 |
|
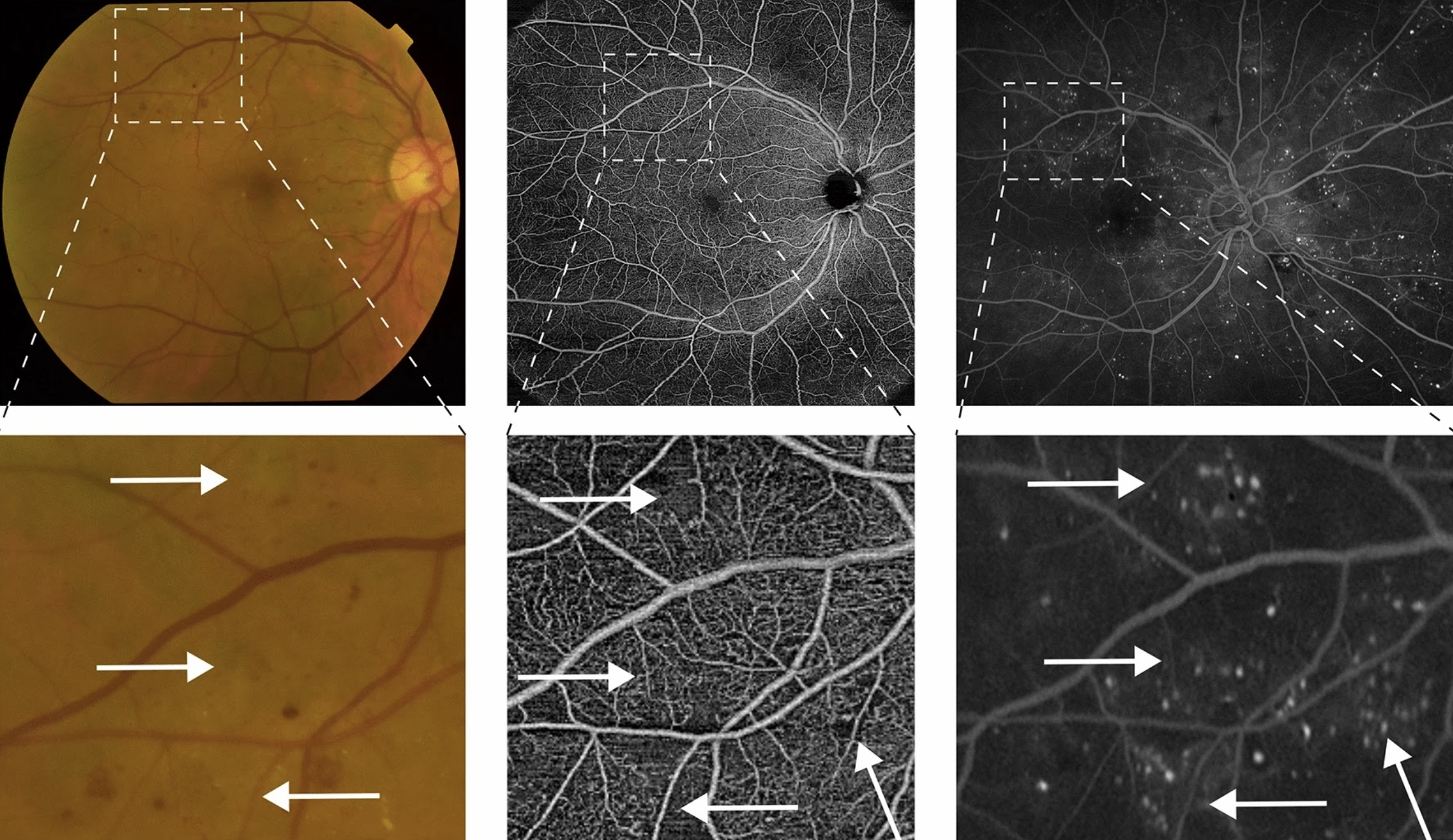
Development of IRMA appears to be associated with the hyperperfusion stage of non-proliferative DR and may be the hallmark of this angiogenic response to the progressive ischemia. This image from the paper shows identification of IRMA in the different modalities used (fundus photography, OCT-A and ultra-widefield fluorescein angiography). Images are shown with different magnifications to compensate for different field of view. Photo: Santos AR, et al. Ophthalmol Ther. October 26, 2024. Click image to enlarge. |
Doctors looking to assess proliferative diabetic retinopathy (PDR) risk in a diabetes patient with the nonproliferative form (NPDR) typically look to identify and quantify a variety of retinal irregularities associated with progression to that stage. Specifically, tortuous intraretinal vascular segments, also known as intraretinal microvascular abnormalities (IRMA), are a risk factor for conversion.
A new study appearing in Ophthalmology and Therapy was conducted with the aim to evaluate the prognostic value of IRMA in patients with NPDR, focusing on central retina (up to 50°), as well as to determine possible correlations between IRMA and other structural changes like ischemia or microaneurysm development. To analyze this, the study included 60 eyes of 60 patients with type 2 diabetes and who had moderate-to-severe NPDR. IRMA was defined as capillary tortuosity covering a minimum circular area of 300μm, imaged with a combination of fundus photography, ultra-widefield fluorescein angiography and swept-source OCT angiography. Both the central macula (up to 20°) and posterior pole (between 20° and 50°) of the retina were examined.
Evidence of IRMA was found in eyes with worse NPDR severity; in milder NPDR, the finding was only detected outside the central macula (>20°). What’s more, IRMA presence was positively associated with microaneurysm presence. As the researchers explain in their paper, this “needs to be examined further to see how peripheral lesions are relevant to identify eyes at highest risk of progression.”
After considering the performance of the different imaging modalities, the team concluded that IRMA identification in eyes with advanced NPDR is better achieved through use of ultra-widefield fundus fluorescein angiography, even in those with more mild findings. Also, when using OCT angiography, IRMA was only identified in the superficial capillary plexus, which may help explain the microvascular disease progression in DR. As they elaborated in their paper, microvascular alterations seem to start in this structure with localized capillary dropout areas, then progressing later with increased involvement of the deep capillary plexus and progressively extending from center to periphery.
When considering their findings’ clinical relevance, the authors believe IRMA is a good indication of the retinal hyperperfusion response to the progressive hypoperfusion characterizing initial stages of DR.
“This observation suggests a clear need to identify and characterize the presence of IRMA in diabetic retina to monitor the disease progression. In addition, microaneurysm quantification appears to be a useful surrogate for the presence and degree of severity of IRMA,” they concluded.
| Click here for journal source. |
Santos AR, Lopes M, Santos T, et al. Intraretinal microvascular abnormalities in eyes with advanced stages of nonproliferative diabetic retinopathy: comparison between UWF-FFA, CFP, and OCTA—The RICHARD Study. Ophthalmol Ther. October 26, 2024. [Epub ahead of print]. |


