 |
|
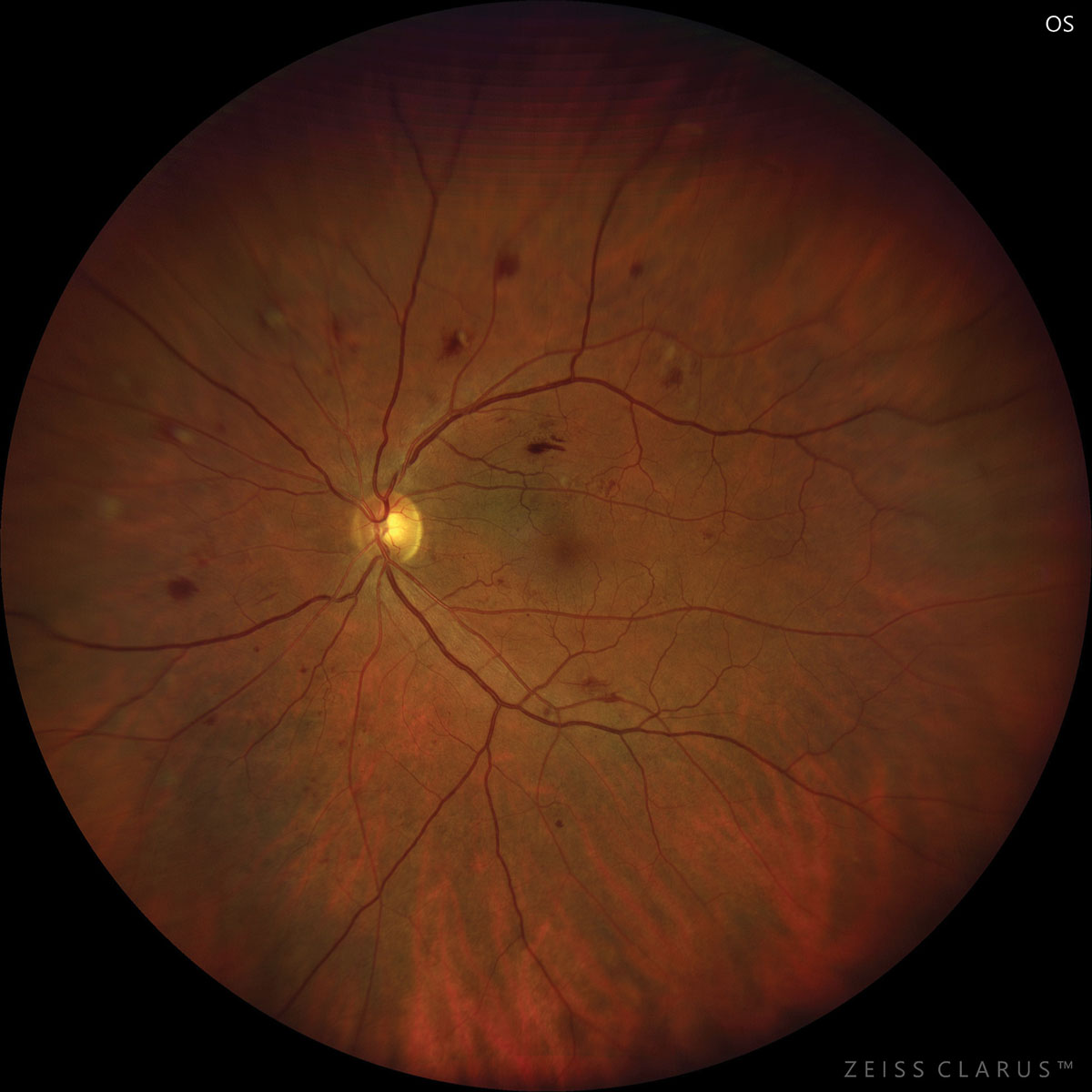
Non-glycemic metabolic risk factors may be especially relevant to the risk of retinopathy in prediabetes and extend the previously suggested protective effect of female sex on retinopathy in diabetes to prediabetes. Photo: Jay Haynie, OD. Click image to enlarge. |
Like diabetes, prediabetes can also be associated with microvascular complications, including neuropathy, nephropathy and retinopathy. The National Health and Nutrition Examination Survey (NHANES) documented the presence and severity of retinopathy in its participants through the evaluation of retinal photographs between the years 2005 and 2008. Researchers based out of the Wilmer Eye Institute at Johns Hopkins University School of Medicine used data from the study to investigate the relative contribution of systemic risk factors to retinopathy in prediabetes and evaluate associations of systemic risk factors and comorbidities with retinopathy in individuals with prediabetes. They determined the prevalence in the prediabetes group was 7.69%. Results of the study were recently published in the British journal Eye.
Their data also revealed an inverse association with female sex and retinopathy in this cohort, though there was a similar trend in the diabetes group that did not reach statistical significance. Nonglycemic metabolic risk factors may be especially relevant to the risk of retinopathy in prediabetes and extend the previously suggested protective effect of female sex on retinopathy in diabetes to prediabetes.
A group of 2,098 participants aged 40 and older with available HbA1c and gradable retinal images from the NHANES 2005–2008 were included in this retrospective cross-sectional analysis. Individuals were classified into three cohorts (control, prediabetes or diabetes) based on HbA1c level and anti-diabetic medication use.
“Though the severity of retinopathy differed across the three groups as expected, we identified an overall prevalence of retinopathy of 5.95% even in the control group,” the study authors wrote in their paper.
Multivariable logistic regression revealed an inverse association of female sex (odds ratio; OR: 0.25), estimated glomerular filtration rate (eGFR; OR: 0.98) and fasting glucose levels (OR: 0.92) with retinopathy in individuals with prediabetes. There was a positive association with a race/ethnicity classification of “Other” (OR: 6.05). Comparison of ORs between groups indicated differential associations of “Other” race, fasting glucose and C-reactive protein (CRP) with retinopathy in prediabetes compared with diabetes. Increased CRP was linked with higher odds of retinopathy in prediabetes, though not statistically significant, but also significantly lower odds of retinopathy in diabetes.
Still, specific conclusions regarding these observations are challenging due to the heterogeneous composition of the “Other” race/ethnicity group, but the researchers suggested that underrepresented ethnic populations may have increased risk of retinopathy in the setting of prediabetes, which underscores the importance of inclusion in appropriate risk assessment.
“Using the NHANES dataset, this prevalence differs overall among racial groups, with higher rates in Non-Hispanic Blacks and Hispanics compared with Non-Hispanic Whites,” they noted. “These results confirm that retinal abnormalities occur even in individuals who have not yet developed diabetes and also suggest that racial/socioeconomic disparities may predispose non-White ethnic groups to develop microvascular complications earlier in the setting of dysglycemia.”
“Our findings confirm published estimates regarding retinopathy prevalence in prediabetes and suggest a protective effect of female sex on retinopathy in prediabetes, an increased risk of retinopathy in underrepresented racial/ethnic groups in the setting of prediabetes and a unique differential association between clinically evident retinopathy and CRP in prediabetes that warrants further investigation,” the study concluded.
Association of systemic and demographic risk factors with prevalence of retinopathy in US adults with prediabetes. Eye (Lond). July 13, 2024. [Epub ahead of print]. |


