Comparing inner retinal measurements against a reference database is vital to diagnosing and monitoring certain pathologies, including primary eye conditions like optic neuropathies, as well as visual pathway lesions and systemic diseases. To improve the body of reference data, researchers from the University of New South Wales School of Optometry recently performed a study that used OCT to conduct measurements of the inner retina in a large sample of normal, healthy eyes. Furthermore, it assessed the association between various inner retinal measures, such as peripapillary RNFL, and physiological factors, demographics, non-ocular pathology and pharmaceutical drug use.
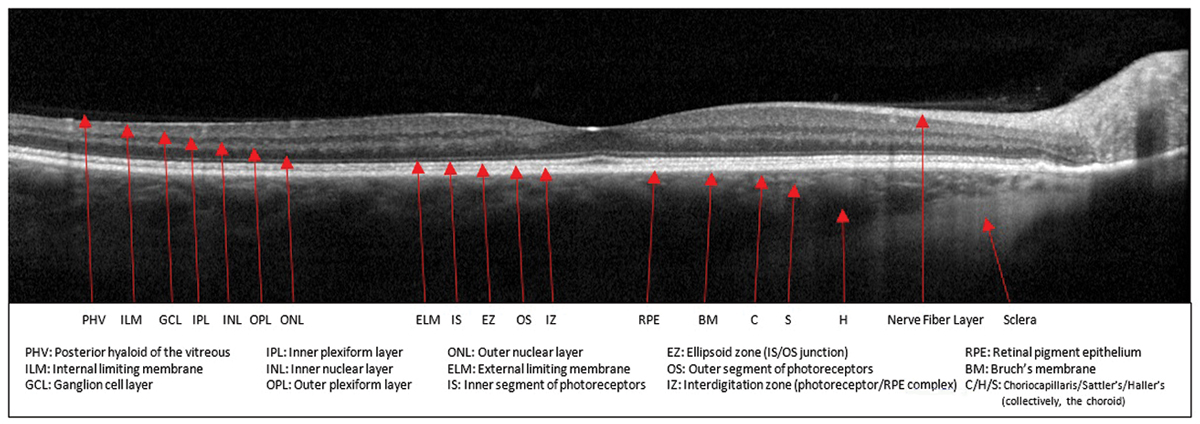 |
| A recent analysis found that certain systemic diseases and drugs were significantly associated with deviations in standard OCT inner retinal measures, underscoring the importance of considering systemic health when assessing OCT data to ensure accurate interpretations of normal vs. pathological inner retinal health. Photo: Sara Weidmayer, OD. Click image to enlarge. |
The study employed a retrospective, cross-sectional analysis of 705 consecutive participants with bilateral normal, healthy optic nerves and maculas. Mean age was 46.6 and 59.0% were women. One-third (33.1%) were white, 24.2% were Asian, 15.7% were categorized as “other” and 26.8% did not disclose their group. The mean refractive error was mildly myopic (-0.92D). The most prevalent non-ocular pathologies were hypertension (10.5%), migraine (7.2%) and asthma (5.4%), while the most prevalent pharmaceutical drugs were lipid-lowering agents (15.7%), ACE inhibitors (9.5%) and diabetes drugs (7.4%).
Data such as vertical cup/disc ratio, cup volume and macular ganglion cell layer-inner plexiform layer thicknesses were extracted from Cirrus OCT scans. These measures were then regressed against predictor variables that included participants' physiology, demographics, non-ocular pathology and pharmaceutical drug use following the World Health Organization classifications.
The results showed that several non-ocular pathologies and pharmaceutical drug uses were significantly associated with deviations in standard OCT inner retinal measures, which exceeded the impact of other factors like age and intraocular pressure. Specifically, the use of systemic corticosteroids or sex hormones/modulators and the presence of diseases like vasomotor or allergic rhinitis were linked to thinner inner retina and larger optic nerve cup measures. Conversely, antineoplastic agents and the presence of liver or urinary diseases were associated with thicker inner retina and smaller optic nerve cup measures.
“Relatively novel findings [of this study] included that the use of sex hormones/modulators were associated with compromised inner retinal integrity, while unspecified liver or urinary diseases and antineoplastic agents were associated with diffuse macular GCL-IPL thickening,” the researchers wrote in their paper on the study for Ophthalmic and Physiological Optics, adding that the magnitude of these associations far exceeded test-retest 95% limits of agreement.
The authors also point out that the factors associated with inner retinal measures on OCT—vasomotor/allergic rhinitis, unspecified liver or urinary diseases, systemic corticosteroids, sex hormones/ modulators and antineoplastic agents—are not uncommon, “which highlights the importance of considering systemic health during clinical assessments of inner retinal health,” they wrote.
Trinh M, OK, La M, Ly A. Linking physiology and demographics, non-ocular pathology and pharmaceutical drug use to standard OCT measures of the inner retina: The PPP project. Ophthalmic Physiol Opt. July 7, 2024. [Epub ahead of print]. |


