 |
|
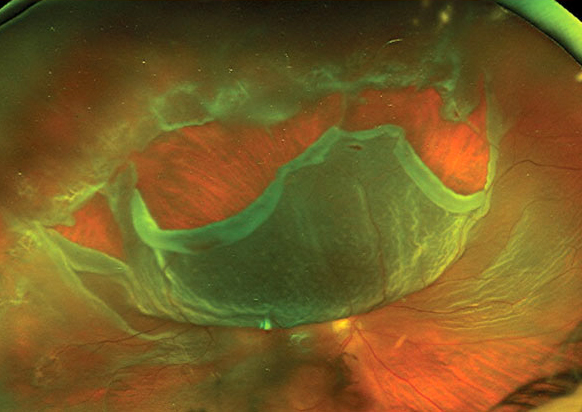
A recent study outlined how both individual and neighborhood-level risk factors may ultimately influence the presentation of RRD. Photo: Mohammad Rafieetary, OD. Click image to enlarge. |
Social determinants of health (SDOH) are now recognized as important contributors to vision outcomes in several eye diseases, including glaucoma, diabetic retinopathy, AMD and cataracts, but have yet to be thoroughly explored in rhegmatogenous retinal detachment (RRD). The identification and resolution of barriers to early RRD repair are likely to improve functional outcomes.
A study published yesterday in JAMA Ophthalmology evaluated the association between neighborhood-level SDOH and baseline severity (visual acuity and foveal status) of RRD. Results of this cohort study suggested that patients with a residence in neighborhoods with greater socioeconomic deprivation or a higher percentage of workers who drive to work were more likely to present with more severe RRD even after accounting for multiple individual-level characteristics.1
The retrospective cohort study included 700 adult patients 18 years old and older who underwent primary repair of uncomplicated RRD at the Wilmer Eye Institute at Johns Hopkins School of Medicine in Baltimore. Mean age was 57.9 and 61.7% were men.
The researchers found associations between adverse neighborhood-level SDOH and the severity of the initial presentation among patients with RRD. Patients who resided in neighborhoods with more socioeconomic deprivation (with higher Area Deprivation Index percentile rank and lower per capita income) had greater odds of presenting with visual acuity worse than 20/40 or fovea-involving RRD, even after accounting for multiple individual-level characteristics including age, sex, race and ethnicity and insurance.
Likewise, patients from neighborhoods where a higher percentage of people drive to work had greater odds of presenting with more severe RRD. The researchers postulate that patients without cars who live in neighborhoods where cars are necessary for work might have difficulty accessing health care and thus present later in the context of RRD.
At the individual level, the team found that non-Hispanic Black patients and those with public insurance had worse visual acuity and fovea-involving RRD, whereas older patients and those without medical insurance had worse visual acuity. Sex was not associated with either visual acuity or foveal status at baseline.
“Findings from this study might help highlight neighborhoods that will benefit from policy changes and interventions that promote earlier presentation with RRD,” the study authors wrote in their paper. “Ultimately, interventions targeting these vulnerable populations may lead to earlier surgical repair, improved functional outcomes, reduced complication rates and reduced health care spending.”1
A commentary also published in JAMA Ophthalmology surmised that “delays between these different steps in the [RRD] care process are likely influenced by each person’s social risk factors, ultimately leading people with worse social risk factors to present to the retina surgeon with worse vision.”2 This research adds to the body of evidence linking socioeconomic hindrances with one’s inability to access routine preventative care, which often manifests as worst baseline status at presentation.
“RRD is an eye condition that requires a timely surgical intervention by a retina surgeon for optimal outcomes,” the commentary authors wrote. “Accessing such a specialist represents a complex journey through the medical system for all patients.”
Discussing why an increase in the neighborhood-level percentage of workers who drive to work was associated with an increased odds of presenting with RRDs with worse visual acuity, they suggested that, perhaps in neighborhoods where a high percentage of people drive to work, these individuals are farther from or lack access to reliable public transit.” Recognizing the limitations placed by real-world circumstances could help policymakers develop efforts to improve access.
“There are new insights to be gained by assessing both patient-level and neighborhood-level interactions separately and together via interaction effects, the commentary noted. “We will see more complex insights into eye and vision health disparities, which can then inform more nuanced policies to address these problems.”2
1. Ong SS, Tran D, Westlund E, et al. Neighborhood-level social determinants of health and presenting characteristics for rhegmatogenous retinal detachments. JAMA Ophthalmol. August 8, 2024. [Epub ahead of print]. 2. Hicks PM, Woodward MA, Newman-Casey PA. Implications of neighborhood- and patient-level factors for eye care. JAMA Ophthalmol. August 8, 2024. [Epub ahead of print]. |


