 |
|
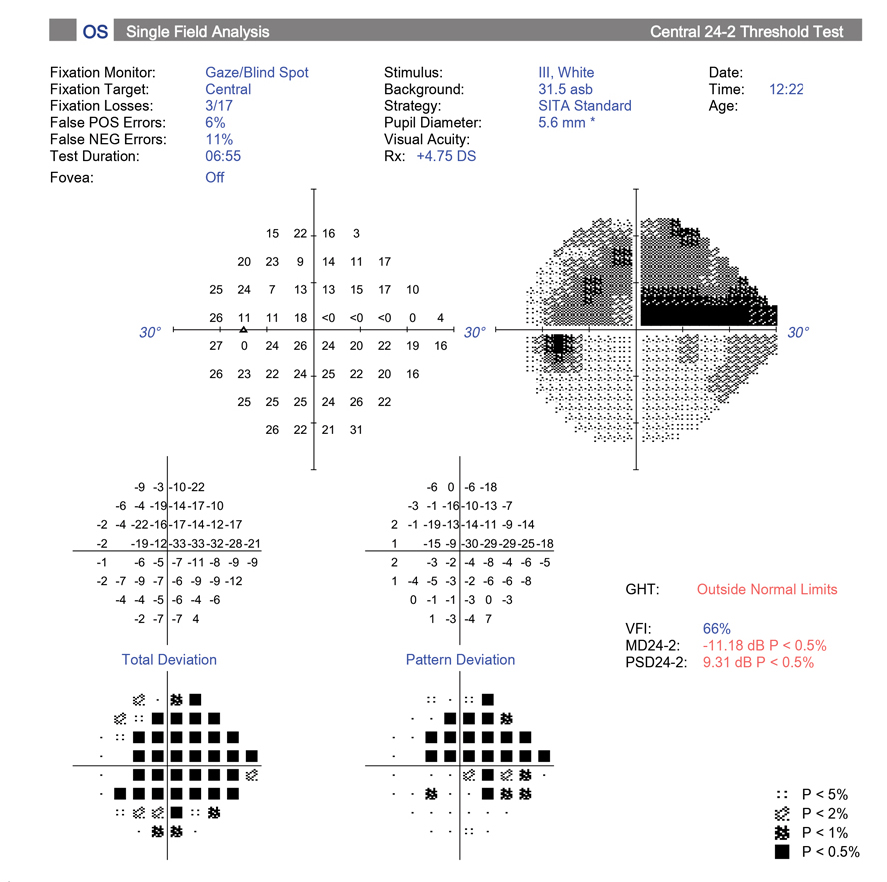
The poor performance of the OHTS-EGPS prediction model in this study may be partially explained by its reliance on a VF-based conversion event definition. Photo: Michael Chaglasian, OD, and Sarah B. Klein, OD. Click image to enlarge. |
Given the high prevalence of ocular hypertension (OHT) and concerns over visual field loss in cases that progress to glaucoma, it’s important to have an effective tool that can predict the risk of developing the disease. In a recent study, UK researchers sought to validate a model derived from the OHTS and EGPS studies using a retrospective EMR review. They found it performed poorly, although updating the model showed modest improvements in discrimination. The team’s paper on the work was recently published in Ophthalmology Glaucoma.
A total of 9,030 OHT patients living in England fit the inclusion criteria of an IOP between 22mm Hg and 32mm Hg (either eye), a normal baseline visual field (VF) test and no significant ocular co-morbidities. A total of 1,530 (16.9%) patients converted to glaucoma during the follow-up period.
Risk factors included age, ethnicity, sex, IOP, vertical cup-to-disc ratio, central corneal thickness, VF pattern standard deviation, family history of glaucoma, systemic hypertension and diabetes. The OHTS-EGPS model was applied to predict a patient’s risk of developing glaucoma in five years and was found to be poorly discriminative.
A likely explanation for the suboptimal model performance, the authors suggested in their paper, is “differences in patient characteristics, disease incidence and patient management between the populations of the original OHTS-EGPS trials and our study.”
The cumulative risk of conversion from OHT to glaucoma at five years (16.9%) was higher than the OHTS cohort but similar to the risks reported in the original EGPS study (16.8% in placebo group) and in a more recent but smaller clinically based study drawing data from five hospitals in England (17.5%). “However, there was considerable variation in conversion risk among hospitals, which may reflect differences in populations or treatment approach among different ophthalmologists, and both discrimination and calibration were worse in hospitals with particularly high-risk patients, highlighting the sensitivity of these models to disease incidence,” the authors added.
Overall, given the poor performance of the OHTS-EGPS model, the authors suggest that caution should be used in its application to populations that differ from those in the OHTS and EGPS.
| Click here for journal source. |
Wright DM, Azuara-Blanco A, Cardwell C, et al. Validating and updating the OHTS-EGPS model predicting five-year glaucoma risk among ocular hypertension patients using electronic records. Ophthalmology Glaucoma. October 28, 2024. [Epub ahead of print.] |


