 |
|
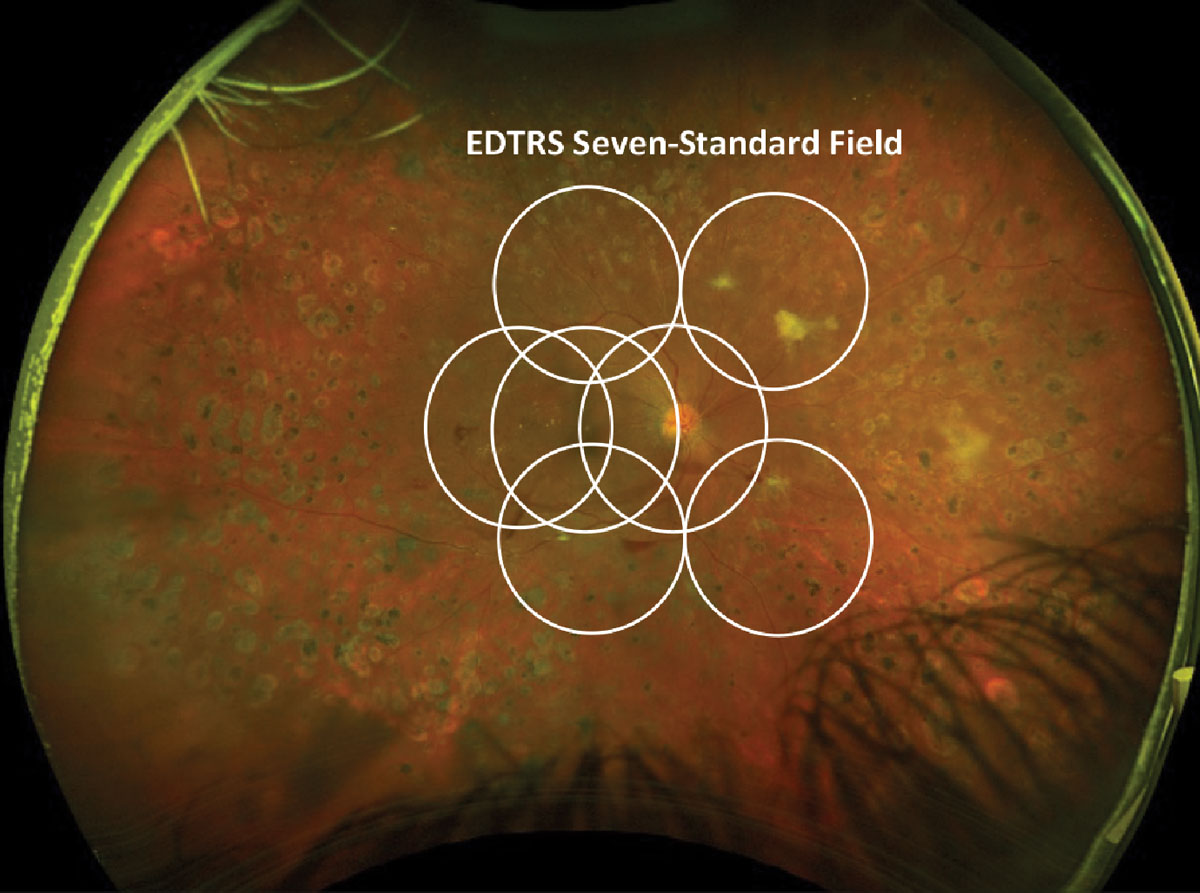
Agreement for standard color grading within one step and within two steps for the ETDRS 7F images were 90% and 97%, respectively, while the UWF images agreement within one- and two-steps were 85% and 94%, respectively. This suggests grading differences seen between these modality types may more generally be due to standard grader variability than true differences in ability to assess DR severity. Photo: Julie Torbit, OD, and Brad Sutton, OD. Click image to enlarge. |
Decades of reliance on the ETDRS 7-field (7F) photo montage in the assessment of diabetic retinopathy (DR) is at odds with the rising popularity of ultra-widefield (UWF) imaging. However, if there is high concordance between the two in sensitivity for DR, this would allow for the combination of both modalities to be used in clinical studies and care settings. Consequently, researchers were interested in testing both options’ comparability in terms of DR severity and associations with risk factors, like hemoglobin A1C, age, diabetes duration and sex.
The study describes the outcomes of the randomized clinical Diabetes Control and Complications Trial (DCCT) and the subsequent observational Epidemiology of Diabetes Interventions and Complications (EDIC) study. A total of 1,441 type 1 diabetes patients were included in the DCCT, of which 1,375 were enrolled in the EDIC study. Between March 2019 and December 2021, 1,171 participants were active, and of these, UWF color imaging and 7F fundus photographs were obtained from 785 patients.
Among those studied, 53% were male with a mean age of 61 years. DR grading was correlated for all outcomes between UWF-7F and 7F images, even for severe outcomes. Severe nonproliferative DR demonstrated concordance of 96%; proliferative DR of 97%, scatter photocoagulation 99% and focal photocoagulation 98%. Most DR severity scores were within one step of agreement (92%), with only 3% being more than two steps apart on the ETDRS severity scale. However, DR severity assessed within the UWF-global area was higher compared with 7F, despite both modalities being correlated, showing 81% one-step agreement and 94% within two-step agreement.
Based on the very high concordance seen, the authors relay in a recent paper for JAMA Ophthalmology that, “these data support the transition between these techniques as not compromising data quality in the DCCT/EDIC studies, similar to the successful transition from film to digital images in 2009. They also support the use of UWF imaging as a way to both maintain comparison to prior DCCT/EDIC data and to allow study of the novel information provided by the new modality.”1
More generally, the authors relay that “this study supports both the use of UWF-7F imaging as a comparable method of evaluating DR severity with past DCCT/EDIC outcome measures, as well as the potential to use UWF-global assessment to assess potential new risks and associations provided by the additional visualized retinal area.”1
Although this data is promising, a separate group of researchers who submitted an invited commentary on the paper expressed some reservations about the applicability of these results in practice. As they point out, several unmet needs and challenges remain, of which they point out three main ones.
The first is that the DCCT/EDIC cohort imaging was standardized with ongoing quality control trained technicians and trained fundus photograph graders, but lack of standardization in typical clinical settings can affect image quality and grading consistency.
Second, they argue that there is still a lack of longitudinal studies that exist on validating effectivity of UWF imaging in predicting long-term results compared with 7F imaging. Finally, factors such as image quality, resolution and color caused by differences in light source, laser wavelength and field of view on devices can lead to different capabilities in identifying DR lesions.
With these potential limitations, the commentary authors caution that, “while UWF imaging shows promising results in enhancing DR detection and management, addressing the unmet needs is essential for its successful integration into clinical practice and research. Standardized protocols, comparability studies, and longitudinal clinical research will help maximize the potential of UWF imaging in improving outcomes for patients with DR.”2
1. Aiello LP, Blodi B, Gao X, et al. Ultra-widefield and early treatment in diabetic retinopathy study 7-field grading of diabetic retinopathy. JAMA Ophthalmol. August 15, 2024. [Epub ahead of print]. 2. Lobo C, Santos AR, Marques IP. Moving forward to a wider retinal field of view. JAMA Ophthalmol. August 15, 2024. [Epub ahead of print]. |


