 |
|
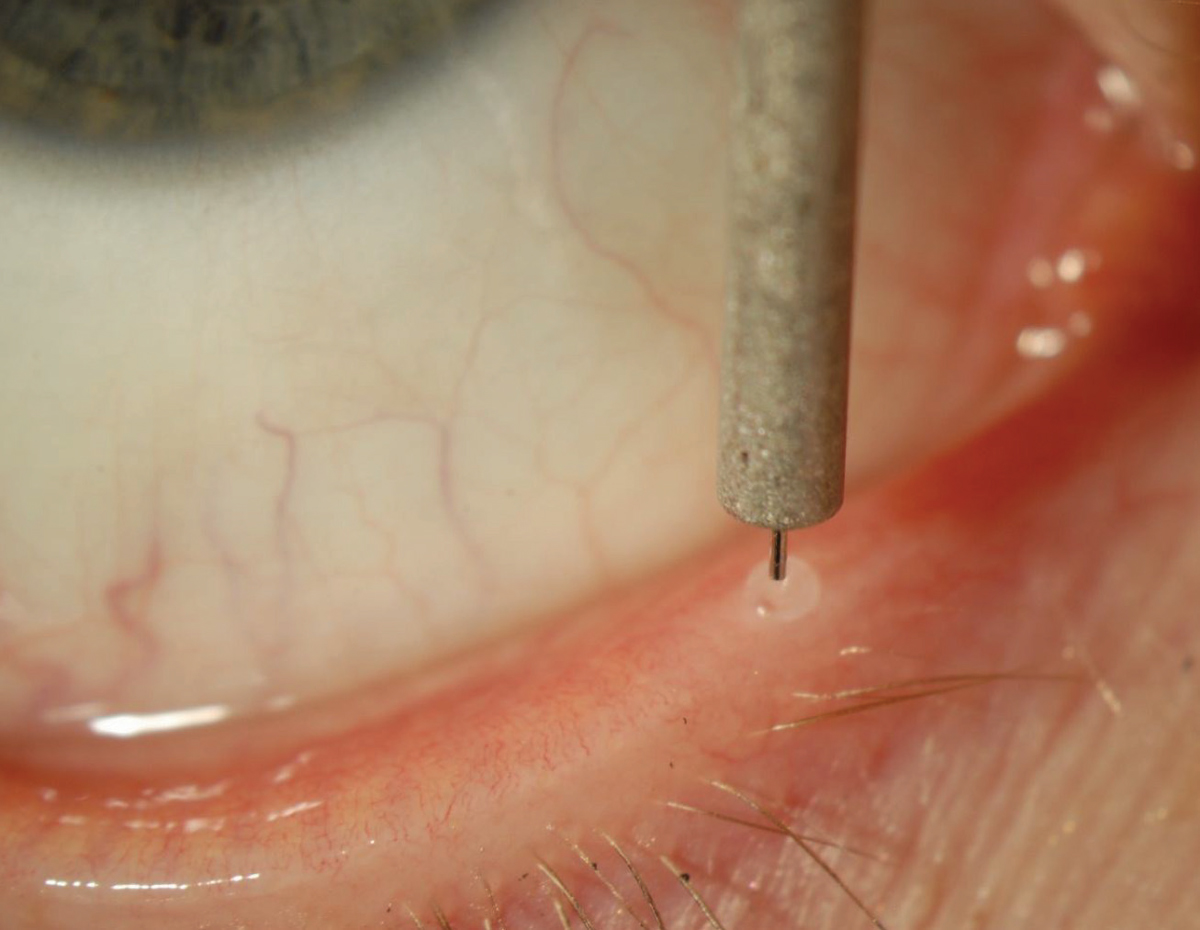
Punctal plugs and intracanalicular devices can become colonized with bacteria composed of oropharyngeal flora, skin flora and other rare but potentially significant pathogens. Photo: Alan G. Kabat, OD. Click image to enlarge. |
While punctal plugs and intracanalicular stents are effective options for treating dry eye, there is concern that bacterial colonization of the device may raise infection risks. In a recent study, researchers sought to characterize the microorganism specimens associated with these devices and found that oropharyngeal flora, skin flora and other pathogens can develop, but there were no cases of clinical infection. The team’s paper on the work was recently published in Eye & Contact Lens.
Devices were removed from participants who underwent placement of punctal plugs for tear insufficiency and lacrimal stents for dacryocystorhinostomy and canalicular reconstruction procedures; the inserts were then cultured. Primary outcome measures included culture positivity, identification of isolated microorganisms, recovery of microorganisms from culture and clinical evidence of ocular infection.
A total of 181 specimens were processed (174 punctal plugs, seven intracanalicular stents), of which 98 (54%) were culture positive. Of the punctal plugs, 92 were culture positive, including 42 with a single organism isolated, whereas 22 yielded two organisms, seven yielded three organisms and the remaining 21 yielded a polymicrobial culture with four or more organisms. The most common isolates from punctal plugs were coagulase-negative staphylococci (27.6%), diphtheroids (16.4%) and Streptococcus viridans (10.2%). Those plugs with polymicrobial culture results grew a mixture of organisms most consistent with skin or upper respiratory flora. Of the intracanalicular stents, six (85.6%) were culture positive.
A technique known as sonication was used to enhance the isolation of organisms by exposing the devices to sound waves, which agitates and dislodges adherent bacteria. “The increased yield in the number of organisms after the sonication step supports the existence of adherent bacteria or a biofilm that harbors microbial organisms on the devices,” the authors explained.
In their paper on the study, the authors noted it’s possible that bacterial colonization of punctal plugs could alter the conjunctival flora of individuals treated for dry eye. However, they added, one study evaluated the conjunctival flora of patients with dry eye with no difference in the prevalence of isolated bacteria from eyes with and without punctal plugs.
“Furthermore, coagulase-negative staphylococci was the most frequently isolated species in the present study,” and that is also the most frequently isolated aerobic bacteria from the conjunctiva dry eye patients, the authors wrote. “This suggests that the predominant conjunctival organisms may also most commonly colonize the punctal plugs and intracanalicular stents.”
Three mycobacterial isolates developed in this study, suggesting this organism is infrequently present in this location and doesn’t always result in infection. “In addition, several other organisms were isolated, which have pathogenic potential such as P. aeruginosa, Stenotrophomonas maltophilia, and Serratia marcescens but were not associated with infection in these cases.”
This suggests that colonization or presence of bacteria within a biofilm or on the surface of the plug or lacrimal stent is common but rarely pathogenic, the authors concluded. “Future studies could evaluate whether presence of a punctal plug or intracanalicular device could be a risk factor for infection when undergoing ophthalmic surgery.”
| Click here for journal source. |
Meyer JJ, Culbreath K, Ager E, et al. Evaluation of the microbiology of removed punctal plugs and intracanalicular devices. Eye Cont Lens. July 16, 2024. [Epub ahead of print.] |


