With over 30 years of development and practical experience to its credit, LASIK is highly predictable and successful. However, researchers continue to improve upon it, and the fairly recent development of topography-guided LASIK (TG-LASIK) tailors the ablation profile of the laser energy in hopes of correcting higher-order aberrations (HOAs) better than traditional procedure. Another advanced refractive surgery, small incision lenticule extraction (SMILE), is growing in popularity for its better preservation of corneal integrity. SMILE uses a femto laser to cut a lenticule of stromal tissue, which the surgeon removes through a small corneal incision.
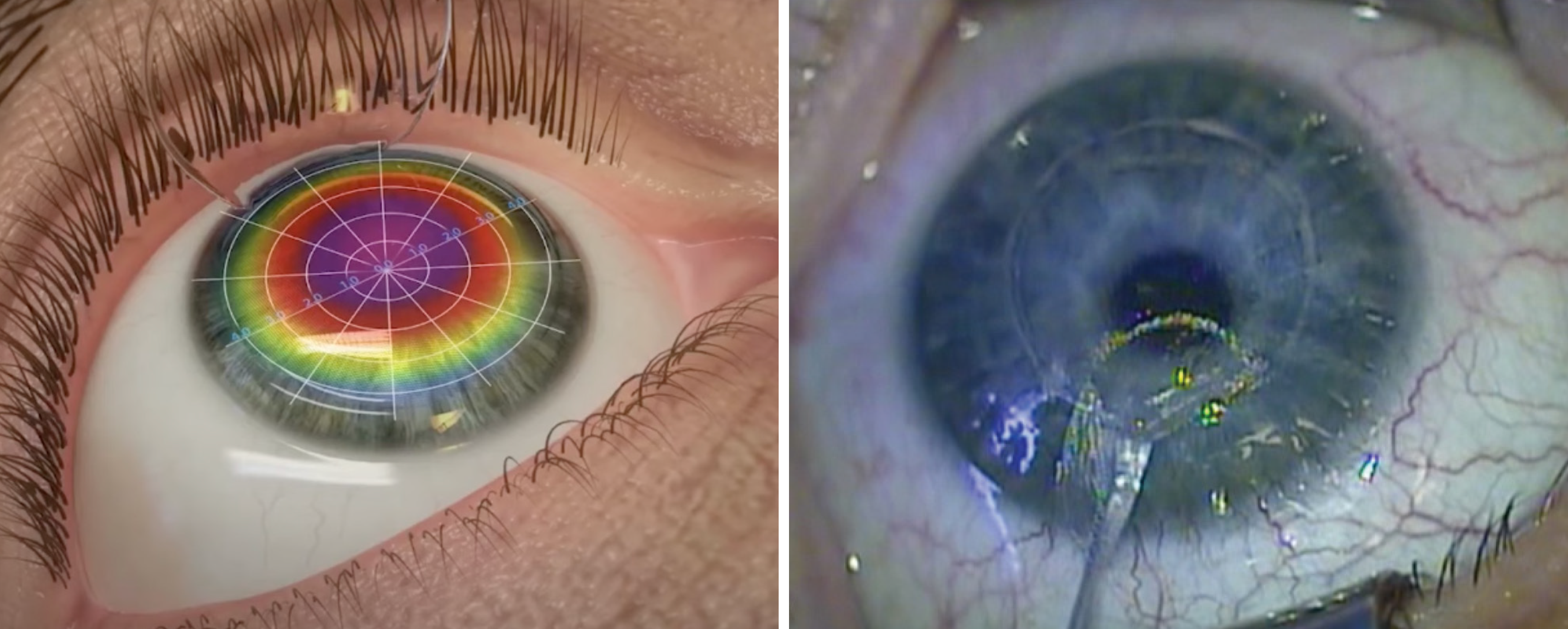 |
| TG-LASIK and SMILE may induce epithelial remodeling by changes in corneal curvature occurring from stromal ablation or lenticule extraction, inciting corneal epithelial cell migration from the limbus. Photo: Eye Mantra Hospital, India; Anders Ivarsen, MD, PhD, and Jesper Hjortdal, MD, PhD. Click image to enlarge. |
A new randomized, contralateral design study included 34 patients (68 eyes) who received TG-LASIK in one eye and SMILE in the fellow eye. Multiple parameters were compared preoperatively and up to three months post-op. Overall, comparable efficacy was seen at three months.
More specifically, TG-LASIK displayed faster visual recovery, as 63% and 89% of eyes achieved uncorrected distance visual acuity (UDVA) of 20/16 or better ate one day and one week, respectively. Comparatively, these rates were 34% at one day and 63% at one week for SMILE. Safety index at three months did not differ between the procedures. TG-LASIK totaled 44% and SMILE 56% of eyes within 0.13D of spherical equivalent target; however, SMILE induced more higher-order aberrations (HOAs), vertical coma and oblique trefoil than TG-LASIK at three months.
While both procedures displayed similar epithelial remodeling increases, SMILE was found to induce thicker epithelium at the 7.0mm nasal zonal area. Both procedures also affected corneal biomechanics similarly, with no differences found in corneal hysteresis or corneal resistance factor at three months. Also reported as not significantly different were symptoms of glare, halos, rings, starbursts and dry eye. At one-month post-op, 59% of patients preferred their eye treated with TG-LASIK, but no eye preference was described in 65% of patients at three months.
In the discussion section of their paper for Ophthalmology & Therapy, the study authors cite previous investigations that favor TG-LASIK in terms of efficacy. They explain that these observed differences in visual recovery rate could be due to higher energy levels being used in SMILE—lower energy levels, conversely, are associated with improved UDVA on post-op day one.
They also note that, originally, they expected TG-LASIK to reduce total HOAs, but this investigation showed significant increase in HOAs in both groups—totaling a 27% increase for TG-LASIK vs. 53% increase for SMILE—from preoperation to three months. This group of investigators also found that SMILE induced significantly more vertical coma than TG-LASIK. This may be due to TG-LASIK’s customized ablation treatment, which can reduce susceptibility to errors caused by pupil centroid shifts caused by changes in pupil size, ultimately improving correction of peripheral corneal irregularities. SMILE has also been shown to cause more vertical decentration than TG-LASIK—specifically around the area of lenticule extraction—which may contribute to higher amounts of vertical coma.
Addressing this issue, the authors relay that “with the introduction of newer SMILE platforms with added cyclotorsion and centration control,” the induced vertical coma seen with older platforms may improve,” they wrote.
Moin KA, Manion GN, Pandiri S, Hoopes PC. Three-month comprehensive outcomes of topography-guided LASIK vs. keratorefractive lenticule extraction (KLEx): a prospective contralateral study. Ophthalmol Ther. July 1, 2024. [Epub ahead of print]. |


