 |
|
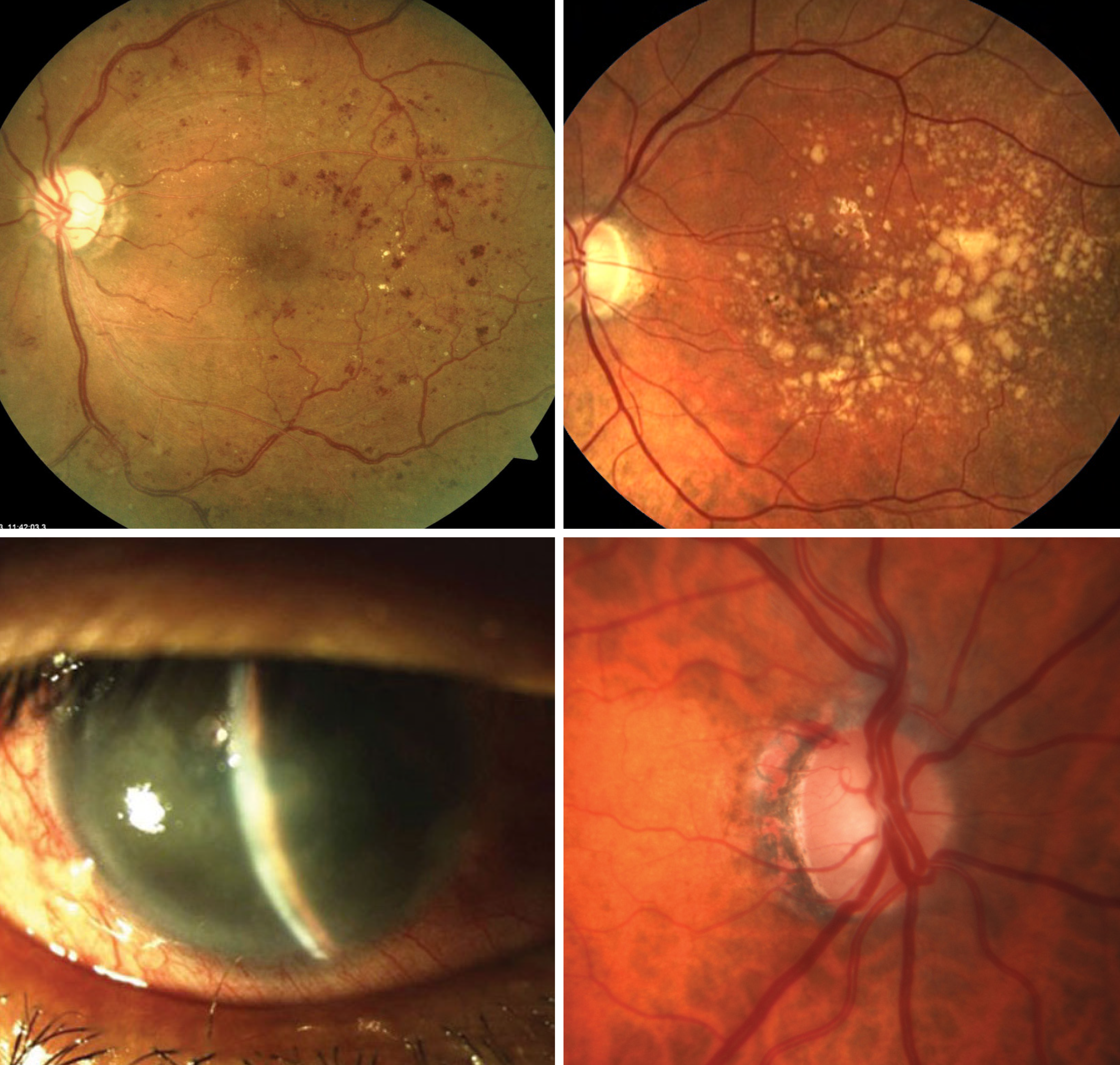
Lengthening of the eye in myopia development confers a protective effect against DR (upper left), AMD (upper right) and angle closure glaucoma (lower left) but elevates risk of open-angle glaucoma (lower right), in addition to increased risk of myopic macular degeneration and non-glaucomatous optic neuropathy. Photo: Mohammad Rafieetary, OD; NEI; Joseph Sowka, OD; Michael Chaglasian, OD. Click image to enlarge. |
The prevalence of myopia and vision impairment due to myopic macular degeneration and myopia-related optic neuropathies have increased throughout the world. In a study published last week in Ophthalmology, researchers evaluated whether myopia is associated with other ocular disorders in a positive or negative sense and found correlations with a lower prevalence of diabetic retinopathy (DR), age-related macular degeneration (AMD) and angle-closure glaucoma (ACG) and lower incidence of DR and AMD, while high myopia more than moderate myopia is associated with a higher prevalence and incidence of open-angle glaucoma (OAG).
