 |
|
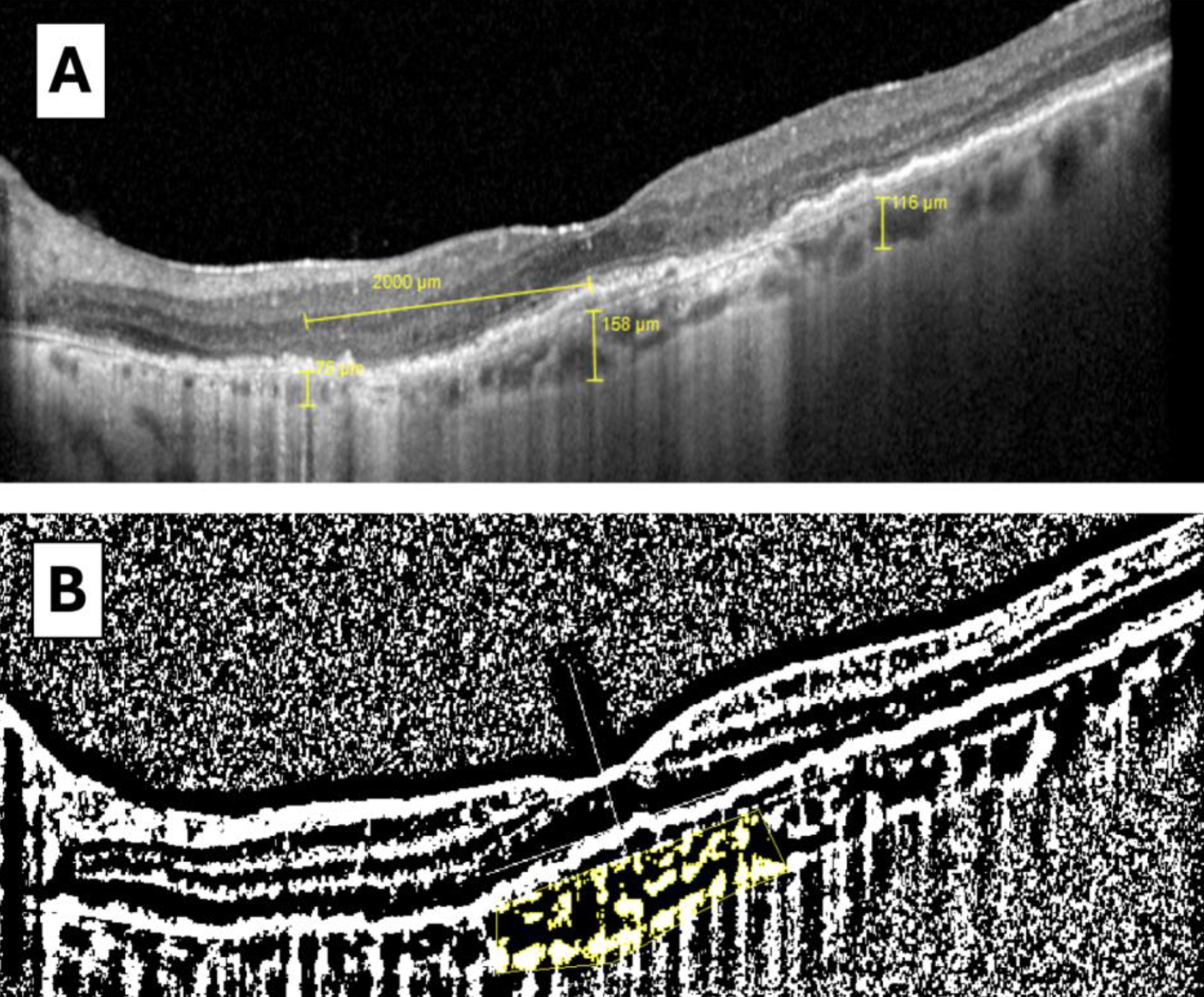
Choroidal thickness and choroidal vascularity index (CVI) measurements on OCT may help further stratify the risk of progression in AMD, a new study finds. Its results showed that more rapid changes in choroidal thickness and CVI over time may indicate a higher risk for geographic atrophy development. These images from the study show (A) choroidal thickness measurement at three different points of the macular area) and (B) calculation of subfoveal CVI from a binarized image, with the dark pixels representing the vessels’ luminal area and the white pixels the stromal area. Total luminal area divided by total choroidal area represents the CVI, a measure of the structure’s vascular capacity. Photo: Vidal-Oliver L, et al. Ophthalmic Res. Nov. 4, 2024. Click image to enlarge. |
Two OCT biomarkers associated with age-related macular degeneration (AMD) onset and progression are choroidal thickness and choroidal vascularity index (CVI). To better understand how these metrics are altered throughout the disease course, researchers performed a longitudinal study that observed the rate of choroidal thinning and CVI changes in eyes with AMD. CVI is a newer metric derived from OCT data that quantifies the vascular area of the choroid as a percentage of the entire structure. Higher values indicate greater vascular capacity.
The study analyzed 105 eyes with varying stages of AMD: nonadvanced (n=46), exudative (n=28), central cRORA (n=5) and healthy eyes (n=26). Choroidal thickness and CVI were evaluated at baseline and throughout two to four years of follow-up. After adjusting the data for AMD stage, age and sex, the researchers estimated the annual rate of change for both metrics and analyzed their relationship with AMD progression.
The mean age of the cohort was 77 years and patients were followed for 3.4 years on average. The results highlighted a pronounced decrease in choroidal thickness and CVI in eyes with AMD compared to healthy eyes. Notably, eyes with exudative AMD showed the most significant choroidal thinning annually (-5.1%, -5.3% and -6.3% per year for subfoveal, temporal and nasal choroidal thicknesses, respectively), while those with central cRORA experienced the largest reductions in CVI (-1.09% per year).
“In eyes with exudative AMD, reduction in choroidal thickness and CVI could be explained by a reduced choroidal permeability caused by intravitreal anti-VEGF injections, which may vary depending on the drug used,” the researchers suggested in their paper, published recently in Ophthalmic Research. They cited a study from earlier this year that reported “a short-term reduction in CVI in patients treated with brolucizumab compared to those treated with aflibercept, which could be explained by the smaller size and higher tissue penetration of brolucizumab.”
Another important takeaway from this study is that “thinner choroids [with lower CVI] may indicate a higher risk for the development of geographic atrophy,” the researchers explained, as evidenced by the greatest CVI decrease being noted in central cRORA patients. “Progressive choroidal remodeling with connective tissue replacing previously preexisting vessels could explain this reduction in CVI,” they continued. Especially for patients with central atrophy, the authors argue the need for automated CVI calculation to be built into OCT platforms for better risk stratification.
“In conclusion,” they summarized, “healthy eyes have higher choroidal thickness and CVI values than eyes with AMD, but in all cases, this decreases over time.” Additionally, they proposed, “In patients with non-exudative AMD, the identification of faster changes in CVI over time may facilitate the detection of individuals at risk for atrophy progression. This, in turn, may inform the selection of those who may derive greater benefit from active treatment with complement inhibitors or neuroprotective agents.”
| Click here for journal source. |
Vidal-Oliver L, Spissinger S, Herzig-de Almeida E, Garzone D, Finger RP. Longitudinal changes in choroidal thickness and choroidal vascularity index in age-related macular degeneration. Ophthalmic Res. November 4, 2024. [Epub ahead of print]. |


