Older keratoconus patients have not been as lucky as their younger counterparts, who can get good stabilization earlier in the disease course from a corneal crosslinking (CXL) procedure. However, researchers are suggesting that these patients may benefit from dual treatment of topography-guided PRK and CXL as a means of offering visual rehabilitation, as one new study finds.
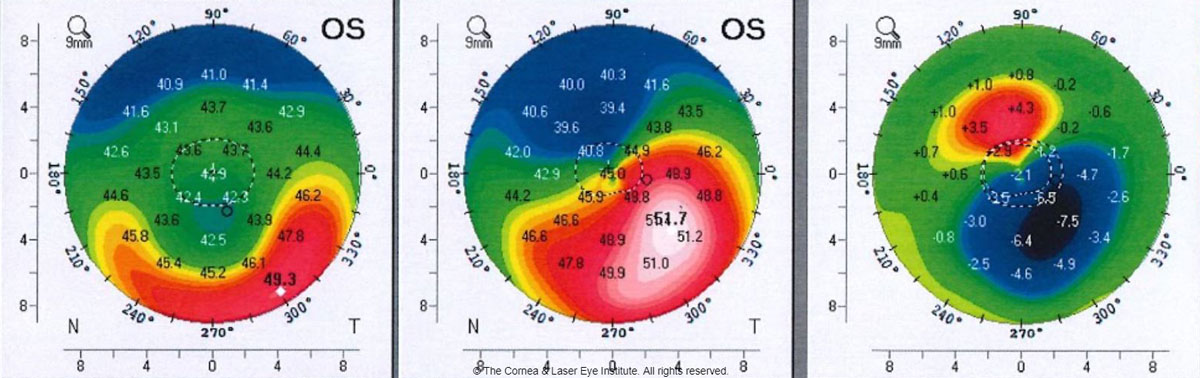 |
| Even stable patients with stiffer corneas experienced a marked improvement in visual outcomes and corneal regularization after combined use of both procedures. Photo: John Gelles, OD. Click image to enlarge. |
A comparative analysis was conducted for the combined procedure in categories of visual, refractive and tomographic outcomes in stable vs. progressive keratoconic patients. The retrospective, case-control investigation included 101 total eyes from 93 patients who all underwent simultaneous topo-guided PRK and CXL. Minimum follow-up was 12 months and extended up to three years. Using predefined disease progression criteria, 62 eyes were considered progressive and 39 stable.
The study researchers found all baseline characteristics were similar between both groups except for age at surgery, which was over a decade greater in stable eyes (23.4±4.2 years progressive; 36.0±9.1 years stable). Corrected distance visual acuity improved in both groups with no differences. Similarly, both groups experienced decreased maximum keratometry with no differences seen between them. Other tomographic outcomes were also similar between groups, and pachymetry decreased after surgery but remained stable throughout the follow-up.
In their paper for the journal, the authors elaborate on their findings by explaining that the combined treatments lead to corneal regularization and significant visual improvements in both patient subsets. As they explain, “this brings breakthrough evidence to expand our current indications for CXL, allowing for older patients to benefit from the visual rehabilitation of TG-PRK.”
The current role of CXL has been in arresting disease progression rather than being used as a tool for visual improvement, since CXL increases corneal rigidity, which paradoxically preserves the ectatic irregular corneal shape induced by keratoconus despite the overall flattening induced. However, topo-guided PRK shows more favorable visual and refractive outcomes in irregular corneas. As such, the combination of both addresses the problem of structural weakness of keratoconus while regularizing and reshaping the cornea. The investigators are hopeful that “this strategy can improve the visual outcomes of CXL in those patients that need it to arrest disease progression but, potentially, also expand the indications of CXL to include those patients that are not progressing but need visual rehabilitation.”
The authors also mentioned that the progressive cases expected to be significantly younger, but visual, refractive and tomographic outcomes across all metrics in both groups were similar up to three years. Spherical equivalent was different at the first postoperative year between the groups, but this was not seen upon follow-up.
Looking forward clinically, they believe that “overall, these results show that the Athens protocol has been gaining in the management of progressive keratoconus is also promisingly valid for older stable patients, which paves the way for an update in our treatment protocols.”
Gil P, Gil JQ, Dias M, et al. Comparative analysis of combined topography-guided photorefractive keratectomy and corneal crosslinking in progressive vs. stable keratoconus. Cornea. July 31, 2024. [Epub ahead of print]. |


