A recent analysis found that widefield OCT angiography (WF-OCTA), which can identify minute vessel tortuosity alterations, offers a noninvasive alternative for the detection of early postoperative proliferative changes among patients with rhegmatogenous retinal detachment (RRD).
“Proliferative retinal changes may occur post-surgery for RRD, possibly preceding recurrent detachment,” the study authors noted in the journal Translational Vision Science & Technology. “This study aims to establish the groundwork for an imaging system capable of discerning changes in retinal vessel tortuosity after RRD repair, analyzing WF-OCTA images.”
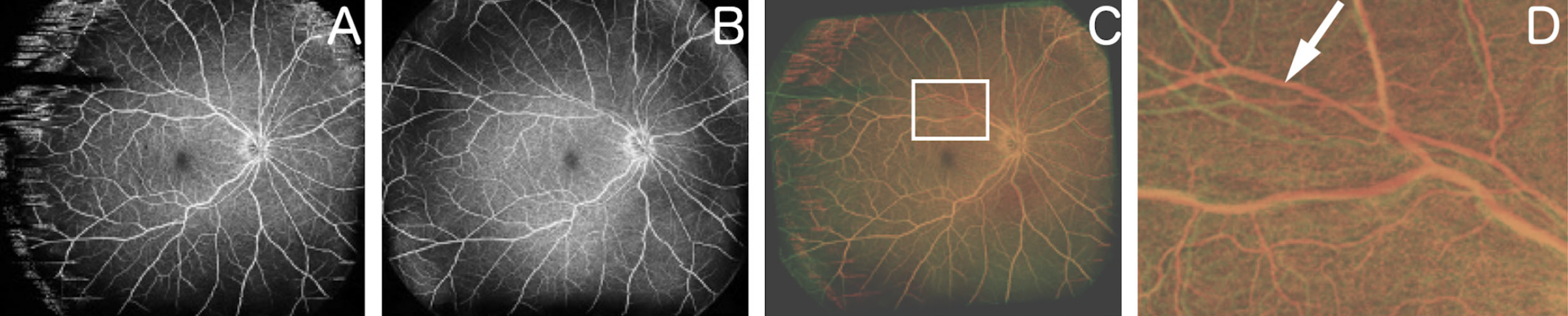 |
| Using widefield OCT angiography to observe vessel tortuosity changes can aid in the identification of early postoperative proliferative changes in eyes with rhegmatogenous retinal detachment. These images from the study show: (A) an OCT-A image obtained one month after RRD repair, (B) another obtained two months after surgery, (C) overlaid image after changing A and B to red and green, respectively, and (D) a magnified image of the superior area of C, where white arrow indicates retinal vessel tortuosity change. Photo: Fukuda Y, et al. Transl Vis Sci Technol. Aug, 8, 2024. Click image to enlarge. |
This retrospective study enrolled 88 eyes of 86 patients with rhegmatogenous retinal detachment who underwent surgical procedures. Study participants also had repeated imaging with both nonangiographic widefield OCT (WF-OCT) and WF-OCTA on different postoperative days.
The patient cohort included 60 men and 26 women with an average age of 50.0 ± 16.7 years. Among these eyes, 56 underwent pars plana vitrectomy, 27 had scleral buckling and five had a combination of both procedures, according to the study authors.
The objective was to use a combination of WF-OCT and WF-OCTA coupled with specialized imaging software to identify alterations in retinal vessel tortuosity in patients with proliferative vitreoretinopathy (PVR) following surgical intervention for rhegmatogenous retinal detachment repair.
To identify alterations in retinal vessel tortuosity, the study authors compared WF-OCTA images over time. The investigators also examined 48 healthy eyes, capturing WF-OCT and WF-OCTA images twice on the same day, to ensure the reliability of detecting retinal vessel tortuosity changes and accuracy of alignment via the image processing used in this study.
After imaging processing, the research team detected changes in retinal vessel tortuosity in 66 quadrants. “These changes, attributed to retinal traction from proliferative membranes, were observed in 56 quadrants, among which retinal thickness remained unchanged in seven sectors (12.5%) according to the WF-OCT map,” they reported. “In nine quadrants, changes in retinal vessel tortuosity were attributed to changes in subretinal fluid, aligning with observable variations in retinal thickness.”
This data offers insights into the utility of WF-OCTA and WF-OCT as a way to assess changes in retinal vessel tortuosity and retinal thickness among patients with rhegmatogenous retinal detachment. “These imaging techniques provide a valuable means of identifying the roots of retinal complications and offer pertinent information for clinical management,” the study authors concluded in their Translational Vision Science & Technology paper.
Fukuda Y, Ishikawa K, Kiyohara K, et al. Postoperative proliferation detection in eyes treated for rhegmatogenous retinal detachment by widefield OCT angiography. Transl Vis Sci Technol. Aug. 8, 2024 [Epub ahead of print]. |


