 |
|
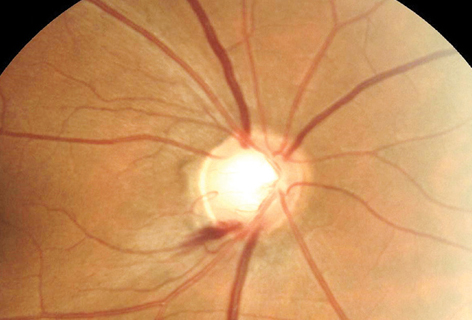
Office-based BP measurements cannot sufficiently and accurately predict individuals with the lowest BP values identified using 24-hour BP recording, leading the study authors to argue for its use in patients at risk of glaucoma progression, particularly those who demonstrate optic disc hemorrhage. Photo: Michael Chaglasian, OD. Click image to enlarge. |
Although intraocular pressure (IOP) is the most important modifiable characteristic in glaucoma development and advancement, the condition can still exist in those with IOPs within a “normal” range, suggesting mechanisms not dependent on IOP to also affect optic nerve injury. As is suggested, these may include impaired optic nerve perfusion due to impaired blood flow autoregulation which may be exacerbated by systemic arterial hypotension.
Consequently, researchers wanted to examine the relationship between systemic arterial blood pressure and the rate of change in standard automated perimetry (SAP) in glaucomatous eyes and glaucoma suspects. The prospective study, published in Ophthalmology, included 124 eyes (91glaucoma; 33 suspects) of 64 patients at the Bascom Palmer Eye Institute; mean age of patients was 68.4±7.6 years.
All included underwent ophthalmic examination, blood pressure (BP) measurement and SAP at four-month intervals. Baseline ambulatory BP monitoring (ABPM) was acquired and the effect of BP on rates of SAP mean deviation change over time was looked at after adjusting for factors of inclusion of both eyes, age, sex, race, IOP, baseline severity and central corneal thickness.
On average, eyes had 8.9 ±1.5 SAP exams over 28.3 ±6.0 months of follow-up. Median mean deviation change rate was 0.14dB/year with 7%, or nine eyes, presenting moderate to fast progression, defined as mean deviation change ≤-0.50dB/year. Each 10mm HG lower in 24-hour average mean arterial pressure and systolic BP were linked with -0.17dB/year and -0.14dB/year faster rates of mean deviation loss. Mean deviation loss was also associated with lower mean systolic BP during follow-up.
In their paper, the researchers discussed how these findings might benefit certain patients. As they explain, “we can speculate that glaucomatous eyes with progression at low IOP levels may have a non-IOP dependent mechanism of disease progression and thus would benefit from 24-hour ABPM to determine if they have vascular risk factors for progression such as low mean arterial pressure or systolic BP.”
They continue that “eyes with optic disc hemorrhage may also benefit from adjunctive 24-hour ABPM monitoring. Finally, patients with a history of low systemic BP, or those in whom an office-based BP reading demonstrates low BP, may benefit from such testing given the risk for future fast progression.”
Therapeutically, the investigators posit: “Based on our data, one may speculate that certain glaucoma patients, for example those with or at high risk for visual field progression, may be identified with 24-hour BP monitoring with systemic hypotension while using systemic arterial hypertension medication.”
Donkor R, Jammal AA, Greenfield DS. Relationship between blood pressure and rates of glaucomatous visual field progression: The Vascular Imaging in Glaucoma Study. Ophthalmology. August 5, 2024. [Epub ahead of print]. |


