 |
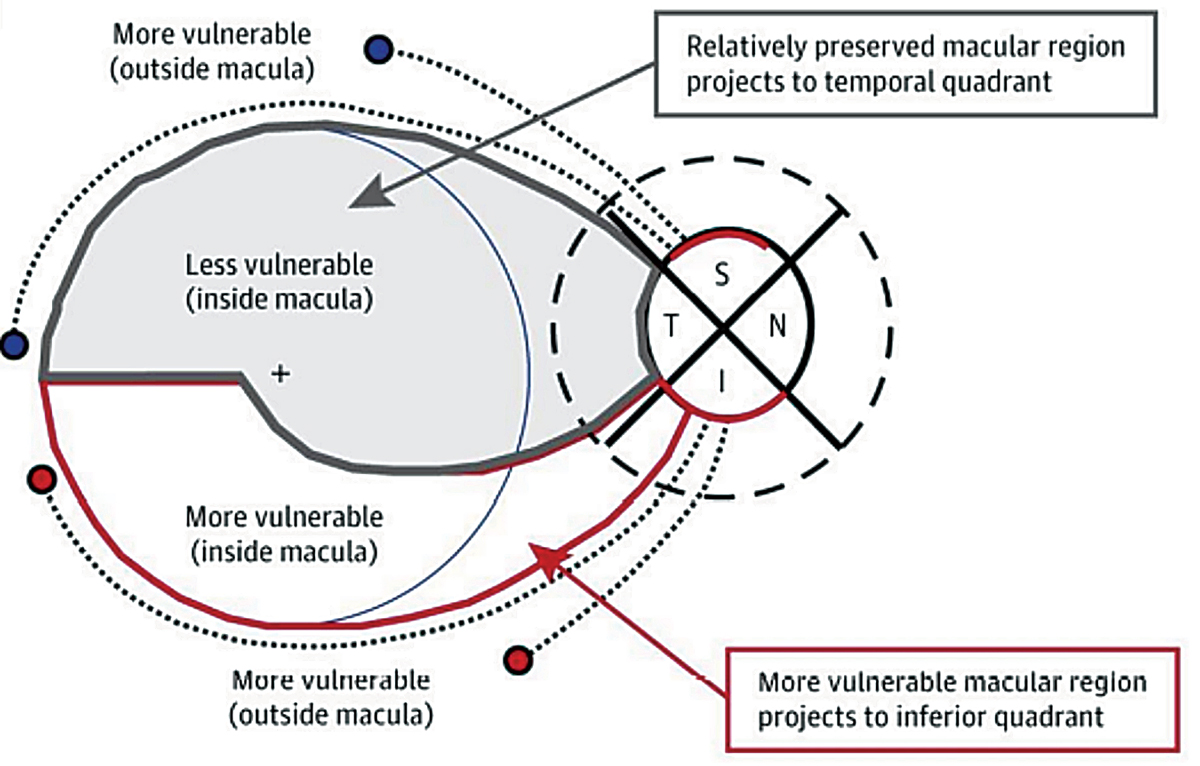
| If a patient’s axial length differs more than 1.0mm between eyes, clinicians may observe structural differences in the optic nerve head, thinner RNFL and GCIPL and more rapid vision loss, this study suggests. This illustration demonstrates the inferior vulnerability zone, which consists of macular fibers that are at risk for damage due to glaucoma. The superior vulnerability zone does not consist of macular fibers. Photo: Andrew Rouse, OD. |
Research has suggested a clear relationship between myopia and glaucoma; axial elongation in myopic eyes stretches posterior ocular structures, resulting in progressive thinning of the retina, choroid and sclera and a higher susceptibility of lamina cribrosa deformation. In turn, these patients are subjected to a greater likelihood of glaucomatous optic disc changes. With the knowledge that axial length and glaucoma are related, a recent study aimed to determine whether there is a difference in inter-eye glaucoma severity and progression in patients with asymmetric axial length. The results revealed that glaucoma tended to be more severe and to progress faster in the longer eye.
The long-term observational study included 190 eyes of 95 glaucoma patients with asymmetric axial length (>1.0mm difference between eyes) from a university hospital in Korea. The researchers classified each person’s eyes as the “longer eye” and “shorter eye” then performed an analysis on baseline and follow-up clinical data. The mean patient age was about 51 years, and the mean follow-up period was just over 10 years.
Here are some of the main findings from the study:
- There was no difference in baseline intraocular pressure or central corneal thickness between longer and shorter eyes.
- Several baseline disc parameters were greater among longer eyes, including ovality index, beta-zone and gamma-zone parapapillary atrophy.
- In baseline OCT data, the thickness of the RNFL and ganglion cell-inner plexiform (GCIPL) layer was reduced in longer eyes vs. short eyes.
- The mean deviation and visual field index values were significantly lower in the longer eyes according to a baseline visual field test.
The researchers also reported differences in glaucoma progression between longer and shorter eyes. The following rates of change were greater in longer eyes: superior GCIPL (longer eyes: -0.65μm/yr, shorter eyes: -0.40μm/yr), mean deviation (longer eyes: -0.40dB/yr, shorter eyes: -0.21dB/yr) and visual field index (longer eyes: -0.92%/yr, shorter eyes: -0.46%/yr).
“The greater the difference between the mean IOP and beta-zone parapapillary atrophy area between inter-eyes, the greater the difference in the rate of change of RNFL and GCIPL,” the study authors pointed out in their paper, published in Ophthalmology. Furthermore, they added, “the greater the difference in IOP fluctuation, the greater the difference in the rate of change between mean deviation and visual field index.”
All these observed differences between clinical parameters of longer vs. shorter eyes “provide insights into the nuanced nature of glaucomatous changes associated with axial length dissimilarities,” the authors noted. When evaluating patients with an inter-eye axial length difference of more than 1.0mm, it may behoove eye clinicians to consider that—based on the findings of this study—the longer eye may experience structural differences in the optic nerve head (larger ovality index and parapapillary atrophy area), greater thinning of the RNFL and GCIPL and more rapid change in mean deviation and visual field index. Additionally, the inter-eye difference in glaucoma progression rate appears to relate to both mean IOP and IOP fluctuation.
“Longer eyes, as characterized by structural variations at baseline and an accelerated rate of glaucomatous change, exhibit a higher susceptibility to disease severity and progression,” the researchers concluded in their paper. “Understanding these differences in glaucoma manifestation within individuals with differing axial length could aid in personalized treatment strategies and reinforce the importance of establishing an early treatment strategy in cases with notable structural disparities.”
Huh MG, Jeong Y, Shin YI, et al. Assessing glaucoma severity and progression in individuals with asymmetric axial length: an intra-patient comparative study. Ophthalmology. July 15, 2024. [Epub ahead of print]. |


