 |
|
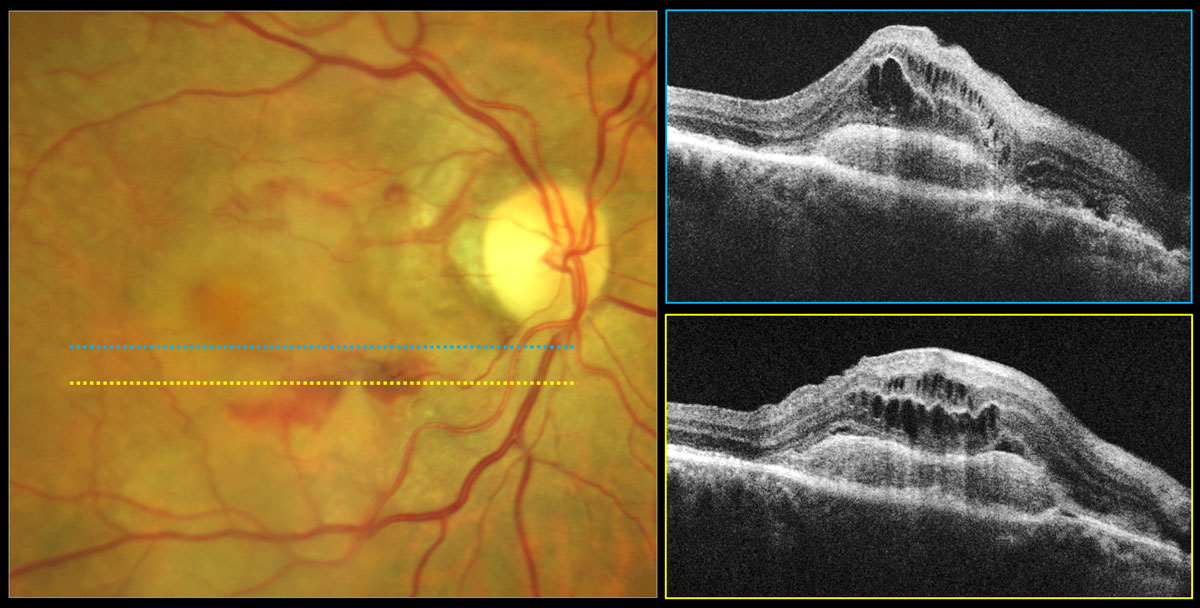
Much of the cost of late-stage AMD was either productivity costs (i.e., patients and their caregivers were unable to work) or the value of patients’ loss of quality of well-being. Photo: Carolyn Majcher, OD. Click image to enlarge. |
Understanding the comprehensive economic effects of age-related macular degeneration (AMD) could aid with decision-making in health care policy, economic planning, health technology assessments, medical research and public health initiatives, potentially leading to better health outcomes and more efficient use of resources. Despite the considerable deleterious effect AMD can have on visual function, it can be associated with adverse economic outcomes that can extend beyond the direct medical costs associated with treatment. People living with AMD often require additional support, including caregiving services, vision aids and rehabilitation, further escalating this burden.
A recent study published in JAMA Ophthalmology estimated the annual total burden of late-stage AMD, including wet AMD and geographic atrophy (GA), in Bulgaria, Germany and the United States to evaluate the toll of late-stage AMD in countries with diverse health care systems, access hurdles, socioeconomic statuses and cultural traits. The researchers found that late-stage AMD imposes a substantial economic burden akin to other common non-life-threatening diseases, such as Parkinson disease and obesity.1
The study used the prevalence approach cost-of-illness economic modeling to estimate costs attributable to late-stage AMD. Participants older than 50 years residing in Bulgaria, Germany and the US who were diagnosed with late-stage AMD (wet AMD or any form of GA) in one or both eyes and caregivers who care for those diagnosed with late-stage AMD were recruited through ophthalmological clinics in Bulgaria and Germany and via online newsletters and social media in the US. The patient survey covered questions in relation to health care utilization, self-reported vision health, emotional well-being, productivity and association with activities of daily living. The caregiver survey assessed the association of caregiving responsibilities with productivity, emotional well-being and activities of daily living.
Of the 128 individuals with late-stage AMD in this study, 62% were female, and 94% were aged 60 years or older. Of the 61 caregivers, 70% were female and 91% were aged 45 years or older. Cost data for clinical examinations, prescriptions, and medical devices were obtained from public sources and clinician interviews. When public data were unavailable, subscription databases were used and validated with clinicians.
Estimated per-annum total costs attributable to late-stage AMD were €449.5 million ($512.5 million) in Bulgaria, €7.6 billion ($8.6 billion) in Germany and €43.2 billion ($49.4 billion) in the US. Across all countries, 10% to 13% of the total cost incurred was attributed to direct medical costs. In Germany and Bulgaria, the biggest contributor to the total economic burden was reduced well-being (67% and 76%, respectively), whereas in the US, loss of productivity (42%) was the biggest contributor.
The researchers suggested that this may signify a greater impact of the disease in the working-age population in the US compared to the other countries studied. They observed higher direct medical costs for wet AMD compared with GA across all countries. They found this reasonable given the fact that several treatment options were available for wet AMD but not for GA at the time of conducting this research.
“Raising awareness and improving early detection and access to vision rehabilitation services could help mitigate some of the indirect costs imposed by vision loss due to late-stage AMD,” they concluded. “Access to current and future therapies for late-stage AMD, including both neovascular AMD and GA, holds promise for reducing the projected increase in AMD burden amid global aging populations.”1
A commentary also published in JAMA Ophthalmology thought that “the study authors should be commended for looking at the total societal costs of AMD across three countries, particularly using a survey that included not only people living with AMD but also their caregivers.”2
Nevertheless, the commentary authors noted that there was little description of the patients who completed the surveys and that readers should be cautious in making intercountry comparisons, as the design and sample size may be insufficient to permit such comparisons.
“The authors also took the assessments of anxiety, depression, falls, and nursing home admissions observed in the survey of this population and assumed that if these patients did not have late-stage AMD, they would not have these conditions, which may overestimate the burden of AMD,” they wrote.
Still, they emphasized that, considering the value of interventions to address vision-threatening disorders like AMD, it is important to include costs like productivity and the value of quality of life, in addition to direct medical costs.
The commentary stressed that “more research on this topic is needed, such as studies with larger sample sizes, evaluating patients residing in more countries, considering unilateral vs. bilateral disease, evaluating other conditions and improving methods (such as valuing quality of life) to get a better, more complete picture of the costs of vision-threatening conditions.”2
| Click here for journal source. |
Paudel N, Brady L, Stratieva P, et al. Economic burden of late-stage age-related macular degeneration in Bulgaria, Germany and the US. JAMA Ophthalmol. October 31, 2024. [Epub ahead of print]. |


