scleral and hybrid lenses, irregular corneas and contact lens fitting. He is a fellow of the American Academy of Optometry and has served as a clinical investigator for studies involving hybrid, scleral, multifocal and orthokeratology lenses, presenting lectures and posters at national and international conferences on these topics.
1. McMahon T, Zadnik K. Twenty-five years of contact lenses. Cornea. 2000;19(5):730-40. 2. Kim E, Bakaraju RC, Ehrmann K. Reliability of power profiles measured on NIMO TR1504 (Lambda-X) and effects of lens decentration for single vision, bifocal and multifocal contact lenses. J Optom. 2016;9(2):126-36. 3. Kajita M, Muraoka T, Orsborn G. Changes in accommodative micro-fluctuations after wearing contact lenses of different optical designs. Cont Lens Anterior Eye. 2020;43(5):493-6. 4. CooperVision. A new look at digital eye strain. Published February 2024. coopervision.com/sites/coopervision.com/files/media-document/digital-eye-strain-research-report_1.pdf. Accessed June 20, 2024. 5. Davis RL, Schwartz M. Seeing multifocal optics more clearly. Review of Cornea & Contact Lenses. May/June 2021;16-20. 6. van der Worp E, Lampa M, Kinoshita B. Variation in sag values in daily disposable, reusable and toric soft contact lenses. Cont Lens Anterior Eye. 2021;4(6):101386. 7. Art Optical. Fast focus, fine tuned custom soft contact lens for all prescriptions. Published 2023. artoptical.com/products/intelliwavepro. Accessed June 20, 2024. 8. Sulley A, Hawke R, Lorenz KO, Toubouti Y, Olivares G. Resultant vertical prism in toric soft contact lenses. Cont Lens Anterior Eye. 2015;38(4):253-7. 9. du Toit R, Ramke J, Brian G. Tolerance to prism induced by ready-made spectacles: setting and using a standard. Optom Vis Sci. 2007;84(11):1053-9. 10. Jackson DN, Bedell HD. Vertical heterophoria and susceptibility to visually induced motion sickness. Strabismus. 2012;20(1):17-23. 11. Momeni-Moghaddam H, Eperjesi F, Kundart J, Sabbaghi H. Induced vertical disparity effects on local and global stereopsis. Curr Eye Res. 2014;39(4):411-5. 12. Kim E, Bakaraju RC, Ehrmann K. Reliability of power profiles measured on NIMO TR1504 (Lambda-X) and effects of lens decentration for single vision, bifocal and multifocal contact lenses. J Optom. 2016;9(2):126-36. 13. Stokkermans T, Gidosh N. GP multifocal contact lenses: the 2024 lineup. Review of Cornea & Contact Lenses. January/February 2024;16-23. 14. SpecialEyes. Study results: multifocal contact lenses with offset optics. Published July 3, 2018. blog.specialeyesqc.com/multifocal-contacts-offset-optics-study. Accessed June 20, 2024. 15. Ovitz. Xwave system: higher-order aberration correction taken to a new level. www.ovitz.us/xwave-system. Accessed June 20, 2024. |

