 |
|
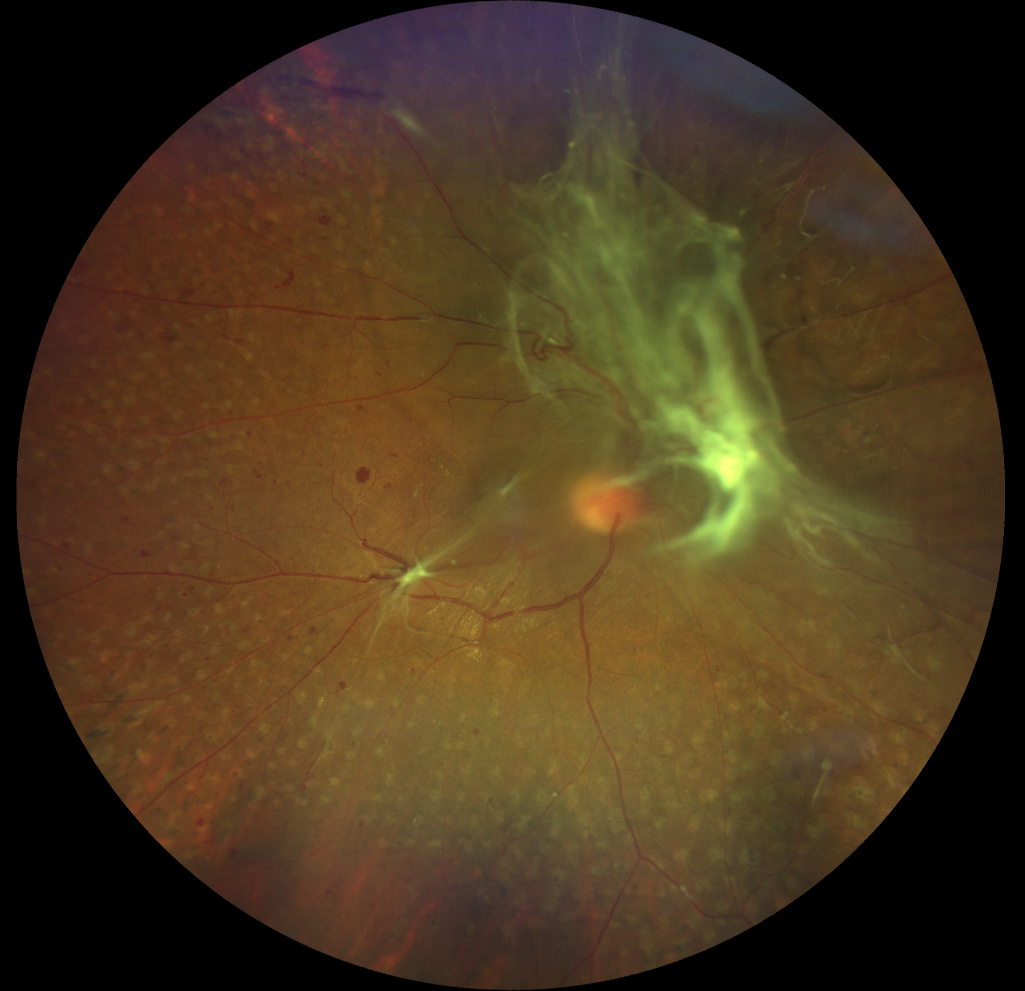
Greater access to routine eye care is unlikely to reduce incidence of corneal abrasion to the same extent as preventable eye emergencies like vitreous hemorrhage, thus making it more important to tackle any barriers to its emergency treatment like limited ED access. Photo:Carolyn Majcher, OD. Click image to enlarge. |
Emergency departments (EDs) are often stretched thin by those presenting with conditions which do not truly require immediate care. To parse out this discrepancy specifically in ocular emergencies, researchers compared sociodemographic factors in patients presenting to EDs with emergent and non-emergent eye-related concerns. Their results were published recently in American Journal of Ophthalmology.
The cross-sectional, multicenter study included a total of 60,677 patients who presented with eye-related concerns across several EDs: 37.0% from Bascom Palmer Eye Institute, 26.6% from Wills Eye Hospital, 25.5% from Massachusetts Eye and Ear and 10.9% from Wilmer Eye Institute. Including all cases seen during the course of one calendar year, 56.7% of these patients had non-emergent diagnoses.
Men were more likely than women to present emergently. An emergent diagnosis was less likely in those with insurance than without; patients with veteran/military insurance were equally likely to have an emergent diagnosis as uninsured patients. As well, Hispanic patients were more likely to present with an emergent diagnosis than white patients. Those who were seen in a standard ED setting were more likely to have emergent diagnoses than those visiting standalone eye facilities.
Most common emergent diagnoses included corneal abrasion (13.0%), extraocular foreign body (7.6%) and corneal ulcer (7.1%); most common non-emergent diagnoses were dry eye (7.9%), posterior vitreous detachment (7.8%) and chalazion (6.6%).
In their discussion, the study authors discuss potential reasons for their findings. Those without insurance likely are affected by lack of longitudinal care in those with chronic ophthalmic diseases, thus predisposing them to acute complications warranting emergency services. As well, those uninsured may wait until symptoms become severe or they experience an eye emergency to seek ophthalmic care. In this regard, the study researchers suggest “interventions that bolster access to and continuity of insurance coverage for vulnerable patients (e.g. uninsured and non-white Hispanic patients) may reduce the incidence of eye emergencies consequent to poorly managed chronic ophthalmic diseases.”
A top presenting diagnosis was vitreous hemorrhage, often a complication of proliferative diabetic retinopathy, which is also known to disproportionately affect Hispanic patients, likely for the same reasons. Reducing ED overload may be possible by providing greater access to routine eye care, which would decrease incidence of preventable vitreous hemorrhage. What’s more, Hispanic patients with diabetic retinopathy face additional barriers to care even after controlling for insurance status and education, such as inability to find childcare, limited English proficiency, health literacy challenges and difficulty finding physicians of similar ethnic background. These obstacles might contribute to the greater proportion of Hispanic patients at higher risk of developing serious complications of diabetic retinopathy like vitreous hemorrhage.
The authors recommend here that “interventions that tackle social determinants of health (e.g. improved child care resources, translation services and patient education) for Hispanic patients may have downstream effects on preventable eye emergencies in the ED.”
Otherwise, the authors also weigh in on the aspect of ED settings, offering that “standalone eye EDs may have sufficient resources to treat non-urgent conditions without detracting from more pressing eyecare needs; yet they may hold greater potential for resource optimization given the higher rates of non-urgent use shown in our analyses. On the other hand, redirecting non-urgent eye cases may be a more essential and clinically impactful intervention in standard EDs, which often suffer from resource constraints.”
Quintero M, Mahjoub H, Ssekasanvu J, et al. Sociodemographic factors associated with emergent eye-related emergency department visits: a multicenter analysis. Am J Ophthalmol. July 5, 2024. [Epub ahead of print]. |


