Several studies have focused on the incidence of idiopathic intracranial hypertension (IIH) instead its prevalence, but authors of a recent study focused primarily on the latter as well as geographic distribution from an epidemiologic and health economic perspective. Researchers from the University of Pennsylvania and the Mayo Clinic found that 3.44 per 10,000 women in the United States between the ages of 18 and 55 are affected and states with a higher prevalence of obesity had a lower-than-expected prevalence of IIH. The team’s work paper on the work was recently published in Ophthalmology.
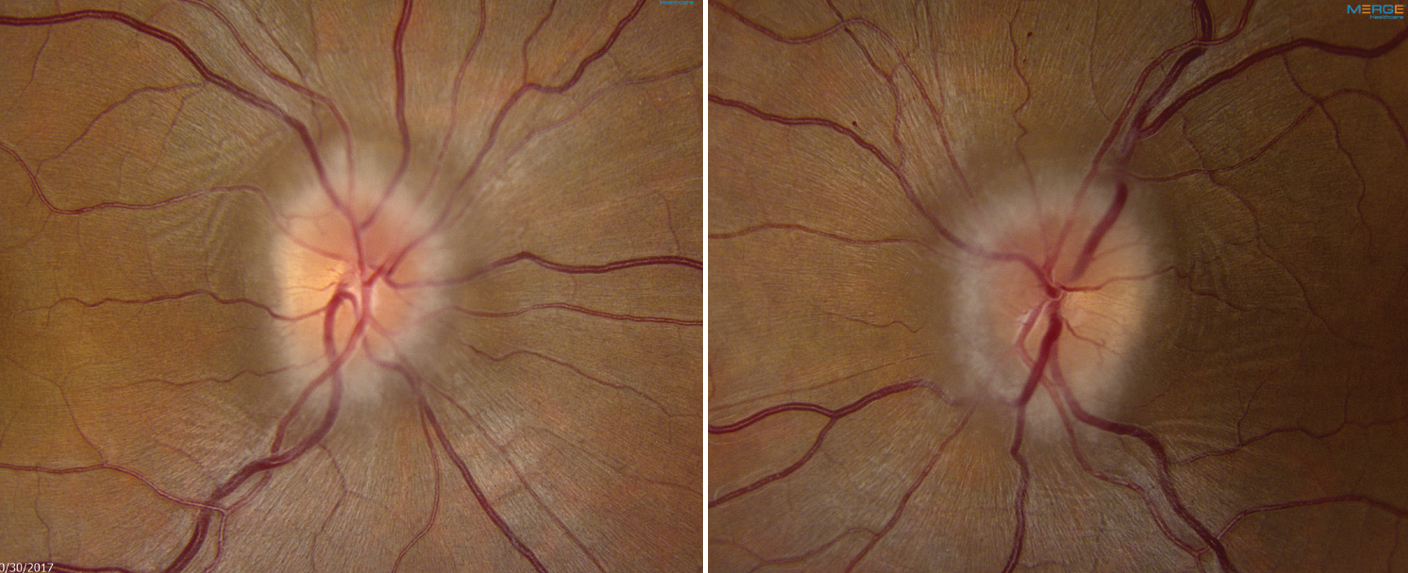 |
| Study shows idiopathic intracranial hypertension affects 3.44 per 10,000 women between the ages of 18 and 55 in the United States. Photo: Mark Dunbar, OD. Click image to enlarge. |
Of 13,959 female Medicaid beneficiaries with IIH diagnoses that were included, 48.9% had prescriptions for acetazolamide or methazolamide. They also calculated the proportion of female IIH patients who were insured by Medicaid (25%) by combining data from the Academy of Ophthalmology’s IRIS Registry and a consortium of academic ophthalmology departments called SOURCE.
The authors found significant geographic variation in the prevalence of IIH among women. “This pattern generally mirrors that of the state-level prevalence of obesity, the primary risk factor for IIH,” the authors wrote in their paper. “However, some states with a higher prevalence of obesity (e.g., Texas, Oklahoma and Alabama) had a lower than expected prevalence of IIH, and this was not explained by differences in Medicaid eligibility and coverage between states.” Because identifying IIH in administrative claims data requires a corresponding healthcare encounter, it’s possible that IIH is underdiagnosed in some states due to limitations in healthcare access and availability, the authors proposed.
For example, the authors wrote, “if patients are referred less frequently or face greater difficulty scheduling an appointment with an ophthalmologist or optometrist in certain states, their papilledema may go unrecognized, and symptoms of IIH could instead be attributed to a primary headache disorder such as migraine.”
The presence of geographic variation may also point to other socioeconomic or environmental risk factors for IIH, which are currently unknown, but the authors wrote that such variation can serve as hypothesis-generating data to guide further investigations. “For example, observations that multiple sclerosis is more common at northern and southern latitudes compared to equatorial regions led to the hypothesis that its pathogenesis was related to sunlight exposure and vitamin D levels, which was confirmed in subsequent studies and is now central to our understanding of this disease,” they explained. “In ophthalmology, spatial variation in cataract, dry eye and uveitis has been linked to local air pollution levels.”
Understanding the regional distribution of IIH is also important for contextualizing the availability of certain limited healthcare resources such as neuro-ophthalmologists and may inform enrollment s strategies for IIH research studies by targeting recruitment efforts to areas with a higher prevalence.
| Click here for journal source. |
Fraz MA, Kim M, Chen JJ, et al. Nationwide prevalence and geographic variation of idiopathic intracranial hypertension among women in the United States. Ophthalmology. October 24, 2024. [Epub ahead of print.] |


