 |
|
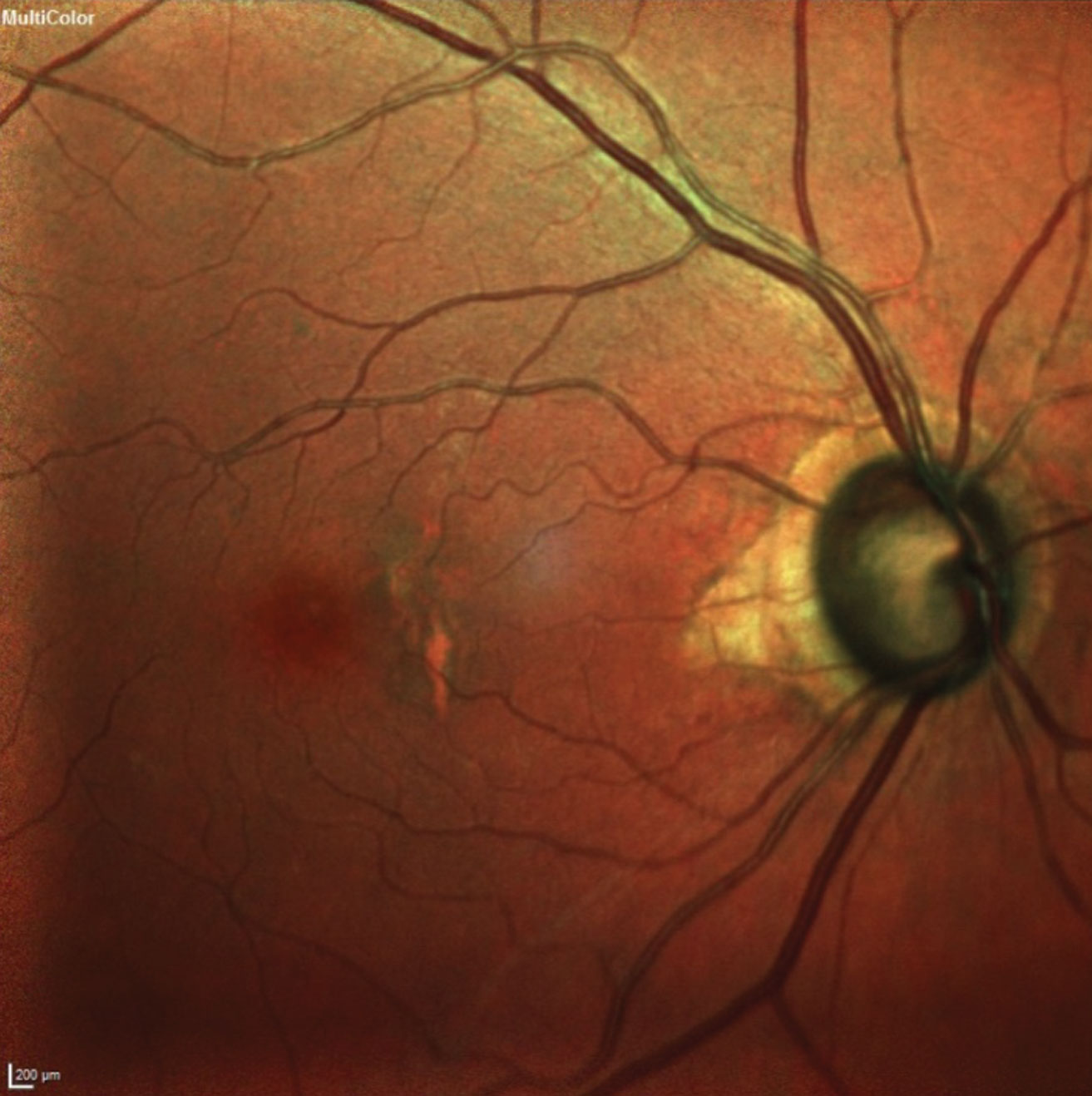
The researchers concluded that "combining canaloplasty with cataract surgery does not compromise the efficacy or safety of the former and might provide a higher absolute IOP reduction and reduced medication burden." Photo: James L. Fanelli, OD. Click image to enlarge. |
Most studies of canaloplasty efficacy limit their follow-up periods to a few years. Recently, researchers from Germany published results with a 10-year follow-up to better understand the course of IOP in such patients over the years, including reduction of glaucoma medication use and the complications that may have arisen in with canaloplasty patients with or without simultaneous cataract surgery.
For this study, glaucoma patients visited a single outpatient clinic and were treated between 2007 and 2013. A total of 50 eyes (35 subjects) underwent canaloplasty with or without phacoemulsification during this timeframe, but one subject was eliminated from the study as they needed a canal expander due to failed catheterization. The remaining subjects were split into two groups: Group A (n=28 eyes) represented canaloplasty and Group B (n=20 eyes) represented phacocanaloplasty procedures.
Researchers examined subjects at one, four, seven and 10-year follow-up periods. When analzying IOP trends, the mean measurements at each time period were lower than baseline for both groups. Group A’s mean IOP was 22mm Hg measured at baseline. This decreased to 14mm Hg at one year, then gradually elevated over the remainder of the study period: 14.3mm Hg at four years, 14.4mm Hg at seven years and 16.5mm Hg at 10 years. Additionally, Group B’s mean IOP was 24.5mm Hg measured at baseline. This dropped to 13.8mm Hg at one year and then followed a similar course: 14.9mm Hg at four years, 15.3mm Hg at seven years and 14.8mm Hg at 10 years.
The team defined “complete success” from the intervention to be IOP ≥18mm Hg and found the following rates at each time period:
| Canaloplasty (Group A) | Phacocanaloplasty (Group B) |
1 year | 89.3% | 94.1% |
4 years | 68.1% | 86.7% |
7 years | 50.0% | 82.3% |
10 years | 41.7% | 66.7% |
Researchers noted that the mean number of glaucoma medications also dropped for patients and remained below baseline even out to 10 years, with better control in the phacocanaloplasty group, as follows:
| Canaloplasty (Group A) | Phacocanaloplasty (Group B) |
Baseline | 1.5 | 2.2 |
1 year | 0.1 | 0 |
4 years | 0.3 | 0.1 |
7 years | 0.6 | 0.1 |
10 years | 0.9 | 0.5 |
“Postoperative complications were generally mild and self-limited,” noted the researchers in their study. “Compared to Group B, Group A exhibited a higher incidence of both hyphema and microhyphema, as well as a greater occurrence of transient hypotony.” The researchers suspect that viscoelastic use during cataract surgery “may contribute to this outcome by temporarily reducing trabecular outflow and impeding blood inflow from Schlemm’s canal.” Additionally, transient hypotony was detected in both groups. Group A had a case of cheese wiring, but it did not need intervention, and another case of clinically significant bleb without globe hypotony, which also did not require treatment.
“Our study shows that combining canaloplasty with cataract surgery does not compromise the efficacy or safety of the former and might provide a higher absolute IOP reduction and reduced medication burden,” concluded the researchers in their paper. “Further prospective, randomized trials are needed to fully explore the long-term outcomes of both procedures.”
Ennerst CD, Fischinger IR, Tetz MR. Long-term outcome after canaloplasty and phacocanaloplasty in primary open-angle glaucoma. Journal of Glaucoma. August 5, 2024. [Epub ahead of print]. |


