 |
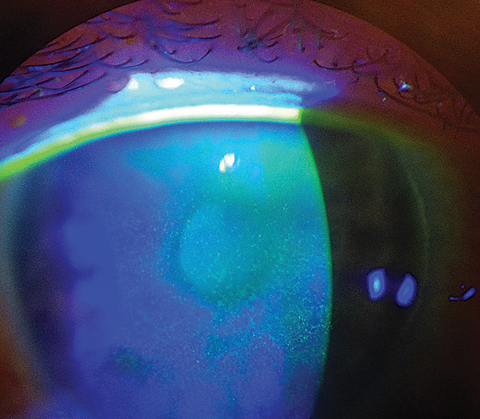
| A recent analysis of dry eye clinical signs in the DREAM cohort has suggested that it is valuable to consider each eye separately in the design and statistical analysis for dry eye studies, as well as in a clinical setting when considering treatment strategies. Photo: Scott G. Hauswirth, OD. Click image to enlarge. |
As it stands, there remains a lack of understanding on the intereye agreement of commonly used sign measures in individuals with dry eye disease (DED). Through secondary analyses of data from a large cohort of participants in the Dry Eye Assessment and Management (DREAM) study, the DREAM Study Research Group evaluated intereye agreement in DED signs to track the worse eye of each dry eye sign over a one-year follow-up period. They found moderate-to-good intereye agreement, with tear osmolarity having the worst agreement and corneal staining and Schirmer test scores having the best. Nevertheless, they found the eye with the worse dry eye sign switched from one eye to the other over time in more than one-third of DREAM participants. Their findings suggest considering signs from both eyes in future DED trials.
“The optimal analysis for the dry eye signs thus should include data from both eyes and account for the intereye correlation,” they wrote in their paper, which was published in Cornea.
Using unique data from the large cohort of DREAM participants, the study group evaluated the intereye agreement of six commonly used clinical sign measures for dry-eye disease: corneal fluorescein staining, conjunctival lissamine green staining, tear film break-up time (TBUT), anesthetized Schirmer test, tear osmolarity and meibomian gland dysfunction (MGD). Each was measured at baseline, three, six and 12 months.
DED signs had moderate-to-good intereye agreement with an intraclass correlation coefficient ranging from 0.45 (tear osmolarity) to 0.81 (corneal staining and Schirmer test) and a weighted kappa ranging from 0.58 (plugging) to 0.69 (lid secretion). The percentage of participants exceeding the threshold absolute intereye difference was 15% to 20% for conjunctival staining, 11% to 15% for TBUT, 17% to 21% for MGD, 13% to 18% for corneal staining, 21% to 23% for Schirmer test and 44% to 47% for osmolarity. The eye with a worse DED sign ranged between 36% (TBUT) and 80% (osmolarity) of participants.
“While tear osmolarity had the highest proportion of participants (47%) demonstrating a clinically significant absolute intereye difference at baseline, about 20% of participants also demonstrated clinically significant differences for conjunctival staining score, Schirmer test and MGD, indicating that these three dry-eye signs could potentially serve as useful indicators for diagnosing DED,” the research group suggested.
Zhong A, Augello P, Asbell P, Ying GS; the Dream Study Research Group. Intereye agreement in dry-eye signs in the DREAM Study: implications for future dry-eye trials. Cornea. July 30, 2024. [Epub ahead of print]. |


