 |
|
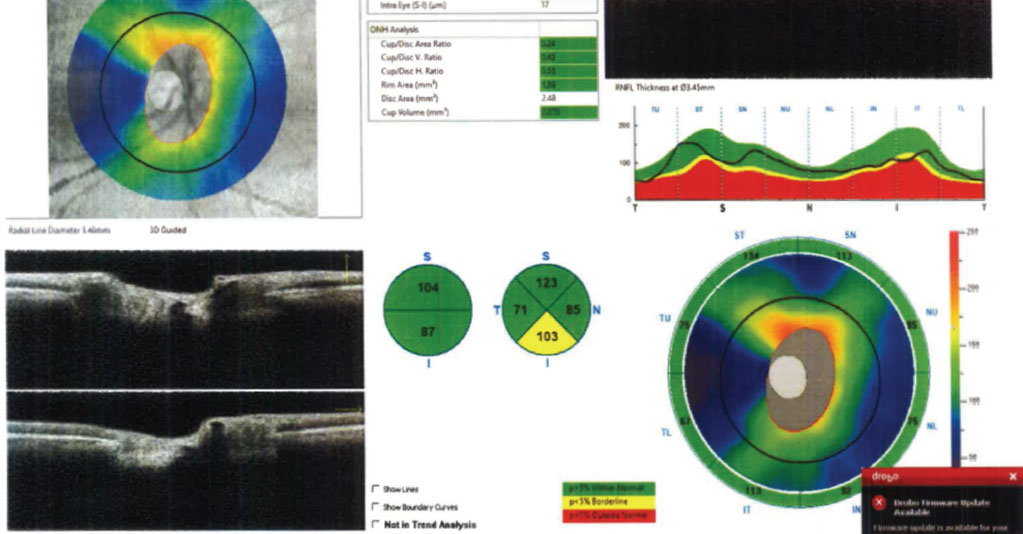
Regional and systemic vascular insufficiency may be independent and additive risk factors in the structural progression of NTG. Photo: Julia Reimold, OD, and Chris Wroten, OD. Click image to enlarge. |
Little is known about the nature of normal-tension glaucoma (NTG) when both systemic and ocular vascular dysregulation are present simultaneously. A recent study published in American Journal of Ophthalmology decided to identify the role that systemic arterial stiffness and choroidal microvascular insufficiency had on the structural progression of the condition. While the difference in the regional choroidal microcirculation was not reflected in the systemic arterial stiffness, the presence of both choroidal microvasculature dropout and abnormal systemic arterial stiffness led to significantly faster ganglion cell-inner plexiform layer (GCIPL) thinning in the macula but not the RNFL in the peripapillary area. The researchers believed that this may be associated with rapid glaucoma structural progression in eyes with low baseline intraocular pressure (IOP).
The retrospective cohort study included a total of 107 early NTG eyes of 88 patients, who underwent pulse wave velocity measurements and OCT-A at baseline were categorized depending on the presence of peripapillary choroidal microvasculature dropout and pulse wave velocity. The researchers then analyzed the differences in glaucomatous progression. Structural progression rates were determined using the trend-based analysis of cirrus OCT. The results revealed that 32 eyes displayed choroidal microvasculature dropout (62.7 years old, 53.6% male), and 70 eyes did not show any microvasculature dropout (59.9 years old, 53.3% male) at baseline. Patients were followed for 48.4 months, with an average of 9.3 completed examinations.
When the patients were further divided based on pulse wave velocity (high pulse wave velocity ≥ 1,400cm/s), those with choroidal microvasculature dropout and high pulse wave velocity showed significantly faster thinning in macular GCIPL. In comparison to those with low pulse wave velocity and no microvasculature dropout, eyes with high pulse wave velocity and microvasculature dropout in the peripapillary area were likely to show fast structural progression (≤-1.2µm/year) in the macular GCIPL by odds of 6.019.
“Our results suggest first and foremost that regional and systemic vascular insufficiency can exert an additive influence on NTG progression,” the study authors wrote in their paper. “The lack of difference in IOP-related parameters in the present study has also provided us with further evidence that there exists a subset of glaucoma in which IOP plays relatively less vital roles.”
Notably, when the researchers examined patients who were excluded from the present study on the basis of high IOP at baseline (> 21mm Hg), no pattern of association was noted between vascular insufficiency (whether it be microvasculature dropout or high pulse wave velocity measurement) and structural progression.
Lee JS, Bae HW, Kim CY, Lee SY. Systemic arterial stiffness and choroidal microvascular insufficiency on the structural progression of normal tension glaucoma. Am J Ophthalmol. July 6, 2024. [Epub ahead of print]. |


