Although anti-VEGF and steroid treatments may lead to the improvement of macular edema in patients who experience central retinal vein occlusion (CRVO), the associated retinal damage may not fully recover—or at least there is a lack of longitudinal studies to turn to. Recently, researchers in South Korea explored longitudinal changes in the thickness of each retinal layer in CRVO patients with resolved macula edema. They found that even after edema resolution, the ganglion cell complex (GCC), inner nuclear layer (INL), outer plexiform layer and outer nuclear layer (ONL) continued to thin over a three-year period, indicating persistent retinal damage. Also, changes in the thicknesses of the GCC, outer plexiform layer and ONL were significantly associated with visual acuity. After the three-year follow-up, the GCC still exhibited continued thinning, which could suggest that changes there have the greatest long-term effects on visual acuity.
 |
|
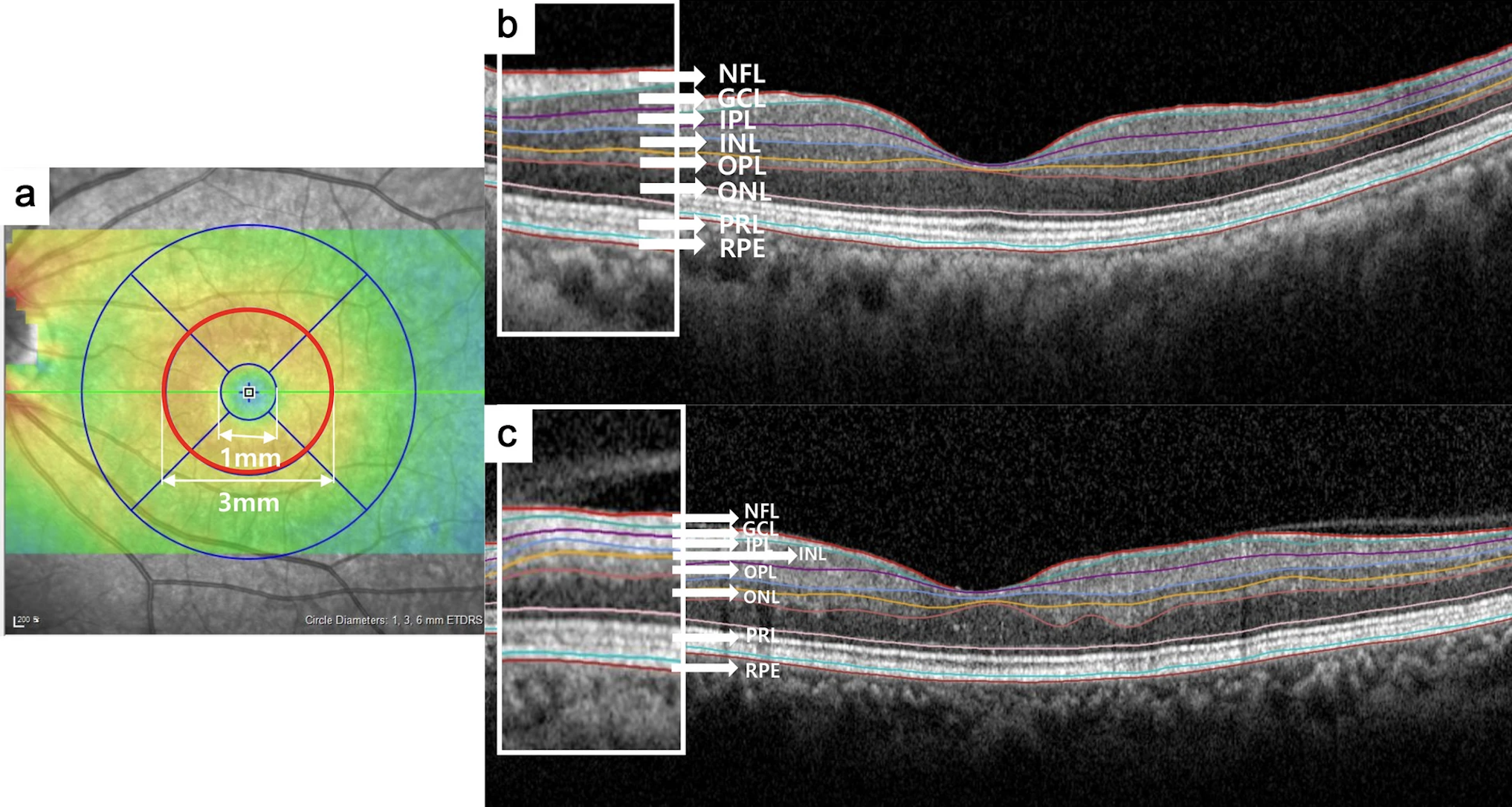
Changes in the GCC, outer plexiform layer and ONL also were significantly associated with BCVA; these relationships have not been previously reported. This image from the study shows: (a) the parafoveal area (red circle) ranging from 1mm to 3mm from the subfoveal region, that was analyzed, (b) a representative B-scan image of the control group and (c) and the CRVO group. Photo: Lee MW, et al. Eye Vis (Lond). 2024;11(1):29. Click image to enlarge. |
This retrospective observational study, which was published in Eye and Vision, enrolled 98 eyes: 50 for the control group and 48 for the CRVO group. Each retinal layer thickness of the parafoveal area, including GCC, INL, outer plexiform layer, ONL, photoreceptor layer and retinal pigment epithelium (RPE), was measured. After the resolution of macular edema, three more examinations with a one-year interval were analyzed. The baseline GCC thickness was 114.2μm and 104.2μm in the control and CRVO groups, respectively, which was significantly different. Because of its high vascularity, the study authors expected GCC to rapidly respond to anti-VEGF treatment, exhibiting drastic changes in thickness.
The reduction rate of GCC, INL, outer plexiform layer and ONL was -3.92μm/year, -1.33μm/year, -0.91μm/year and -2.31μm/year, respectively, in the CRVO group, whereas no significant reductions were observed in the control group. Best-corrected visual acuity was significantly associated with changes in the GCC, outer plexiform layer and ONL in the CRVO group. The photoreceptor layer and RPE, which receive a portion of their oxygen supply from the choroid, did not exhibit significant differences between the two groups or changes over time.
“These results indicate that the continuous thinning of each retinal layer due to sustained damage by CRVO, despite macular edema resolution, may adversely affect visual function,” the researchers wrote in their paper.
“These findings should be considered when assessing retinal thickness changes in CRVO patients,” they added.
Lee MW, Jun JH, Seong HJ. Longitudinal changes in each retinal layer thickness in patients with non‑ischemic central retinal vein occlusion. Eye Vis (Lond). 2024;11(1):29. |


