 |
|
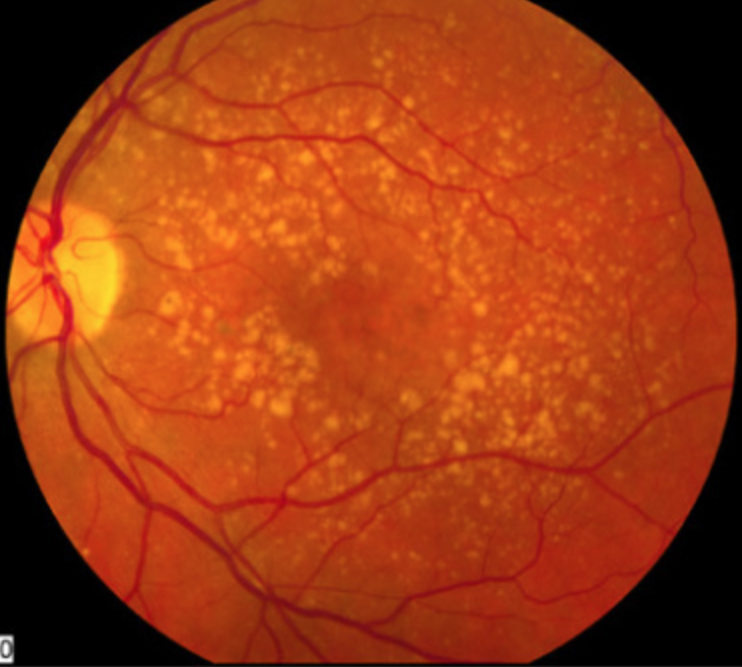
As AMD progresses, patients might experience a shift in the pattern of retinal sensitivity across the visual field potentially linked to structural and functional transformations occurring in the macula. Photo: NEI. Click image to enlarge. |
In the initial stages of age-related macular degeneration (AMD), many patients with relatively good BCVA may still experience noticeable difficulties with their vision, particularly under conditions of low light or poor contrast. Hence, there's a significant interest in identifying more sensitive and specific clinical indicators for early diagnosis, disease progression and response to treatment in AMD.
Some eyecare clinicians and researchers have recently gravitated towards microperimetry for its ability to assess retinal sensitivity at multiple points and discern differences among healthy individuals and those with early or intermediate AMD. Contrast sensitivity testing can also provide insights on early functional vision loss. Combining both of these potential functional clinical markers for AMD, a new study published in Ophthalmic Research by a team of Swiss and Portuguese researchers evaluated retinal sensitivity in different macular subfields by microperimetry and looked for correlations with contrast sensitivity values in healthy controls and patients in early and intermediate disease stages.
In the prospective longitudinal study, retinal sensitivity of 92 eyes from 92 participants (13 early AMD, 31 intermediate AMD and 48 controls) was measured using a customized 24-point grid in microperimetry assessments, and the data were segmented into several subfields. Although optometrists have workhorse contrast sensitivity tests like the Pelli-Robson chart readily available, this study used a device called the Manifold Contrast Vision Meter—a digital monitor that can test multiple spatial frequencies and optotypes at once.
The team then analyzed the relationships between functional metrics and various personal and health-related variables of participants.
The data revealed that the association of retinal sensitivity with contrast sensitivity varied across the groups, being weakest in the control group, stronger in the early AMD group and strongest in the intermediate AMD group, indicating a pattern of progression where retinal sensitivity declines more visibly as the disease advances. Detailed subfield evaluations in controls showed significant associations of nasal retinal sensitivity with contrast sensitivity, while temporal retinal sensitivity generally showed weaker or no significant associations.
No significant association was observed between retinal sensitivity and fixation stability across all groups, indicating that the ability to fixate might not directly relate to this metric.
Overall, these findings suggest that as AMD progresses, there might be a consequential shift in the pattern of retinal sensitivity change, potentially linked to structural and functional transformations within the macula zone.
“It is important to recognize that retinal sensitivity both in healthy controls and also in AMD is not evenly distributed throughout the retina,” the researchers explained in their paper. “This cross-sectional study also suggests a different trajectory of loss of retinal sensitivity throughout the retina, which would have implications for the application of localized treatments. It will be important to investigate these localized differences longitudinally as well,” they concluded.
Chan EJ, Anders P, Garobbio SA, et al. Retinal sensitivity in macular subfields and their association with contrast sensitivity in early and intermediate age-related macular degeneration. Ophthalmic Res. July 24, 2024. [Epub ahead of print]. |


