 |
|
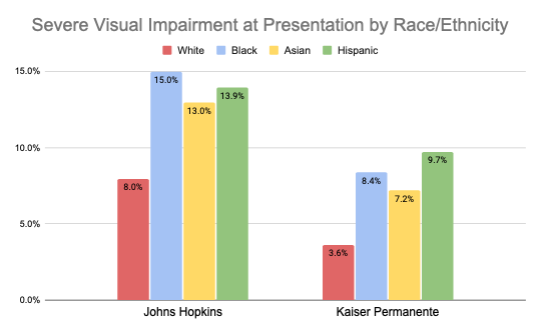
Data from the study shows disproportionately higher rates of severe visual impairment in non-white groups seen at both institutions. Photo: Awidi AA, et al. Ophthalmology. July 19, 2024. Click image to enlarge. |
A recent cross-sectional study published in the journal Ophthalmology found that Black, Asian and Hispanic patients as well as individuals of any ethic background who live in more economically disadvantaged neighborhoods have a higher likelihood of visual impairment due to cataracts at the time of surgery. Put another way, these demographic and socioeconomic groups endure the quality-of-life hardships brought on by cataract development for a longer period of time than others.
Researchers explored the relationship between race/ethnicity and socioeconomic status with visual impairment prior to cataract surgery among patients aged 65 years and older who underwent surgery across two health systems in the U.S. Mid-Atlantic region (Johns Hopkins Hospital and Kaiser Permanente) between January 2017 and December 2019.
This analysis included the following covariates: patient age, sex, smoking status, surgery laterality, Charlson Comorbidity Index (a measure of the relative one-year risk of mortality based on 17 possible systemic conditions) and ocular comorbidities such as glaucoma, AMD and diabetic retinopathy and others. The main outcome measure was the assessment of visual acuity prior to cataract surgery, categorized as mild (20/40 or better), moderate (between 20/40 and 20/200), and severe (20/200 or worse).
Of the study participants, 11,509 patients (17,731 eyes) were from Johns Hopkins Hospital and 7,143 patients (10,542 eyes) were treated at Kaiser Permanente. After adjusting for covariates, the study authors found that Black, Asian and Hispanic patients were more likely to have worse visual acuity secondary to cataracts at both facilities compared to white patients.
Data showed that living in more disadvantaged neighborhoods was also correlated with worse visual acuity at presentation prior to cataract surgery for patients seen at Johns Hopkins; however, the same association was not observed among patients at Kaiser Permanente.
This is likely due to differences in patient populations, according to the study authors, who noted in their paper that Kaiser Permanente is an integrated health system and members are largely insured by their employer. At Johns Hopkins Hospital, however, “health care is provided to those who are under- and uninsured through financial assistance programs. Thus, it was not surprising that Kaiser Permanente only had about 8% of their population living in deprived neighborhoods compared to 14% at Johns Hopkins Hospital.”
When summarizing their findings in Ophthalmology, the research team emphasized that “older patients of Black, Asian and Hispanic race/ethnicity, as well as patients living in more economically disadvantaged neighborhoods, were more likely to present with worse visual acuity due to cataracts at the time of cataract surgery.”
They also noted that “non-white patients and those with social needs (e.g. financial strain, food insecurity, housing instability) are at greater risk of vision loss from cataracts at the time of cataract surgery possibly due to social, structural and institutional barriers. Future studies should investigate health system-based programs to intervene on these racial/ethnic and socioeconomic barriers.”
Awidi AA, Woreta FA, Sabit A, et al. The Effect of Racial/Ethnic and Socioeconomic Differences on Visual Impairment Prior to Cataract Surgery. Ophthalmology. July 19, 2024 [Epub ahead of print]. |


