 |
|
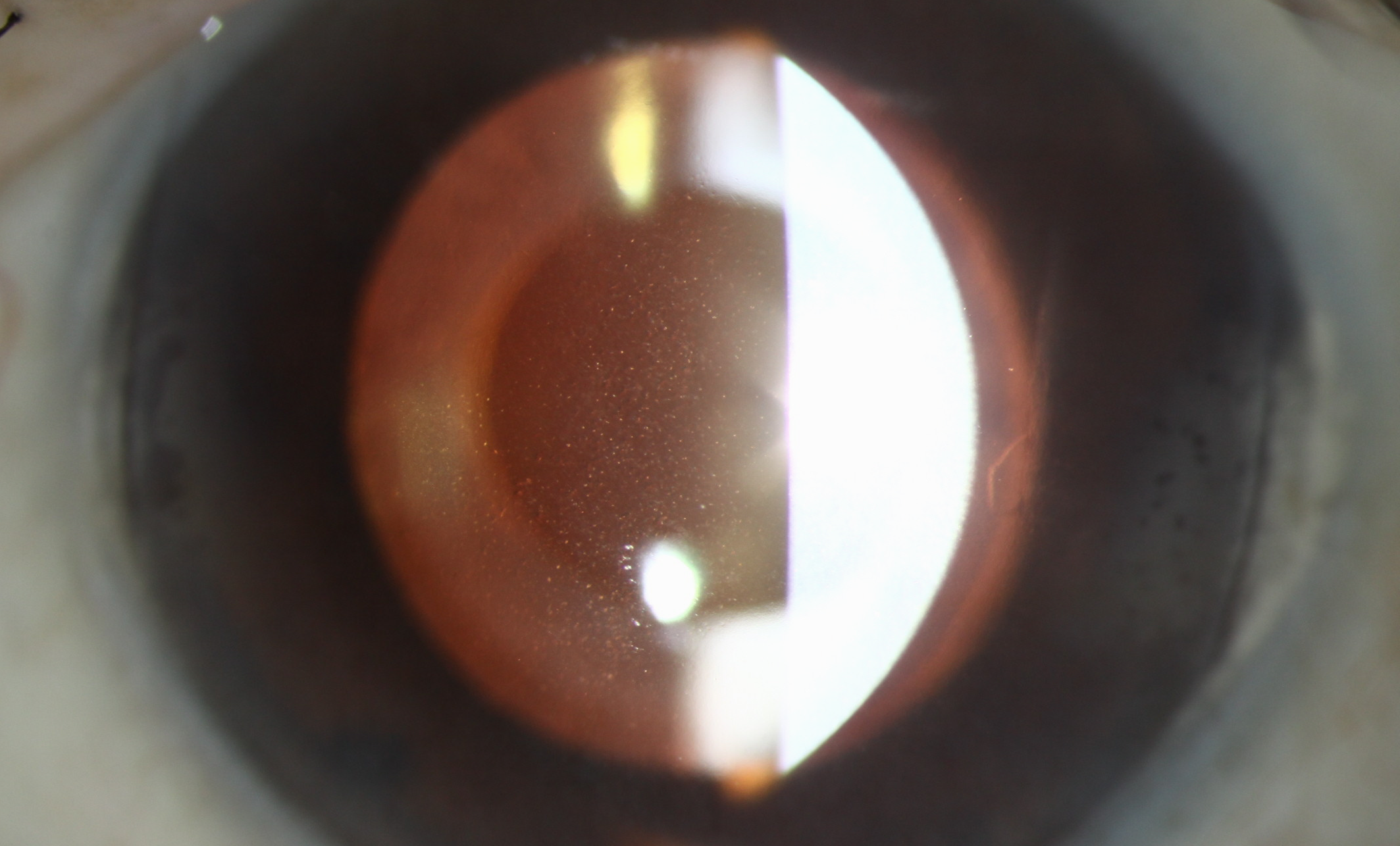
Between 2013 and 2020, the IRIS Registry of ophthalmology practices logged 1.95 million Fuchs’ cases, a figure that represented 37.3% of all corneal dystrophy cases in the database. Photo: Christine Sindt, OD. Click image to enlarge. |
In the largest US-based epidemiologic assessment of corneal opacity to date, researchers retrospectively looked data on this presentation from the Intelligent Research in Sight (IRIS) Registry. The investigation, recently published in Ophthalmology, analyzed demographic and clinical data of 79,887,324 patients who presented to eye clinics that participate in the IRIS Registry within a seven-year period (2013 to 2020). A notable shortcoming of the analysis is the exclusion of optometry practice data from the IRIS database, which would have made this study more representative of eyecare services provided in the United States.
Nevertheless, from this large set of patients 5,220,382 individuals were identified as being diagnosed with corneal opacity and scars via ICD-10 and ICD-9 codes over the study period. During the study period, the case frequency of corneal opacity was 6,535 per 100,000 visits, or 6.5%. A marginal majority of these patients were women, making up 57.6%, and mean age was reported to be 63.4 ±18.1 years. Bilateral corneal opacity occurred in 38.4% and unilateral cases in 30.0%. Most patients were white (69.1%), followed by Black (6.8%), Asian (2.5%), American Indian or Alaska Native (0.3%) and Native Hawaii or Pacific Islander (0.2%) patients; 7.3% of corneal opacity patients reported Hispanic or Latino ethnicity.
The most common etiologies that were identified to be associated with corneal opacity were corneal dystrophies (64.7%), edema (18.3%), ulcer (7.8%), keratoconjunctivitis (7.2%), degeneration (5.6%), neovascularization (6.3%) and trauma (5.3%). Average baseline visual acuity was 20/26 and this worsened from corneal opacity to 20/58; post-management improved slightly to 20/54. Worse visual outcomes were observed in women compared with men, as well as in Asian, Black and American Indian or Alaska Native patients compared with White patients. As for underlying causes, worse visual outcomes were associated with corneal malformation, degenerative disorders, edema, injury and ulcer when compared with those with hereditary corneal dystrophies.
In the discussion section of their paper, the study authors elaborate on their findings. Among corneal dystrophies, corneal endothelial dystrophy was the most common disease form and was seen in about 1.95 million (37.3%) people. Keratopathies were underlying etiologies in 7.2% of patients, with exposure keratoconjunctivitis making up 5.4%, neurotrophic 1.2% and phlyctenular 0.6%. Infectious keratitis was the underlying etiology in 3.0%, and of these patients, viruses were the most common causative organism (1.6%), followed by bacteria (1.3%), fungi (0.1%) and Acanthamoeba (0.01%).
The study authors do note that despite the IRIS Registry being quite a large dataset, it is limited to patients undergoing assessment at ophthalmic practices, thus not being totally representative of corneal opacity prevalence of the entire US population. However, as the authors argue, “the high case frequency of corneal opacity cases in the IRIS registry highlights the significant public health impact of opacity causing corneal disorders in the population. Additionally, it highlights urgent need for developing practice patterns that emphasize in the need for developing screening protocols that help in early detection and treatment of individuals affected by various etiologies causing corneal opacities.”
Singh RB, Dohlman TH, Ivanov A, et al. Corneal opacity in the United States: an American Academy of Ophthalmology IRIS Registry (Intelligent Research in Sight) study. Ophthalmology. July 8, 2024. [Epub ahead of print]. |