The work comprised three large population-based studies: the Russian Ural Eye and Medical Study of 5,899 individuals, the Beijing Eye Study (4,439, all aged 40+ years) and the Central India Eye and Medical Study (4,711, aged 30+ years). The studies were conducted, respectively, in rural and urban regions in Bashkortostan, Russia; Beijing, China; and Nagpur, India. Axial length as a surrogate for myopia and prevalence of DR, AMD, ACG and OAG were all measured.
The odds ratio (OR) for prevalence of each of these conditions in the three populations were as follows:
| Russia | China | India |
DR | 0.73 | 0.33 | NA |
AMD | 0.85 | 0.83 | 0.81 |
ACG | 0.72 | NA | 0.55 |
OAG | 1.45 | 1.35 | 1.45 |
In all three studies, the association between higher OAG prevalence and longer axial length was nonlinear, with a slight increase for the moderate myopia range and a steep increase in the highly myopic range, the researchers wrote in their paper.
The study’s findings prompt the question: Why is a longer axial length associated with a lower prevalence of DR, AMD and ACG and with a lower incidence of DR and AMD while simultaneously related to a higher prevalence and incidence of OAG?
“Axial elongation-related changes in the region of the optic nerve head in highly myopic eyes with an axial length of more than 26.5mm include an elongation and thinning of the lamina cribrosa, an elongation and thinning of the peripapillary scleral flange with an increase in the distance between the peripapillary arterial circle of Zinn-Haller and the lamina cribrosa, and an increase in the distance between the retinal ganglion cell bodies in the retina and the optic disc, leading to a lengthening of the retinal nerve fibers,” the researchers wrote in their paper.
“Moderately myopic eyes show markedly less pronounced morphologic changes, such as an enlargement of parapapillary gamma zone in association with a misalignment between Bruch´s membrane opening and the lamina cribrosa,” the authors continued. “Interestingly, intraocular pressure increased with longer axial length in previous population-based studies. The basis for the associations between axial myopia and the prevalence of DR and AMD has also remained elusive so far.”
What is also interesting to the authors is that recent small-scale studies revealed a lower intraocular concentration of VEGF in axially myopic eyes with an axial elongation–related increase in intraocular volume.
“It may be discussed whether the larger depth of the anterior chamber in myopic eyes may be related with a lower prevalence of angle-closure glaucoma,” the researchers suggested in their paper. “In general, it may be recognized that causality for the associations has not been established yet. This may have implications for comparing and weighing the disadvantages of myopia and high myopia, such as OAG and myopic macular degeneration, against the myopia-related advantages of having less AMD, DR and ACG.”
Better understanding the causality of the associations of myopia with OAG, ACG, AMD and DR may be important, since if myopia control is implemented to control high myopia, it may or may not affect the other changes, the authors concluded.
Jonas JB, Bikbov MM, Kazakbaeva GM, et al. Positive and negative associations of myopia with ocular diseases in population-based studies. Ophthalmology. July 1, 2024. [Epub ahead of print.] |


