 |
|
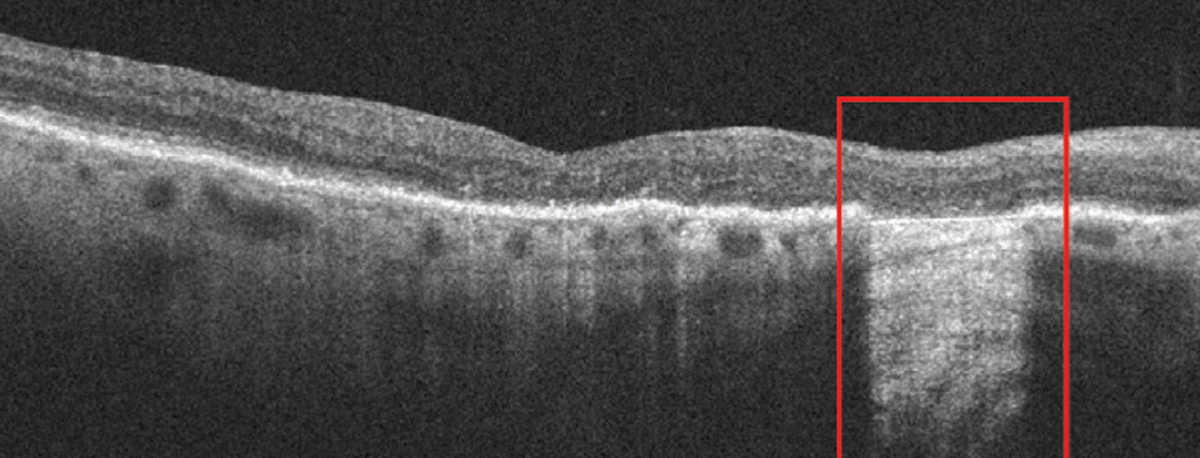
A study in Ophthalmology Science suggests the value of certain OCT measurements, such as the extent of RORA and OPL deterioration, for anticipating visual acuity outcomes in patients with this form of AMD. Photo: Anna Bedwell, OD. Click image to enlarge. |
Experts from the Classification of Atrophy Meetings have established a unified terminology and set of criteria for identifying atrophy based on OCT results in patients with age-related macular degeneration (AMD). Retinal pigment epithelium (RPE) degradation becomes noticeable later in the disease course, referred to as RPE and outer retinal atrophy (RORA). This eventually evolves into complete RORA (cRORA), with lesions typically appearing first in the extrafoveal area and subsequently expanding into the foveal center. While central foveal involvement can affect BCVA, lesion presence and extent don’t always correlate with visual acuity. Hoping to gain more clarity on the pathogenesis of RORA and resulting visual impairment, researchers conducted a small retrospective study, the findings of which were recently published in Ophthalmology Science.
Sixty-four eyes of 64 patients from 10 hospitals in Japan were included in the investigation (mean age: 76.8 years; 59% men). All eyes had cRORA associated with AMD with foveal center involvement. The main outcome measure was the relationship between BCVA and the extent of RORA and outer plexiform layer (OPL) deterioration as measured by OCT.
The study authors made the following observations from the data:
- BCVA was significantly related to the extent of retinal atrophy and the deterioration in the outer plexiform layer.
- A notable reduction in central retinal thickness was associated with worse visual outcomes.
- There was a strong statistical relationship where eyes with deeper retinal atrophy tended to show extensive OPL damage and more profound visual acuity loss.
- Higher levels of retinal atrophy were observed alongside conditions like reticular pseudodrusen, further compounding the effect on visual acuity.
“Eyes with BCVA >20/60 more often exhibited RORA ≥3,000μm, OPL deterioration ≥1,700μm and complete central OPL defect after adjusting for age and sex,” the researchers wrote in their paper. Additionally, after adjustment, “the RORA ≥3,000μm was associated with OPL deterioration ≥1,700μm and the presence of complete central OPL defect.”
This data underscores the predictive values of specific OCT measurements, such as the extent of RORA and OPL deterioration, for anticipating visual acuity in patients affected by this form of macular degeneration.
“In conclusion,” the researchers wrote in their paper, “a longer extent of cRORA in the OCT images with foveal center involvement was associated with a longer extent of OPL deterioration and defect, particularly at the foveal region, and worse BCVA.” They posit that this study “will help understand the pathogenesis of RORA and geographic atrophy and how to evaluate the lesion in a daily clinic.”
Nagai N, Matsubara H, Terasaki H, et al. Extent of complete retinal pigment epithelial and outer retinal atrophy with foveal center involvement is associated with visual acuity. Ophthalmol Sci. August 28, 2024. [Epub ahead of print]. |


